Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
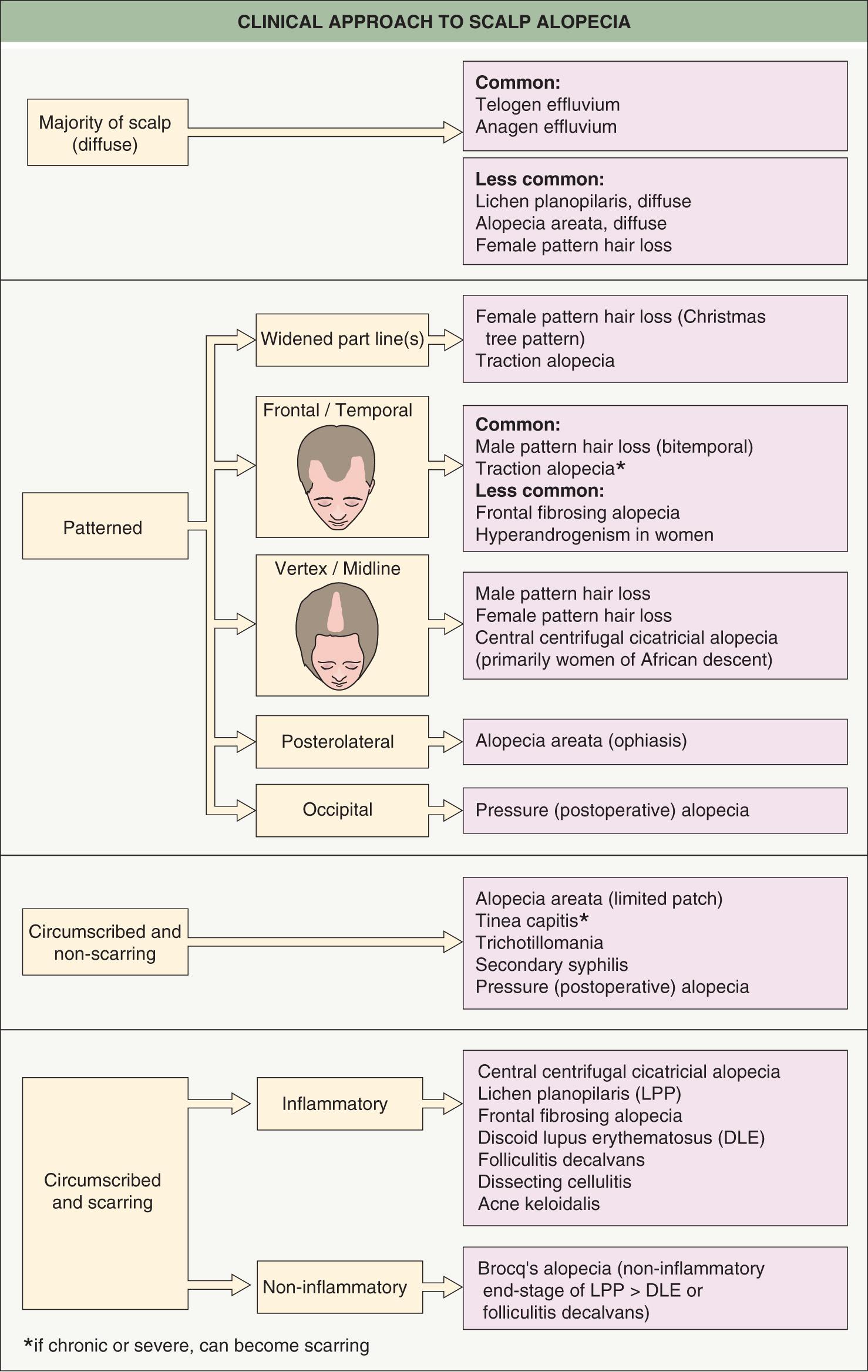
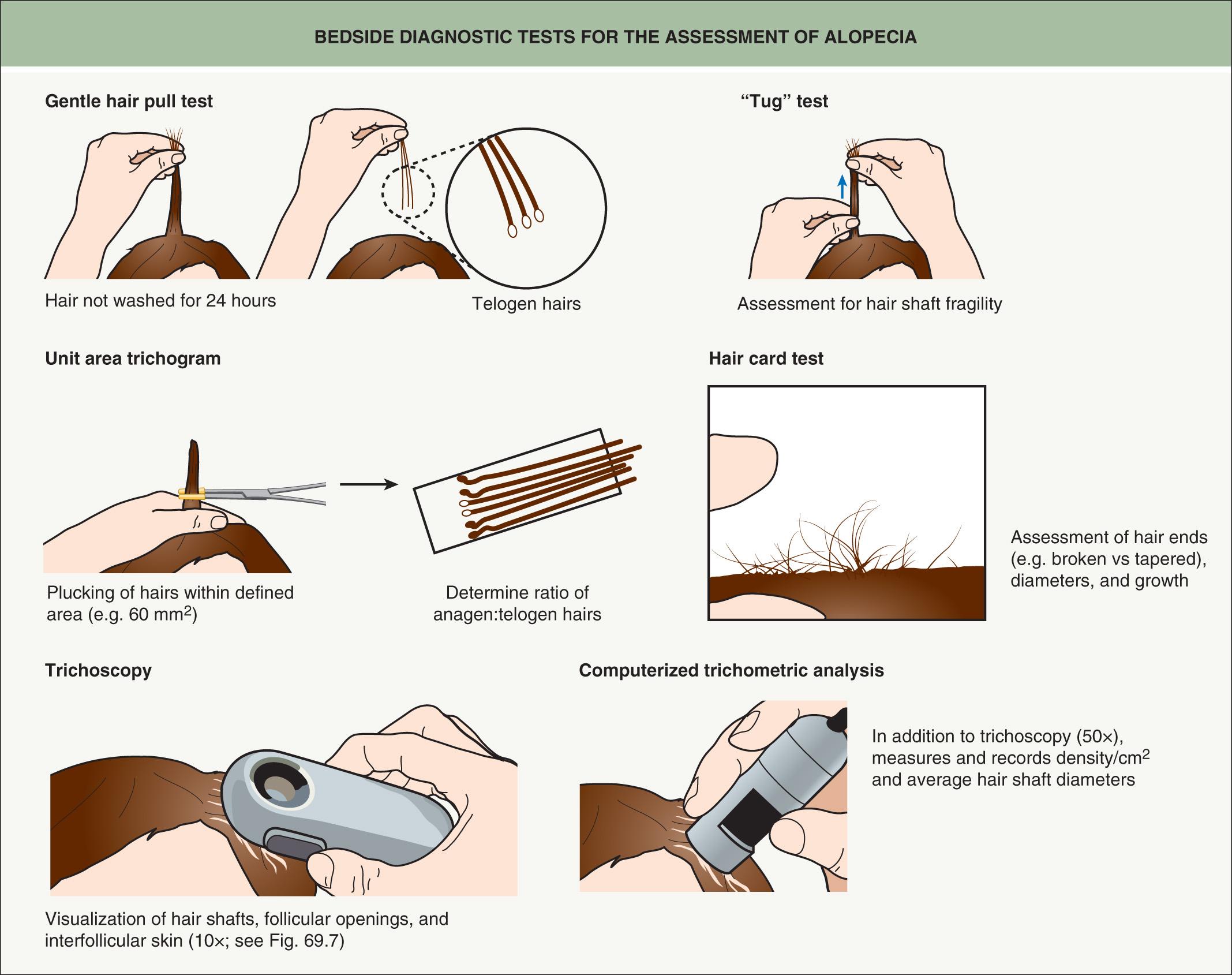
In this chapter, the major non-cicatricial (non-permanent) alopecias will be reviewed first, followed by a discussion of cicatricial alopecias and a review of structural hair shaft abnormalities. Chapter 68 reviews the structure and function of the hair follicle as well as regulation of the hair cycle. Table 69.1 outlines the historical information of importance in the evaluation of alopecias while Figs 69.1 and 69.2 depict a clinical approach and the diagnostic tests that can be performed in addition to the clinical examination. The decision to perform scalp biopsies, hair shaft analysis, and blood tests is guided by the differential diagnosis.
| CLINICAL ASSESSMENT OF ALOPECIA |
| The clinical history should be directed toward establishing the diagnosis, detecting precipitating factors where relevant, identifying associated comorbidities, and obtaining information pertinent to the proposed treatment |
| Establishing the diagnosis and detecting precipitating factors |
|
| Identifying associated comorbidities |
|
| Obtaining information pertinent to the proposed treatment |
|
▪ Male pattern and female pattern hair loss (MPHL and FPHL) ▪ Common balding ▪ Hereditary balding or thinning
Genetically determined sensitivity of scalp hair follicles to adult levels of androgens
Miniaturization of hairs in a symmetric “pattern” on the crown, vertex, and frontal regions
Antiandrogen medications can be used for successful treatment
Androgenetic alopecia (AGA) is an androgen-dependent, hereditary physical trait resulting from the conversion of scalp terminal hairs into miniaturized vellus hairs in a characteristic pattern. The frequency and severity increase with age, and at least 80% of Caucasian men and ~50% of women show evidence of AGA by age 70 years .
High concordance of MPHL amongst monozygotic twins indicates a strong genetic predisposition. The inheritance is polygenic and a number of genetic loci have been implicated, including those that encode the androgen receptor (MPHL; see Ch 157 ), estrogen receptor-β (FPHL), and the aromatase which converts testosterone to estradiol (FPHL) . Androgens clearly initiate and promulgate MPHL in genetically susceptible individuals, and while inhibition of androgen biosynthesis or action will arrest the progression of MPHL, this will only partially reverse the hair miniaturization. Additional implicated genes in MPHL include those that encode histone deacetylases (HDAC) 4 and 9 and the WNT molecule WNT10A . The WNT signaling pathway is known to play a key role in hair follicle development (see Ch. 68 ).
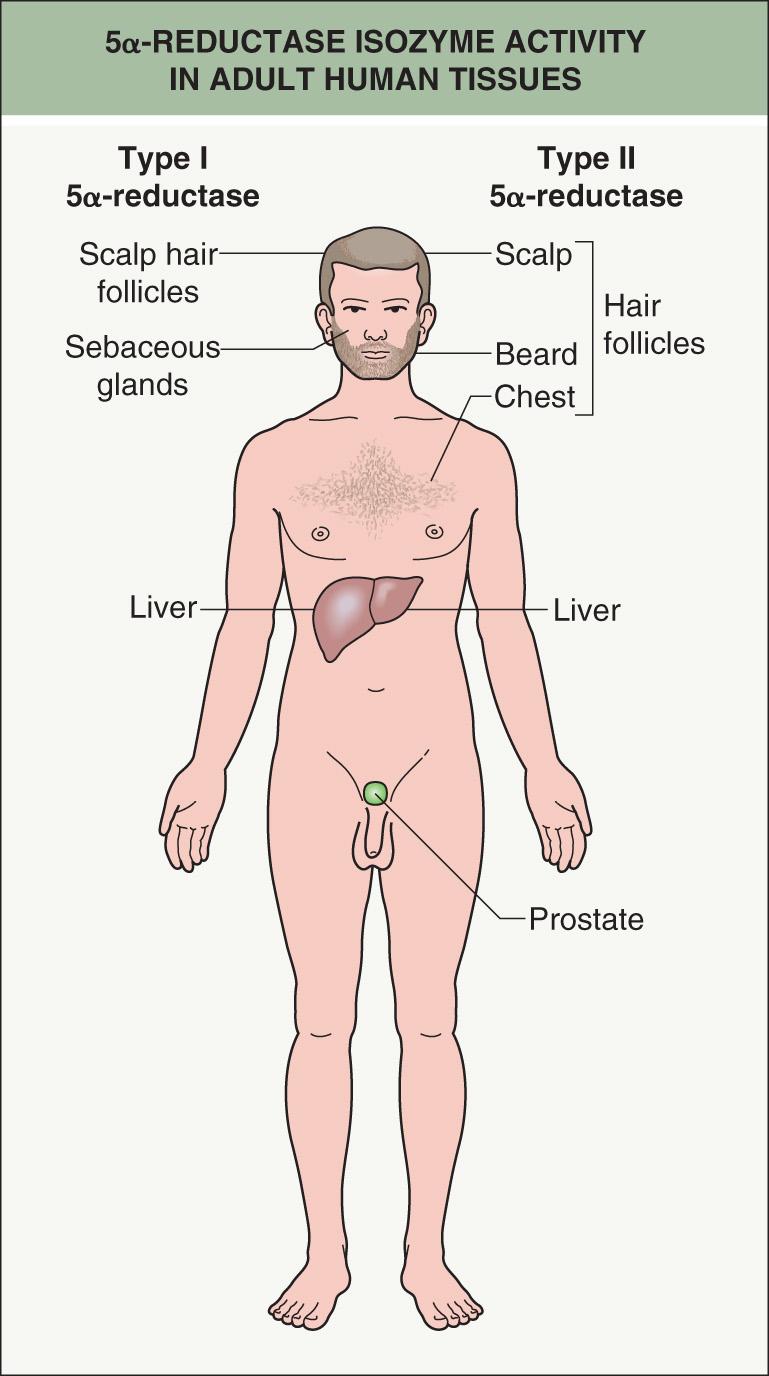
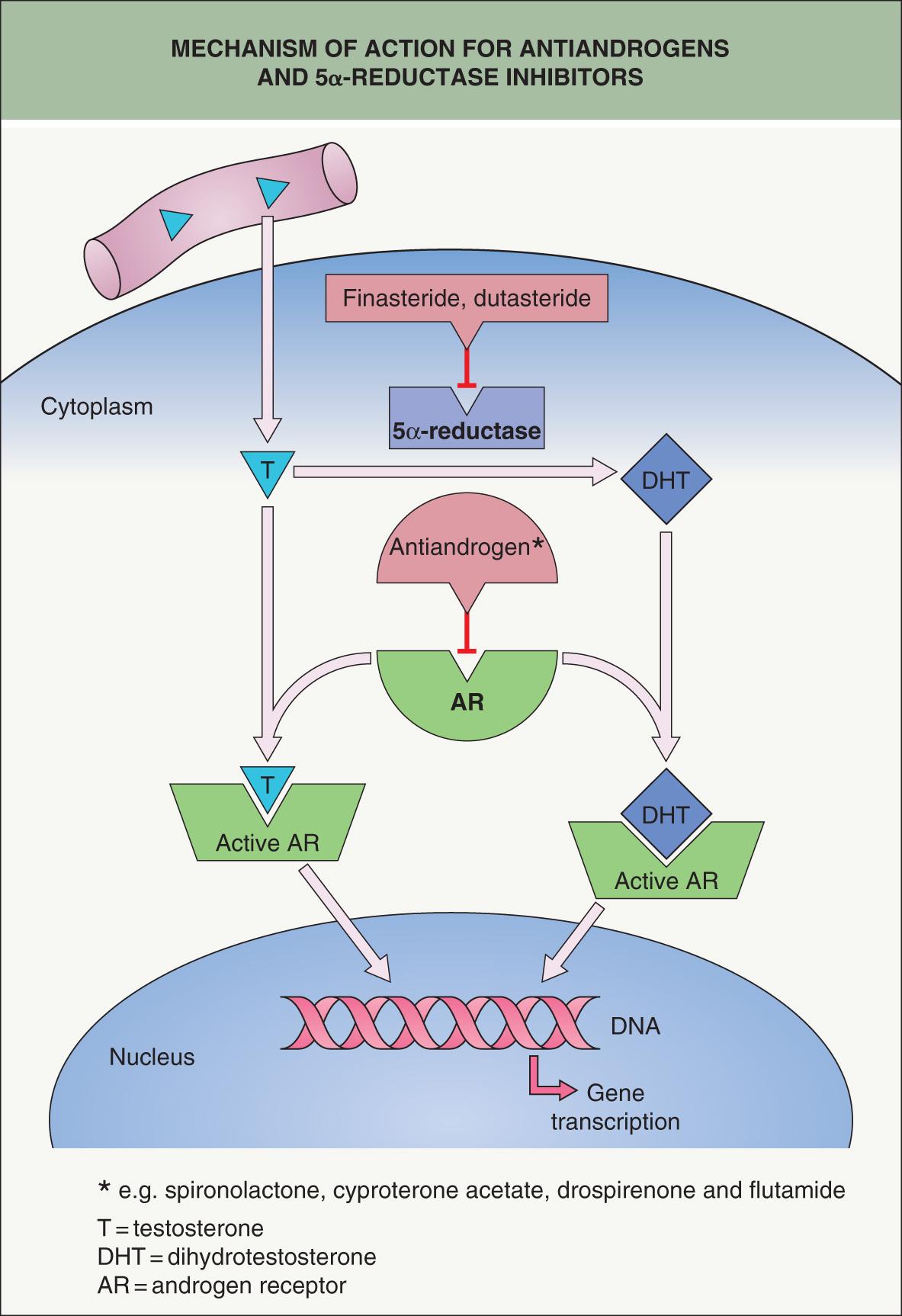
In men, the expression of AGA is specifically related to the androgen hormone dihydrotestosterone (DHT). Testosterone is converted to DHT by the enzyme 5α-reductase, of which there are three isoenzymes (types I, II, and III); the latter are encoded by separate genes and differ in their expression and activity in various tissues. For example, Type I 5α-reductase is present predominantly in sebaceous glands and the liver, whereas type II 5α-reductase dominates in scalp, beard and chest hair follicles, as well as in the liver and the prostate ( Fig. 69.3 ). Type III is found throughout the epidermis and dermis, but its functional role has yet to be elucidated. Of note, the genetic absence of type II 5α-reductase prevents development of male AGA.
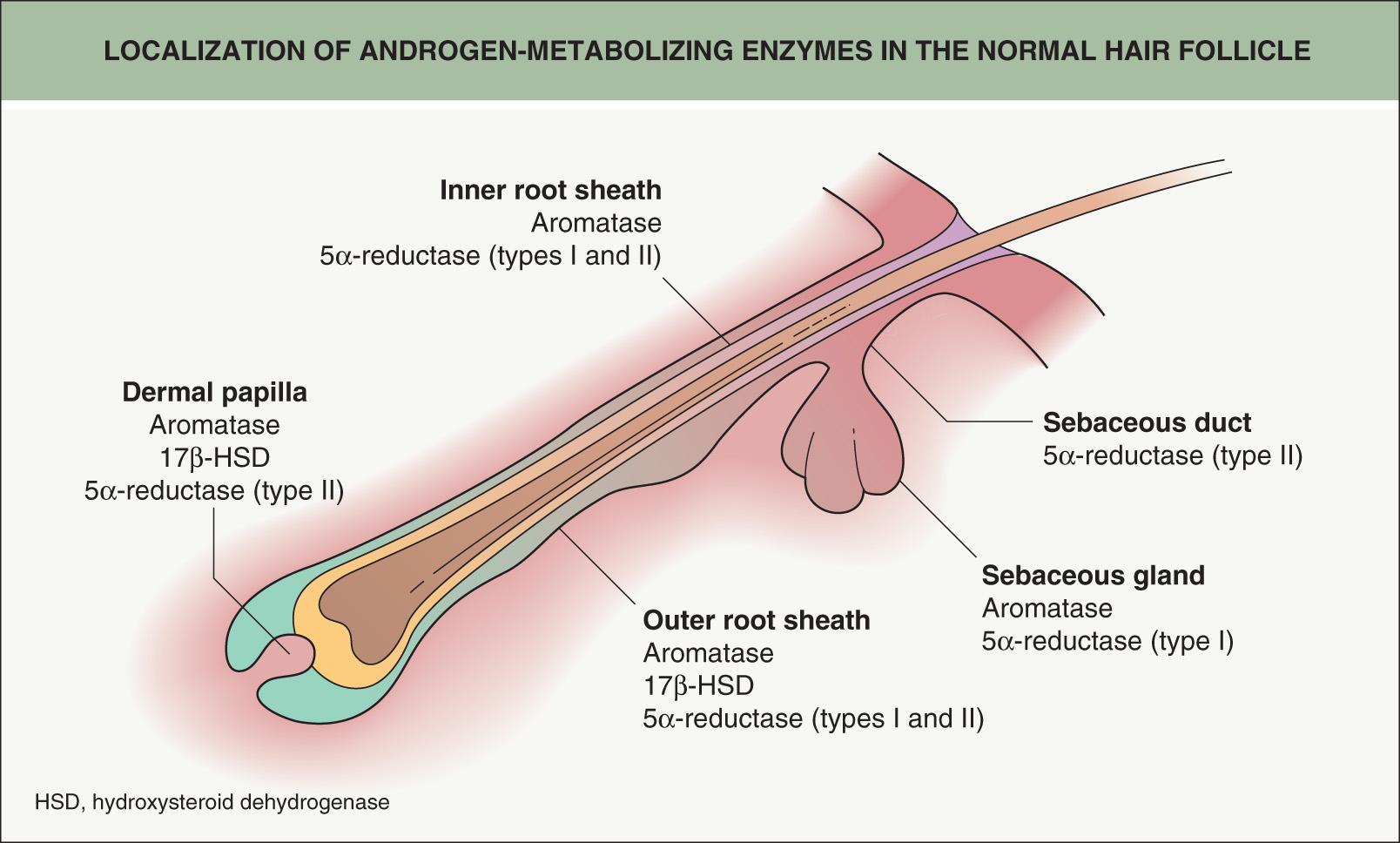
Investigators have localized androgen-metabolizing enzymes to various regions of the hair follicle ( Fig. 69.4 ). In scalp biopsy specimens obtained from men with AGA, 5α-reductase activity and DHT levels are increased compared to non-balding scalp skin . DHT is implicated in the appearance of miniaturized hair follicles and hair shafts, and decreased levels in both the skin and the blood have been associated with a reversal of miniaturization.
In women, a similar androgen-related pathophysiology is postulated . Women who develop balding shortly after puberty often have a positive family history for pattern hair loss in both male and female family members. In women who develop pattern alopecia during the perimenopausal period and menopause, it may be due to a genetic predisposition as well as alterations in androgen metabolism at the level of the hair follicle and systemic hormonal changes .
Rarely, AGA develops in prepubertal children (ages 6–10 years) . Affected boys and girls demonstrate a FPHL pattern without bitemporal recession, and they have a strong family history of AGA (present in at least one parent). No evidence has been found for abnormal circulating testosterone levels or precocious puberty.
Utilizing gene expression arrays of scalp biopsies from men with AGA, enhanced expression of the gene that encodes prostaglandin D2 synthetase was observed in bald scalp as compared to haired scalp ; prostaglandin D2 synthetase converts prostaglandin H2 (PGH2) to PGD2. Increased levels of PGD2 were also found in balding scalp, and in explants of human hair follicles, PGD2 was shown to inhibit hair growth. This inhibition of hair growth by PGD2 required interactions with one of its receptors, raising the possibility of a potential therapeutic target.
MPHL is symmetric and progressive with some pattern variation. Hamilton and then Norwood first classified the patterns of male AGA based upon frontoparietal and frontal recession as well as vertex thinning (see Fig. 157.2 ). Occasionally, a “male type” pattern with frontotemporal and vertex thinning is seen in women, and then they too can be classified with the Hamilton or Norwood system.
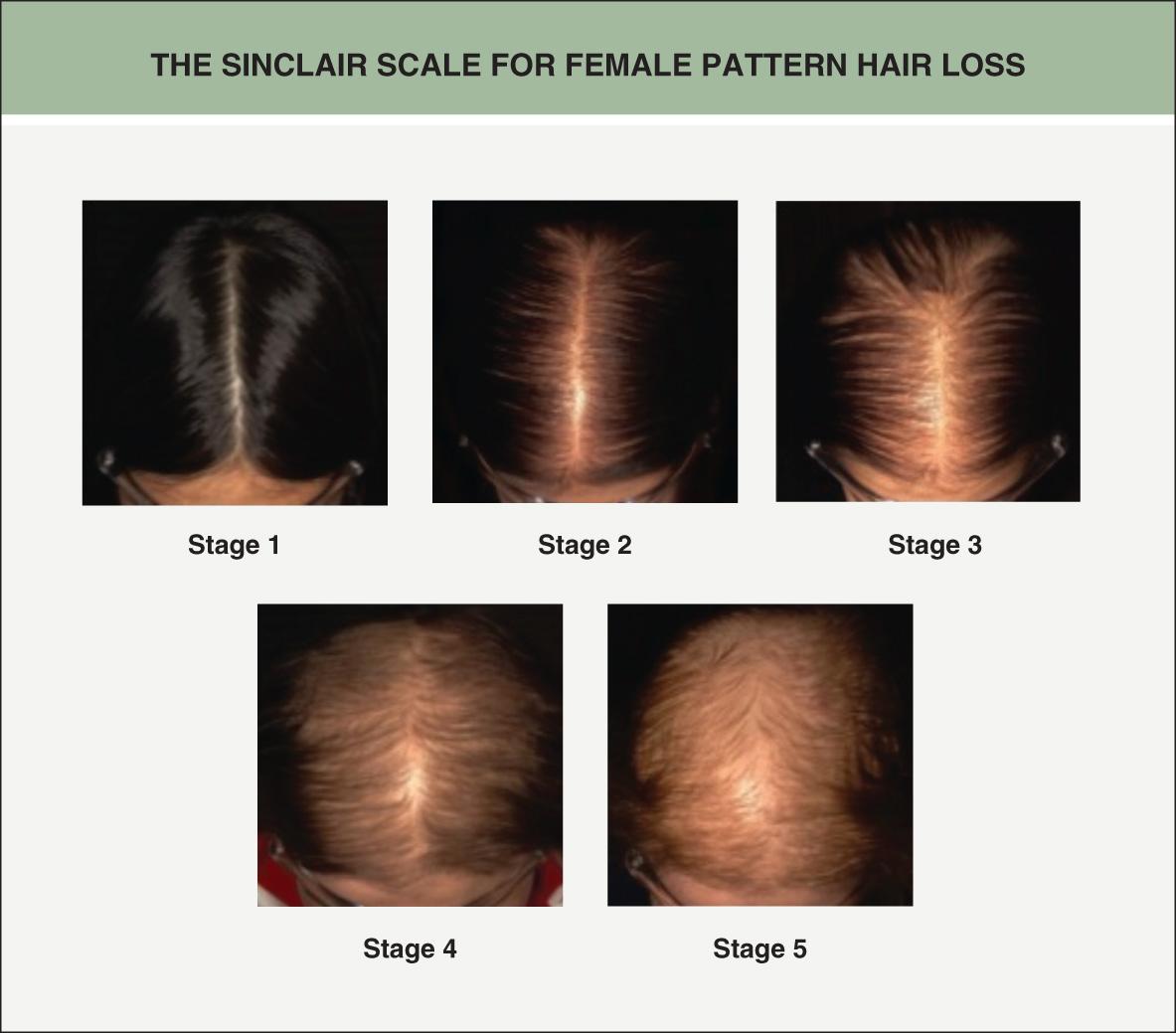
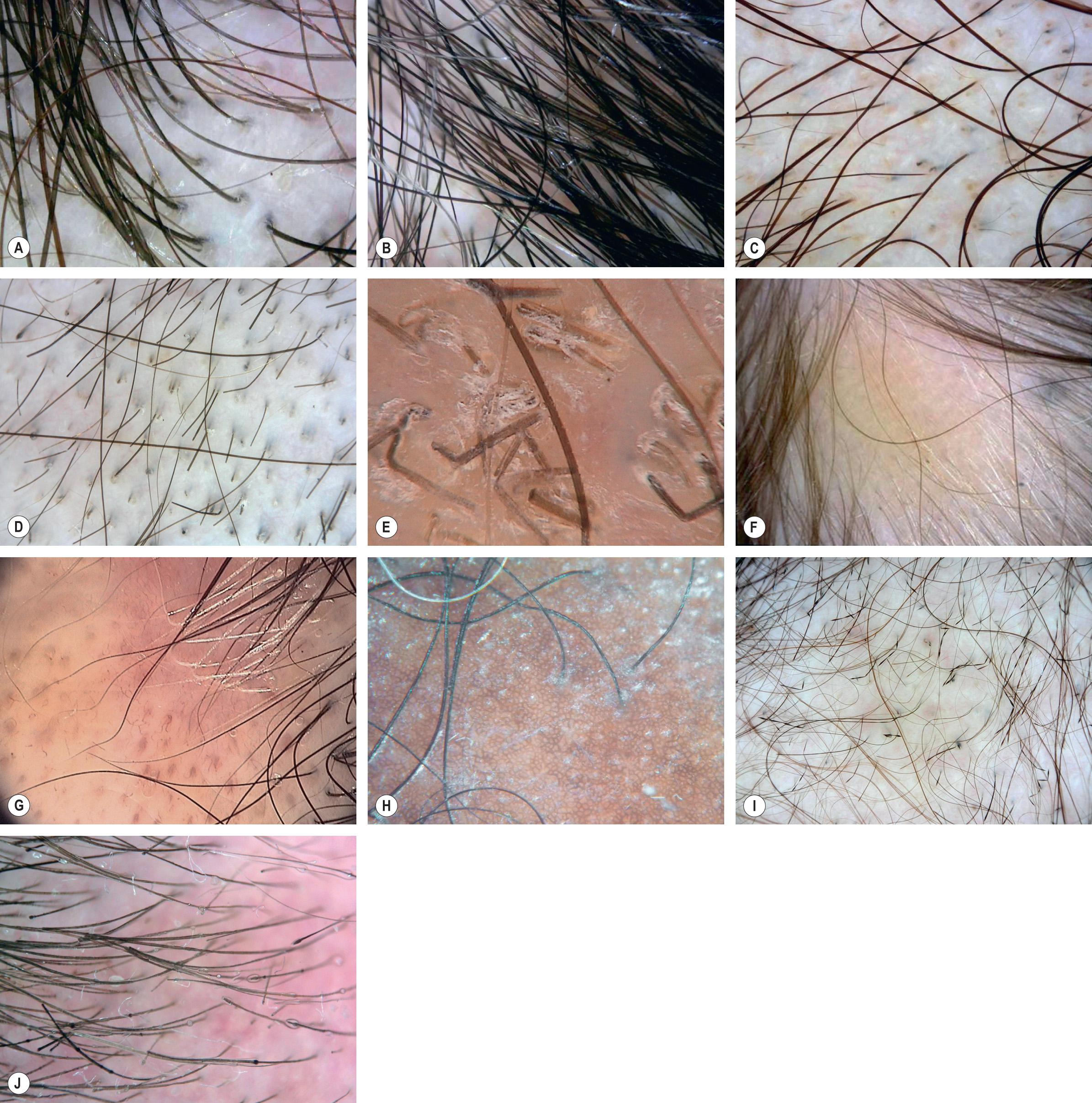
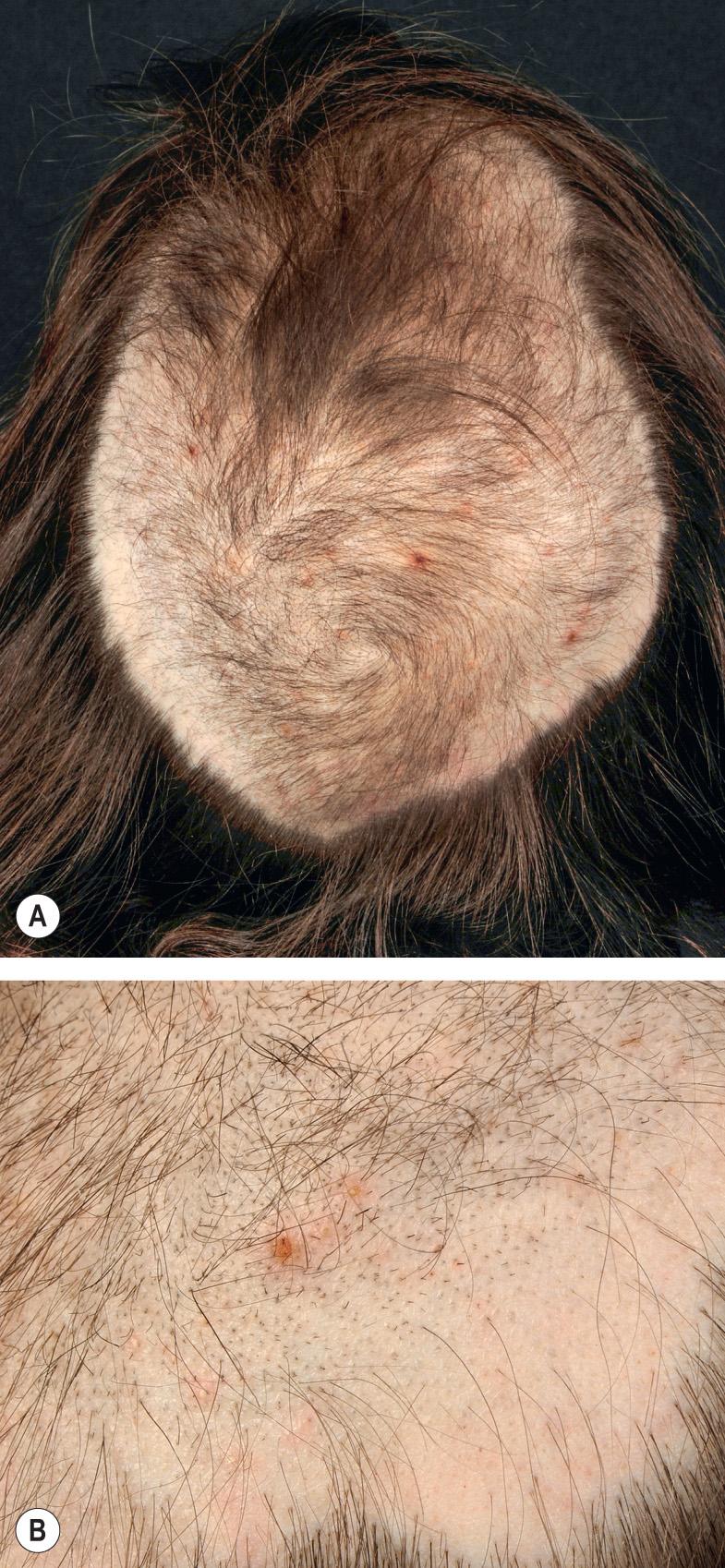
However, the most common pattern of FPHL is diffuse central thinning of the crown with preservation of the frontal hairline which can be assessed by the Ludwig grading scale (see Fig. 157.3 ). Often there is frontal accentuation of the hair loss, creating a “Christmas tree” pattern . Examination of the central part width can also be used to classify the severity of FPHL via the Sinclair scale ( Fig. 69.5 ) and it can be compared to the occipital part width ( Fig. 69.6 ) . The findings by trichoscopy are shown in Fig. 69.7 . A history of increased hair shedding may precede the clinical appearance of central thinning, but this is not specific for FPHL (see below).

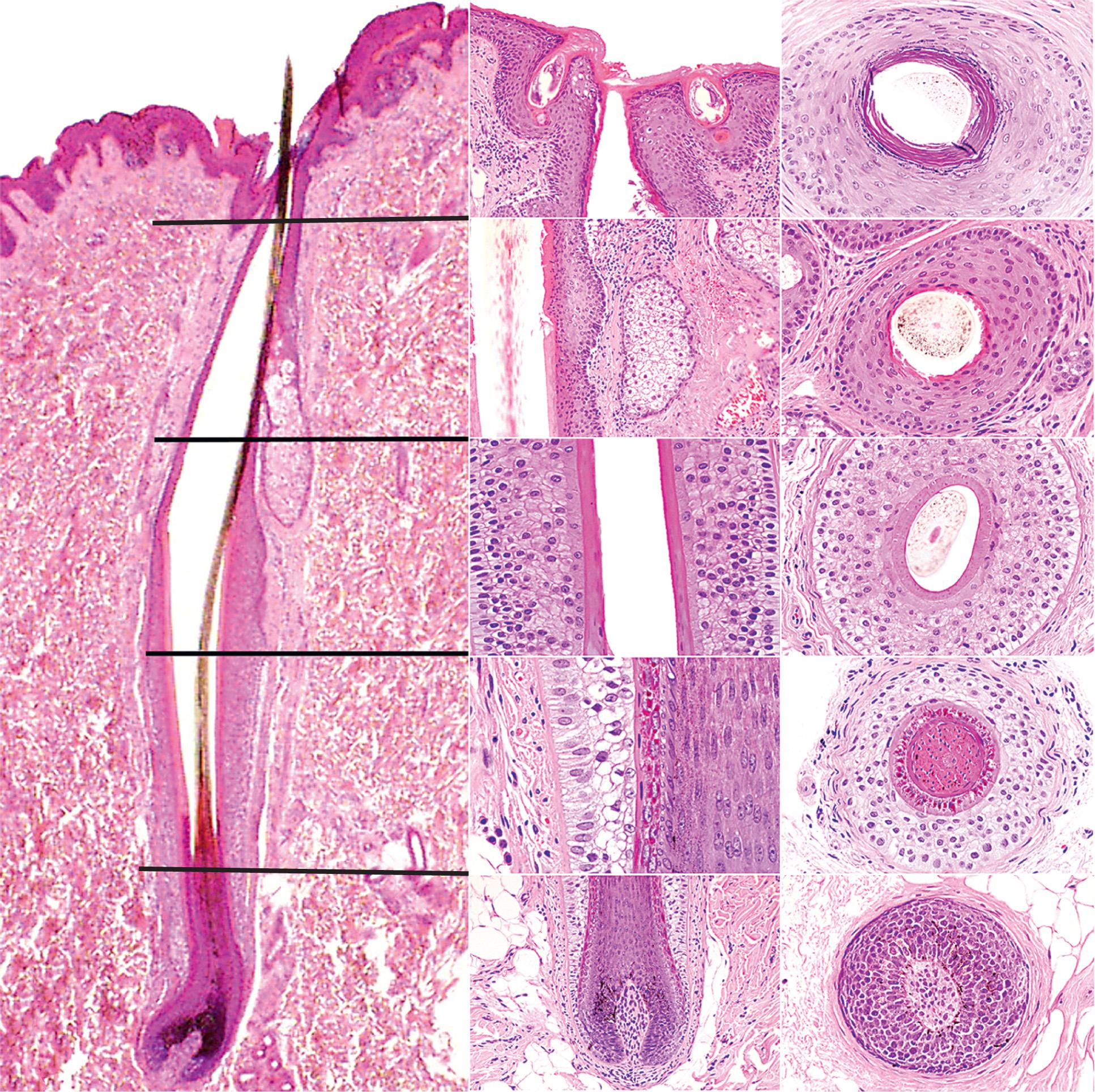
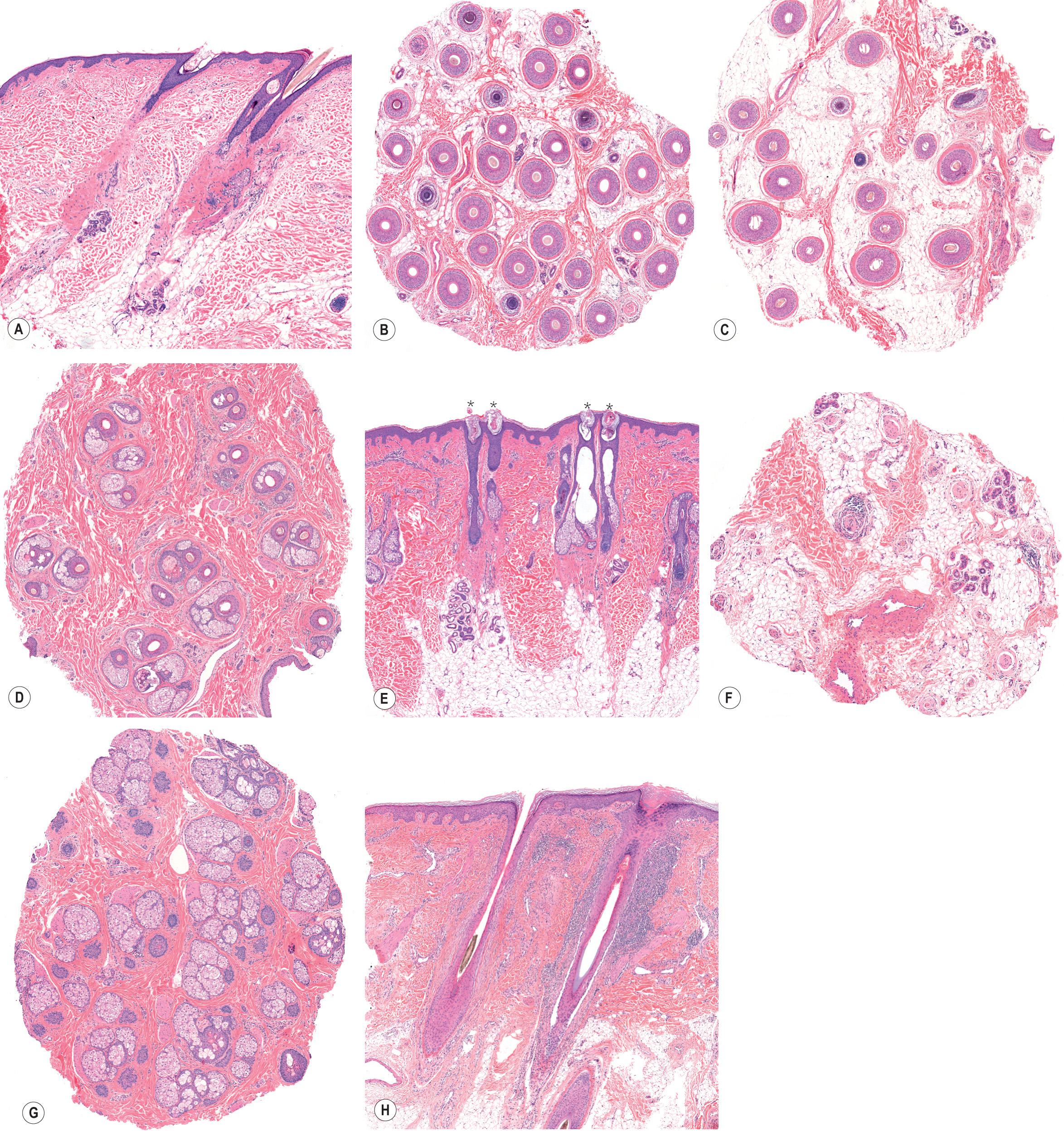
Scalp hairs exist as clusters (follicular units) composed of three to five shaft-producing follicles serviced by a single arrector pili muscle. One by one, as follicles miniaturize, the follicular units within thinning regions of the scalp begin to produce only one or two terminal hairs. Once all the follicles within a follicular unit miniaturize, baldness is observed. Histopathologic findings of MPHL and FPHL are described in Table 69.2 and are illustrated in Figure 69.9 as well as compared to normal hair follicles ( Fig. 69.8 ).
| HISTOLOGIC FEATURES OF VARIOUS FORMS OF ALOPECIA |
|---|
| Male and female pattern hair loss (androgenetic alopecia) (see Fig. 69.9 ) |
|
| Telogen effluvium |
|
| Trichotillomania |
|
| Alopecia areata (see Fig. 69.9 ) |
| Early, progressive disease (“acute” and “subacute”) |
|
| Longstanding and stable disease (“chronic”) |
|
| Postoperative (pressure-induced) alopecia |
|
| Psoriasiform alopecia |
|
| TNF-α inhibitor-induced psoriasiform alopecia |
|
| Central centrifugal cicatricial alopecia |
|
| Lichen planopilaris (see Fig. 69.9 ) |
|
| Discoid lesions of lupus erythematosus |
|
| Acne keloidalis |
|
| Dissecting cellulitis of the scalp |
|
| “End-stage” cicatricial alopecia |
|
| Traction alopecia (end-stage) |
|
The diagnosis of MPHL is straightforward unless it is coincidentally associated with other non-scarring hair diseases such as alopecia areata or telogen effluvium. Initial recognition of FPHL may coincide with a superimposed telogen effluvium. Early-onset or severe patterned hair loss in women should suggest the possibility of pathologic hyperandrogenism, and appropriate screening laboratory tests (total and free testosterone, dehydroepiandrosterone sulfate, and 17 hydroxy-progesterone) should be performed (see Ch. 70 ).
Topical formulations of minoxidil (2% solution, 5% solution, 5% foam) and oral finasteride have been approved by the US Food and Drug Administration (FDA) for the treatment of men with male AGA. Minoxidil is considered to be a biological response modifier and 1 ml is applied to the affected area twice a day. The most frequently reported adverse reactions are mild scalp dryness and irritation, and, rarely, allergic contact dermatitis. Minoxidil-induced hair growth is commonly associated with shedding of telogen hairs and a paradoxical worsening of hair loss ~4 to 6 weeks following initiation of treatment. This resolves with continued treatment.
Oral finasteride (1 mg daily), a type II 5α-reductase inhibitor ( Fig. 69.10 ), has been found to be effective in the treatment of balding in men . It halts hair loss in 90% of patients, and partial hair regrowth occurs in 65% of those receiving finasteride. Continued use of the product is necessary to sustain regrowth, which is also true for topical minoxidil; halting the medication will be associated with resumption of hair loss.
Possible finasteride side effects include reversible loss of libido, reduced volume of ejaculate fluid, and erectile dysfunction, which occurs in ~2% of men. There are reports of long-lasting sexual dysfunction (post-finasteride syndrome), but its incidence is unknown. While the overall incidence of prostatic carcinoma is reduced among elderly men who take finasteride 5 mg daily for benign prostatic hypertrophy, patients should be informed that this higher dose has been associated with an increased risk of the diagnosis of high-grade prostatic carcinoma . It is uncertain if the latter represents overdiagnosis due to enhanced screening or whether it is predictive of an increased risk of metastasis and a higher mortality rate . With regard to the effects of finasteride (1 mg/day) on lowering serum concentrations of prostate-specific antigen (PSA), the recommendation is to adjust the measured serum PSA concentrations upwards by 40–50% for the purposes of prostate cancer screening .
Surgical hair replacement, specifically hair transplantation and scalp reduction, are alternatives for the treatment of male androgenetic alopecia (see Ch. 157 ). Potential therapies such as the oral PGD2 receptor antagonist setipiprant await further studies.
In the US, topical minoxidil (2% solution, 5% foam) is approved for the management of FPHL. There is a low-to-moderate level of evidence to support its effectiveness . FPHL can develop in the setting of hyperandrogenemia, and women may benefit from oral contraceptives (to suppress ovarian androgen production), spironolactone ( Fig. 69.11 ), or, if appropriate, finasteride therapy . If oral finasteride or spironolactone is used in women with childbearing potential, appropriate contraception should be utilized (given the risk of feminization of the male fetus), with oral contraceptives being the rational choice. While finasteride (1 mg per day) appears to be ineffective in postmenopausal women , when given at higher daily doses of 2.5 and 5 mg, it can improve FPHL . However, the level of evidence in support of the use of finasteride for FPHL was recently judged to be low .

Dutasteride is a combined type I and type II 5α-reductase inhibitor. A dose of 0.5 mg/day leads to a greater reduction in serum and scalp DHT levels than does finasteride at 5 mg/day. This suggests that dutasteride may be a more effective therapy. While there are case reports of dutasteride leading to improvement of FPHL, the potential teratogenicity and prolonged biologic half-life preclude its use in women of childbearing age . Hair transplantation can also be offered to women with severe FPHL.
Increased shedding of otherwise normal telogen hairs in response to a pathologic or normal physiologic change in health status
A chronic form with no discernible precipitating factor is observed in some women
Laboratory evaluation is directed by history, physical examination, and microscopic evaluation of shed or plucked hairs
In the normal scalp, there are ~100 000 hair follicles of which ~90% will be in the anagen phase, and the remaining 10% in telogen (see Table 68.3 ). Telogen typically lasts for three months. Daily, ~50–200 hairs undergo exogen and are shed (see Fig. 68.4 ). Only 500–1000 follicles are in the transitional catagen phase on any given day. The biologic clock that determines the end of the anagen phase and the beginning of the catagen/telogen phase is a complex phenomenon whose molecular basis is beginning to be understood (see Ch. 68 ).
During the anagen phase, each human hair will grow for a few months to years before it becomes a telogen hair and is shed. Scalp hair grows longer than hair on other parts of the body because its anagen phase is longer. Unlike mammals that molt, hair cycling in humans is asynchronous such that shedding of each follicle is independent of surrounding follicles. Consequently, a fairly uniform density of hair is maintained at all times. Various metabolic alterations such as pregnancy, malnutrition, and other stresses are capable of adjusting the biologic clock within hair follicles, and it is possible for abnormally large numbers of hairs to enter the telogen phase simultaneously. When this happens, the hair loss is termed a telogen effluvium .
Depending on the cause of telogen effluvium, the period of excessive shedding can vary. Telogen effluvium is by far the most common form of hair loss due to medications or in association with systemic diseases or altered physiologic states. The causes of telogen effluvium are listed in Table 69.3 . However, a fair number of women have been found to have a persistent telogen effluvium without any discernible precipitating cause . This chronic telogen effluvium primarily affects women between the ages of 30 and 60 years and is a diagnosis of exclusion. Computer modeling of hair cycle kinetics has suggested that chronic telogen effluvium results from a reduced variance in the duration of anagen rather than a shortened anagen phase per se .
| CAUSES OF TELOGEN EFFLUVIUM |
|
If there is a definable precipitating event, hair loss begins approximately 3 months after this event, since it takes that amount of time for a hair follicle to progress through the telogen phase and then finally be shed. There is neither clinical nor histologic evidence of inflammation in “pure” telogen effluvium.
Most drugs that have been associated with hair loss, with the exception of antineoplastic agents, cause hair loss via telogen effluvium. While numerous medications have been associated with hair loss, only a subset of these are common causes of telogen effluvium (see Table 21.19 ). The most prominent offenders are retinoids (acitretin and isotretinoin) , anticonvulsants, antithyroid medications, anticoagulants, lithium, and interferons. More complete lists of medications associated with alopecia are readily available .
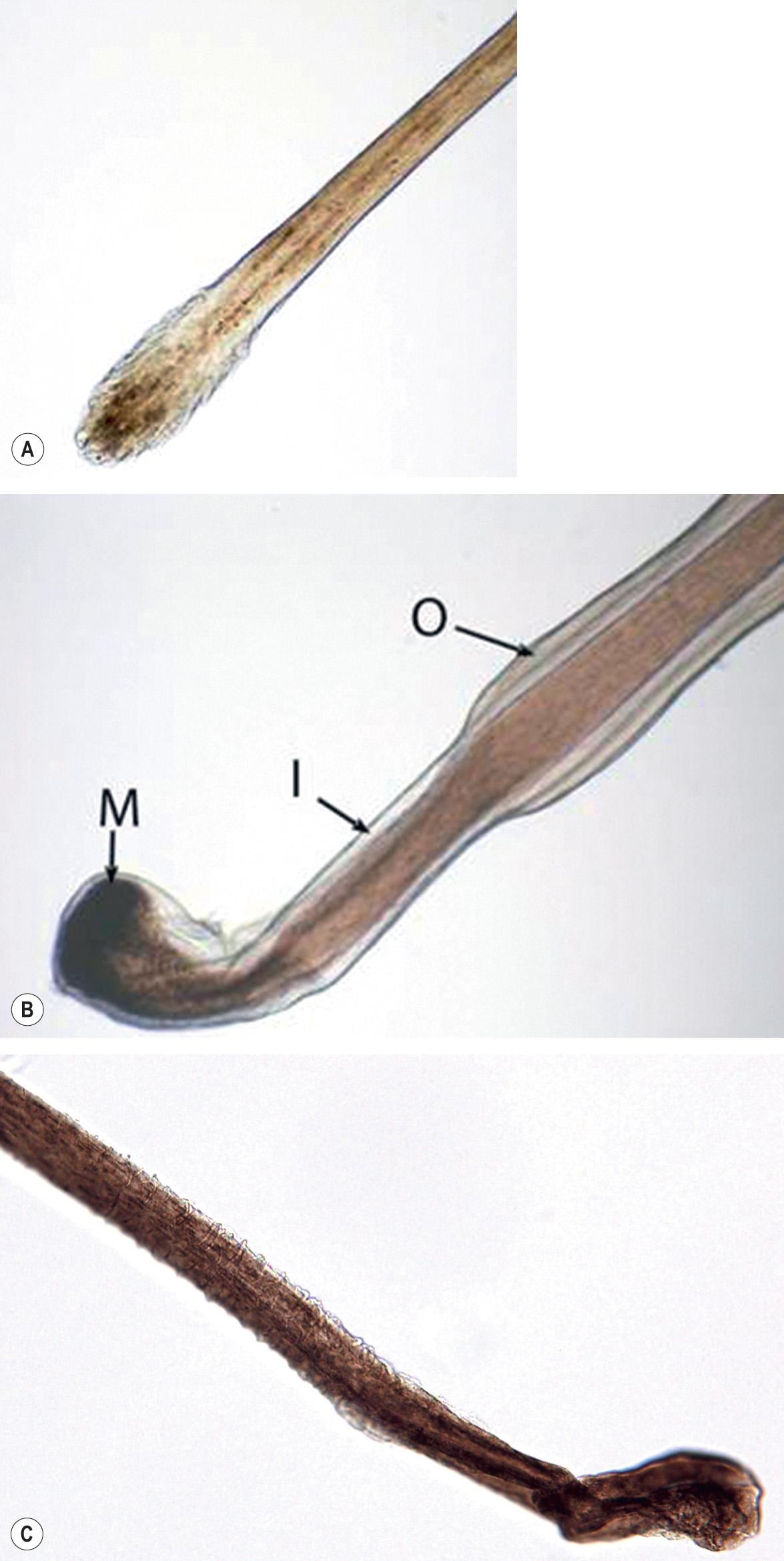
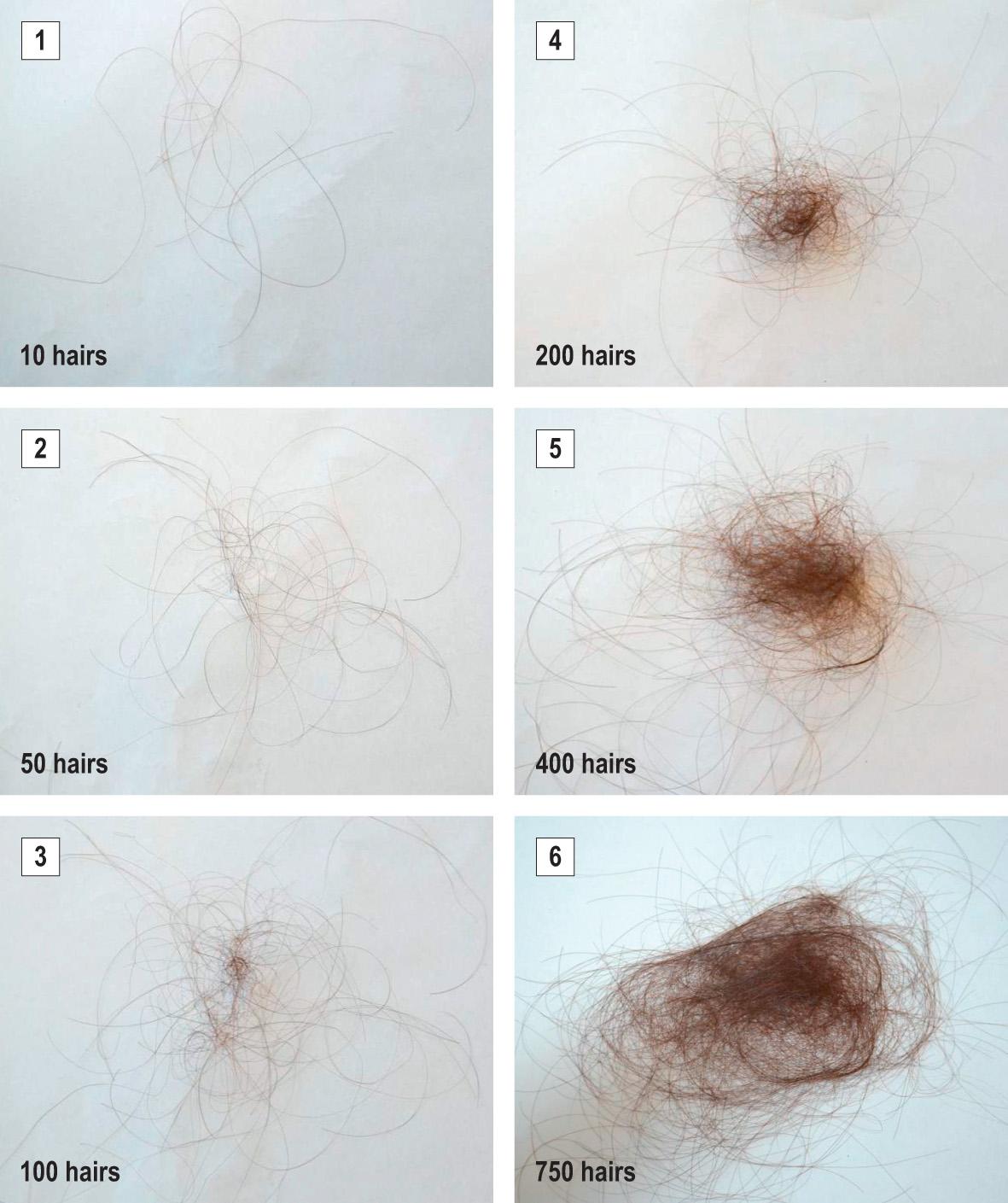
Thinning of the hair involves the entire scalp and may also be noted on other hairy regions of the body (e.g. pubic and axillary hair). A gentle hair pull may be positive for two or more normal telogen hairs ( Fig. 69.12 ). A forcible hair pluck (trichogram) will show a mixture of anagen and telogen hairs with the percentage of telogen in excess of 20% (see Fig. 69.2 ). While a telogen count of 15–20% is suggestive of abnormal shedding, >20% is diagnostic. In an active telogen effluvium, a 60-second timed hair count will usually be in excess of 100 hairs (the mean normal value is 10 hairs) . This method, which involves combing the hair forward for 60 seconds over cloth of a contrasting color before shampooing, can be used to follow the progression and eventual resolution of a telogen effluvium. In an attempt to assist patients in describing the amount of daily hair shedding they are experiencing, a visual scale that depicts varying numbers of hairs has been proposed ( Fig. 69.13 ) . The histopathologic findings in telogen effluvium are outlined in Table 69.2 .
Eventually complete hair regrowth is expected. The prognosis for women with chronic telogen effluvium is relatively good, for although hair shedding can continue for many years, this does not appear to lead to baldness . The prognosis for telogen effluvium associated with systemic disease is excellent if the precipitating cause is eliminated.
When the cause is unclear, the evaluation of a patient with telogen effluvium includes thyroid and chemistry panels, sedimentation rate, hematocrit, and ferritin (as a reflection of total body iron storage). According to literature recommendations, ferritin levels should be at least 40 ng/dl, but the significance of abnormal values is uncertain . In persistent cases of telogen effluvium, i.e. those lasting beyond 6 months, a scalp biopsy specimen submitted for horizontal sectioning can prove useful in excluding early AGA; the ratio of terminal to vellus hairs counted at the level of the isthmus allows distinction . However, there does remain the possibility of the coexistence of both disorders. Trichoscopy findings are shown in Fig. 69.7B .
Non-scarring patterned alopecia, most commonly presenting as circular areas of alopecia
Organ-specific autoimmune disease involving T cells
Can lead to total scalp hair loss (alopecia totalis) or complete scalp and body hair loss (alopecia universalis)
Celsus is credited with describing patterns of hair loss using the Greek word alopekia , meaning fox mange, and Sauvages coined the term “alopecia areata”. Alopecia areata is a non-cicatricial alopecia that is postulated to be a hair-specific autoimmune disease, with genetic factors playing a role in disease susceptibility and severity. A concordance rate of 55% has been found in identical twin studies, implicating both genetic and environmental factors.
In the acute progressive stage of alopecia areata, lymphocytic infiltrates are seen around, and sometimes within, the hair bulb region of anagen follicles. Despite the presence of this inflammatory infiltrate, the follicle retains its potential to produce hair, implying that the follicular stem cells remain viable.
The chronic relapsing nature of alopecia areata and its profound effect on physical appearance make the development of this condition a distressing and life-changing event for many affected individuals .
The prevalence of alopecia areata in the US is ~0.1% to 0.2% of the population . The average lifetime risk of developing alopecia areata is estimated to be 1.7%. Overall, one in five patients with alopecia areata reports that another family member has the disease.
There are multiple hypotheses regarding the pathogenesis of alopecia areata, ranging from an environmental insult such as a viral infection to a genetic susceptibility to T-cell-driven autoimmunity . The latter could result from a primary attack of the immune system against the hair follicle or a breakdown in the hair follicle's immune privilege which leads to a secondary attack by the immune system (see Ch. 68 for details). Of course, it is most likely that there is an interplay of several factors and depending upon the particular patient or subtype, one factor may play a more important role.
With regard to genetic susceptibility, genome-wide association studies have identified several loci which are involved in immune regulation, including that of regulatory T cells . Examples of these genes include those that encode HLA alleles, interleukin (IL)-2 and -21, the IL-2 receptor A, and cytotoxic T lymphocyte-associated protein 4 (CTLA-4; Table 69.4 ) . Additional associated genes point to a role for oxidative stress and disrupted autophagy/apoptosis.
| ALOPECIA AREATA: DISEASE AND GENETIC ASSOCIATIONS |
| Associated diseases |
|
| HLA associations |
|
| Additional genome-wide associations |
|
Evidence in support of a T-cell-driven autoimmune process includes the observation that CD8 + T cells are the initial intrafollicular lymphocytes to appear in alopecia areata. In mouse models, it is also possible to induce alopecia within transplanted human skin by transferring CD8 + T cells, but this does not occur if T cells are depleted . Cytotoxic CD8 + NKG2D + T cells, which produce interferon (IFN)-γ, are thought to play a key role in pathogenesis (see Ch. 68 for details). Involvement of IFN-γ and the γ-chain cytokines (IL-2, IL-7, IL-15, IL-21) implicates downstream signaling via the JAK (Janus kinase)/STAT pathway (see Fig. 128.10 ). These findings represented the rationale for cytokine-targeted therapy and indeed the JAK inhibitors tofacitinib and ruxolitinib did promote hair regrowth in separate uncontrolled clinical studies.
As noted previously, collapse of the hair follicle's immune privilege may play a role in the pathogenesis of alopecia areata . Normally, anagen hair follicles express low levels of MHC class I molecules (thereby minimizing presentation of autoantigens), upregulate immunosuppressant molecules such as TGF-β1 and α-MSH, and do not activate natural killer (NK) cells by expressing UL16 binding protein 3, an NKG2D ligand. In that hair matrix immune privilege is restricted primarily to the anagen phase, it has been postulated that an autoantigen from melanocytes, which are active during the anagen phase, could be responsible for initiating the immune response against the hair follicle.
Alopecia areata commonly presents as round or oval patches of non-scarring hair loss ( Fig. 69.14A ). Short “exclamation point” hairs (i.e. distal end broader than the proximal end) can often be seen, particularly at the margins of areas of alopecia ( Fig. 69.14B ). Other presentations include alopecia totalis (loss of all scalp hair), alopecia universalis (loss of all scalp and body hair; Fig. 69.14C ), an ophiasis pattern (band-like pattern of hair loss along the periphery of the temporal and occipital scalp; Fig. 69.14D ), and alopecia involving the beard area ( Fig. 69.14E ). The reticular variant is characterized by recurrent patchy disease, in which the patient experiences hair loss in one area while at the same time undergoing spontaneous regrowth in other sites. The rare diffuse variant of alopecia areata can manifest with widespread thinning or may primarily affect the top of the head. Non-pigmented hairs may initially be spared, and, as a result, some patients with diffuse involvement will appear to develop rapid graying of the hair. With regrowth, the hairs may initially be gray or white, but repigmentation is usually observed within a few weeks or months .

In addition to the hair follicle, nails may be involved. The most common abnormality is nail pitting, but other changes described include trachyonychia (sandpaper-like roughness due to excessive longitudinal ridging; Fig. 69.14F ), brittle nails, onycholysis, koilonychia and, rarely, onychomadesis (see Ch. 71 ).
Disease associations are listed in Table 69.4 . The histopathologic features of alopecia areata (see Fig. 69.9 ) are described in Table 69.2 , and trichoscopy findings are shown in Fig. 69.7C .
Tinea capitis, trichotillomania, temporal triangular alopecia, traction alopecia, secondary syphilis, and loose anagen syndrome need to be considered in the differential diagnosis of alopecia areata as well as pressure-related alopecia, aplasia cutis, and “burnt-out” cicatricial alopecia. The diffuse variant may initially be confused with telogen effluvium and androgenetic alopecia. Usually, the history and clinical examination (including trichoscopy) is sufficient to distinguish between these conditions, but performing a scalp biopsy may prove useful for less distinctive presentations.
Treatment studies are difficult to perform because the disease has an unpredictable course and may improve on its own. Nevertheless guidelines have been established to facilitate research .
Numerous therapies are available for the management of alopecia areata ( Table 69.5 ), and several can be utilized in combination. The treatment of patchy alopecia areata may include topical or intralesional corticosteroids , topical minoxidil (2% or 5%), topical anthralin (0.5–1% cream applied daily; see Ch. 129 ), and combination therapy. The concentration of intralesional corticosteroid is usually 2.5–5 mg/ml of triamcinolone acetonide , and injections can be repeated every 4–8 weeks. This medication should be injected at the level of the mid dermis to target the diseased, miniaturized hair bulbs.
| TREATMENT OPTIONS FOR THE MANAGEMENT OF ALOPECIA AREATA |
| Topical and intralesional corticosteroids (1) |
| Topical irritants (e.g. anthralin, tazarotene, azelaic acid) (2) |
| Topical minoxidil (2) |
| Topical immunotherapy (e.g. squaric acid dibutyl ester, diphencyprone) (1) |
| Systemic corticosteroids, pulsed dosing * (especially if rapidly progressive) (2) |
| Systemic JAK/STAT pathway inhibitors: tofacitinib (2), ruxolitinib (3) |
| Topical or oral photochemotherapy (PUVA) (2) |
| Excimer laser (3) |
| Systemic corticosteroids, chronic (2) |
| Systemic cyclosporine (3) |
* e.g. oral prednisolone 300 mg (5 mg/kg for children) monthly for a minimum of three doses.
A dependable and safe treatment for extensive disease (totalis or universalis) has yet to be found, although spontaneous recovery is possible (albeit rarely), even in longstanding disease. Approximately 80% of patients will respond to high-dose systemic corticosteroids (e.g. 40 mg triamcinolone intramuscularly monthly, or daily oral prednisolone or dexamethasone tapered over 6–8 weeks); however ~50% will relapse with dose reduction or cessation of therapy . Long-term maintenance therapy with oral corticosteroids is rarely justified and steroid-sparing agents such as azathioprine and methotrexate are unreliable.
Topical immunotherapy (with diphencyprone or squaric acid dibutyl ester) is a non-FDA-approved treatment for extensive disease. Clinicians interested in using topical immunotherapy should carefully review the published protocols ( Table 69.6 ). PUVA, potent topical corticosteroids under plastic occlusion, and systemic targeted immunomodulators (“biologics”) have all been tried with less success. More recently, promising results with oral JAK/STAT pathway inhibitors (e.g. tofacitinib , ruxolitinib ) have been reported, but relapse following discontinuation is an issue. Of note, patients with the ophiasis pattern of hair loss are more resistant to therapy than are other patients with similar amounts of hair loss.
| TOPICAL IMMUNOTHERAPY FOR ALOPECIA AREATA |
| Treatment protocol for diphencyprone (DPCP) or squaric acid dibutyl ester (SADBE) * |
|
| Additional information |
|
| Contraindications |
|
The treatment of eyebrows with intralesional corticosteroids is usually helpful, even in extensive cases. When eyelashes are absent, the wearing of eyeglasses can serve as a distracting cosmetic enhancement. All patients should be directed to the resources provided by the National Alopecia Areata Foundation ( www.naaf.org ) for extensive practical information about support groups, wigs, cosmetics, and the latest research.
Self-induced plucking or breakage of hair
Often associated with psychological stress or a personality disorder
Incomplete and distorted follicular anatomy is a histologic hallmark
The term “trichotillomania” is derived from the Greek thrix , hair; tillein , pulling out; and mania , madness. Trichotillomania is seen more commonly in females than in males, and in children more than adults. Onset of the disease is usually during early childhood to adolescence, and its prevalence is uncertain.
Trichotillomania is listed in the American Psychiatric Association's diagnostic classification system, DSM-5, as one of the “obsessive-compulsive and related disorders” ( Table 69.7 ) . However, many patients who chronically pull their hair do not meet all of the DSM-5 criteria for trichotillomania.
| DSM-5 DIAGNOSTIC CRITERIA FOR TRICHOTILLOMANIA (HAIR-PULLING DISORDER) |
|
Individuals with trichotillomania typically represent a very heterogeneous group, varying from those with a mild habit to others who have an impulse-control disorder, personality disorder, intellectual disability, or a psychosis (see Ch. 7 ) . The DSM-5 criteria do recommend distinguishing trichotillomania from mental disorders that better explain the hair pulling, e.g. body dysmorphic disorder. Often the hair pulling that occurs during infancy and early childhood (boys>girls) resolves without treatment.
Individuals with trichotillomania usually pluck scalp hair, resulting in patchy or full alopecia of the scalp ( Fig. 69.15A ). Some patients may also pluck from other hair-bearing regions such as the eyebrows, eyelashes, face, extremities, or pubic region. Patches of alopecia often have bizarre shapes, irregular borders, erosions, and contain hairs of varying lengths ( Fig. 69.15B ). Plucking may cause hair shaft fractures, and emerging shafts tend to feel “rough”. In severe cases, hairs in the occiput tend to be spared. The clinical diagnosis can be supported by creating a “hair growth window” by repeatedly (weekly) shaving a small area of involved scalp to demonstrate normal, dense regrowth.
The histopathologic changes seen in trichotillomania are listed in Table 69.2 . When incomplete or distorted follicular anatomy is found, suspected plucking is confirmed.
The differential diagnosis includes tinea capitis, alopecia areata and monilethrix, which can be excluded by history, physical examination, trichoscopy, KOH examination, fungal culture, and scalp biopsy. Trichoscopy reveals irregularly broken hairs in virtually all patients (see Fig. 69.7D ). Trichoptilosis (split ends), the V-sign (2 broken hairs of equal length arising from a single follicle), and black dots can also be seen . Other less constant findings are coiled hairs, flame hairs (remnants of proximal hair shafts), and tulip hairs (darker ends in the shape of a tulip). Exclamation point hairs, typical of alopecia areata, are rarely observed. In such cases, histopathology can assist in determining if both disorders are present.
No specific treatment approach has been established as effective in any large controlled study. Hypnosis, behavioral modification therapy, insight-oriented psychotherapy, and pharmacologic therapy have all been tried, but success rates are low. If pharmacological therapy is considered, the recommended first-line medication is clomipramine. Selective serotonin reuptake inhibitors (SSRIs) have been tried without convincing success.
This form of hair loss is seen most commonly in patients who have undergone lengthy surgical procedures under general anesthesia where a portion of their scalp has been in prolonged contact with the operating table.
Postoperative alopecia typically presents as a solitary, roughly oval patch at the site of greatest pressure, most often the upper occiput. Usually complete hair regrowth occurs, although several cases of permanent (i.e. cicatricial) hair loss have been reported. The histologic findings in postoperative alopecia change as the lesion evolves (see Table 69.2 ) . An analogous condition in newborns is halo scalp ring which manifests as a self-resolving occipital band of alopecia that is believed to be due to pressure from the maternal cervix during labor .
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here