Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Maintaining expertise in airway management is the responsibility of every airway practitioner. This responsibility extends throughout one’s professional career and reaches far beyond the formative years of medical training into lifelong learning to stay competent.
The essential ingredients of expertise are the willingness to become an expert, deliberate practice, immediate feedback, problem solving, and evaluation with an opportunity to modify or repeat performance.
Traditional in situ education in the operating room can be optimized and structured to minimize any adverse effect on patient care. Background knowledge and skill can be assessed before entering the operating room, educational goals can be clarified, and supervision is provided during the case with immediate feedback.
The features of a good clinical teacher include good content knowledge combined with an ability to provide a positive learning environment, excellent listening skills, constructive feedback even in difficult situations, and enthusiasm for education and the learners.
Simulation-based medical education (SBME) provides valuable opportunities to supplement or even supplant traditional clinical training. Procedural and nontechnical skills can be developed and assessed in an environment that is safe for the patient, the learner, and the instructor. Training is conducted without patient involvement where mistakes can be safely repeated, procedures can be interrupted for feedback, difficult scenarios can be rehearsed, and trainees can learn at their own rate. Short, structured briefing before the case and debriefing after can be rehearsed and this habit can be integrated into daily clinical practice.
Assessment provides a vital link between airway management education and improved patient care. Learning should be measured and performance assessed to meet defined levels of expertise. Ideally, these standards of performance should be associated with patient audits to ensure improved patient care. Signing off for independent practice is based on a new educational concept: entrusted professional activities.
There are many opportunities to improve education in airway management. Research is required to expand the opportunities offered by SBME. Assessment techniques should be implemented and refined, and training options should be evaluated to establish the value of new opportunities provided by remote learning.
Education, along with research and clinical patient care, is one of the three pillars of academic medicine. For any practitioner engaged in airway management, education is an essential requirement for their own development and as a teacher imparting knowledge and skill to junior or senior colleagues. Generally, those “airway teachers” are expected to display a high standard of knowledge, procedural skill, and professionalism throughout their careers. Sadly, these standards sometimes fall short and, consequently, that can lead to patient harm. This was reported in the Fourth National Audit Project (NAP4) of the Royal College of Anaesthetists and the Difficult Airway Society. In that audit 184 patients with severe airway morbidity or mortality were reviewed by an expert panel looking for causal or contributory factors. Poor judgment (59%) and inadequate education or training (49%) were the second and third most common contributory factors of risk, respectively, after patient factors (77%). Deficiencies in airway assessment, failure to follow an airway plan, inappropriate use of supraglottic airways, and underutilization of awake intubation were found. Difficult, delayed, and failed tracheal intubation accounted for 39% of adverse events identified in this UK survey. That was a kind of “wake-up call,” and suddenly, airway management was in the middle of the debate to improve the anesthetist’s performance and patient safety. Over the last decade, new concepts from education research have been developed and new opportunities for teaching are now available, which are being applied to develop a safer approach to airway management.
Before embarking on a detailed discussion of education for airway management, it would be helpful to understand where the deficiencies remain. An international survey conducted in 61 countries, including 4948 individual questionnaires, found deficiencies in accessing practice guidelines and key airway equipment, particularly in low-income countries (LIC). For example, in low-resource settings emergency front-of-the-neck equipment was available in less than 60% and videolaryngoscopes in less than 50% of locations. In total, 91% of the respondents agreed that airway management skills should be assessed, and 60% of respondents thought training should be mandatory for trainees, but only 34% felt it should be mandatory for continuing medical education. Lack of confidence performing a number of skills was reported, including emergency invasive airway access, awake intubation with a flexible intubation scope (FIS), intubation via a supraglottic airway (SGA), asleep FIS, and retrograde intubation. Similar findings were reported in a Danish survey, where most anesthesiologists rated their competence as high or very high for basic airway management. Conversely, confidence dropped for advanced airway management techniques, where low procedural volume was a problem.
In this chapter we will review the strengths and weaknesses of current education practice in airway management and identify areas for improvement. We will examine the role of simulation-based medical education (SBME) and review other opportunities to expand airway management competencies. Undergraduate and postgraduate airway management education and the importance of lifelong learning for all persons dealing with airway management will be considered, along with the importance of training the airway trainers and faculty development. Consideration of human factor training, leadership development, and current concepts in airway management research will conclude the chapter. The reader will not be surprised that very little specific evidence exists about education in airway management. Very often, approaches and results from studies in other fields of medicine need to be translated for their use in the teaching and learning of airway procedures. That again leads to a call for high-impact research in airway management education.
Most airway practitioners have learned airway management at work, by acquiring practical skills and maybe learning from a mentor while attending to patients. This apprenticeship model of medical education can be traced back over a hundred years and is still a widely applied form of medical education for airway management. At the turn of the 20th century, Dr. William Osler and Dr. William Halsted from Johns Hopkins Hospital were the first to formalize and structure medical training and are credited with laying the foundations for our current residency training programs. Emphasis was placed on mentors, behavioral modeling, rotations, and evidence-based medicine. Halsted characterized surgical teaching in three phases: “See one, do one and teach one.” This stepwise learning was a good idea at the time. Medical trainees first observed someone performing a procedure, then after understanding the procedure, they performed it, mostly under supervision, and after mastering a skill, the final aim was to teach the procedure. Halsted’s idea about resident education revolutionized medical education as it meant not “learning by doing” and is not that far away from currently applied teaching practice. Exposure to cases to gain experience and competence is still widely discussed with very diverse opinions. The current question is how can we train young doctors without jeopardizing safety or harming patients when performing procedures for the first time, as well as in subsequent practice?
In many anesthesia teaching institutions this traditional apprenticeship model of medical education is still regarded as the standard for teaching. Learning airway management during patient care has obvious advantages of involving real anatomy, physiology, and pathology with a wide range of patient presentations. Despite these positive features, there are many difficulties and inadequacies associated with the apprenticeship model. It is becoming increasingly difficult for trainees to find sufficient time in their rotations to gain expertise in managing a challenging or difficult airway. Skill development takes time, and that time varies between individuals. In the interest of patient safety and the well-being of doctors at their workplace, limitations have recently been imposed on trainee working hours. In Europe that limit is between 40 and 56 hours per week, and 80 in the United States. Restrictions have also been imposed on the duration of on-call time and a requirement for time off after being on-call. These initiatives are designed to reduce fatigue and burnout, but inevitably they impact education and training time, as well as case load. The apprenticeship model relies on exposure to patients with normal and abnormal airways and the availability of a dedicated airway teacher for supervision and guidance. Due to the low incidence of many complex airway problems, it can take a long time to gain the required experience necessary to be considered trustworthy at managing a difficult airway ( Table 49.1 ).
| Difficult intubation | 6.2% |
| Difficult bag-mask ventilation | 1.4% |
| Difficult bag-mask ventilation, difficult laryngoscopy | 0.4% |
| Impossible bag-mask ventilation | 0.15% |
| Impossible laryngeal mask | 1.1% |
| Impossible intubation, difficult bag-mask ventilation | 0.3% |
| Impossible intubation, impossible ventilation | 0.0019% |
New concepts were introduced, defining not only competencies but also skilled performance that enable supervisors to trust a learner in their performance. These Entrustable Professional Activities (EPAs) are a further development of the apprenticeship model as still the “master” defines the EPA and the learner needs to reach these aims with all the limitations described before.
During the formative stage of skill development, patients are exposed to novices with an increased risk of side effects and complications. For example, paramedics intubating in an emergency prehospital situation had a 36% failed intubation rate and 11% unrecognized esophageal intubation rate. All of these patients were subsequently successfully intubated by prehospital physicians. Failed intubation and esophageal intubation are associated with a high incidence of morbidity and mortality, demanding close supervision of novices during their skill development. Similar results were seen with emergency physicians engaged in out-of-hospital retrieval medicine, where high rates of esophageal and endobronchial intubation were reported.
Teaching in the operating room can increase the workload of the tutor and may cause distraction by diverting attention away from the patient. The often noisy environment with a lot of people in the room does not create a learning-suitable climate for both the learner and the airway teacher.
Training in the operating room has financial implications. Clinical bronchoscopy takes 50% longer when a trainee is involved and 18 minutes can be added to procedure time. There is also a threefold increase in complication rates. Operating room efficiency often takes precedence over teaching, and therefore trainees can be neglected during rapid turnover operating sessions.
Ethical issues arise concerning patient safety when unorthodox techniques or unnecessary procedures are used for clinical training. Selecting an SGA for teaching when a tracheal intubation might have been a safer option or distorting the larynx to create a difficult intubation are examples where patient safety could have been compromised. Ideally, patients should be informed and give consent for trainee care, particularly when that trainee is performing a complex procedure such as flexible bronchoscopy for the first time.
Trainees find it confusing when they are exposed to a range of different tutors and a lack of standardization. A very disturbing downside of the apprenticeship model is when instructors each have “their own way.”
These issues have prompted a reassessment of the apprenticeship model for airway management training. Alternative training methods have the potential to supplement or even replace traditional clinical teaching with the aim to educate more efficiently and overcome the deficiencies of the apprenticeship model by dealing with a limited clinical case load.
Effective education in airway management is far easier with a mentor who is interested in the learners and wants to facilitate the development of cognitive and practical skill, as well as personal and professional growth, to an expert level. Most clinicians have not received any formal education as a clinical teacher, but teach-the-teacher courses are becoming more common and certain characteristics have been identified as worthy attributes for this task. Many of the attributes of a good clinical teacher relate to their personality. , The features of a good clinical teacher include good content knowledge and clinical skills, combined with an ability to create a positive learning environment, have excellent listening skills, provide feedback (even in distressing and embarrassing situations), and show general enthusiasm for teaching. These attributes apply particularly to medical teaching but also are required of clinical teachers who serve as a specialty role model for the learners and their situation. Senior faculty often act as a coach in short-term rotations, achieving previously established educational goals, but can act as mentors to junior faculty and reinforce positive attributes in long-term relationships over residencies and beyond. ,
Providing feedback is viewed increasingly as a normal component of the teacher–learner relationship in both directions, to the learner but also from the residents to the teaching staff. Feedback extends into debriefing competencies, which are components of excellence in teaching. Such teaching excellence needs to be recognized and rewarded by the corresponding institutions and educational bodies as it improves the performance of faculty and prevents burnout. , Bould et al. identified techniques to improve clinical teaching, which emphasize the importance of constructive and supportive feedback ( Table 49.2 ).
| Before the Case |
|
|
| During the Case |
|
|
|
|
| After the Case |
|
|
|
|
|
|
|
|
Effective learning experiences can be created before and after clinical contact. This also minimizes the impact of some of the problems already discussed, including distraction from patient care during teaching and the creation of a proper learning climate. It is important before the case for the learner to establish familiarity with the level of knowledge, competence, and understanding of the airway problem of the patient. In learner-centered education the specific educational goals can be discussed and defined and the teacher might seek agreement with the learner on the teaching plan that describes how the learner is going to achieve their objective with the help of the teacher. An educational goal to achieve competency in a particular task is intimately linked to the level of knowledge and prevailing skill of the learner. A novice achieving competency at holding a face mask on a patient with normal morphology is quite a different educational goal from that demanded of an advanced trainee who is required to hold a face mask on a patient with a difficult airway due to a beard. Theoretical concepts can be acquired beforehand by reading or video-assisted instruction appropriate for the learner. The concrete techniques can be discussed and rehearsed on a manikin outside the operating room prior to patient contact. The concept of the “flipped classroom” to engage the learners with the theoretical background before being involved with a patient in the OR or in the classroom setting is highly effective and accommodates the busy clinical environment by allowing the learner to enter directly into the clinical education of the airway skill. After the case, debriefing provides constructive and corrective feedback, which will further enhance the learning experience ( Table 49.2 ).
A useful concept that relates clinical skills, competence, performance, and assessment is Miller’s learning pyramid , ( Fig. 49.1 ). Four stages are described: knows, knows how, shows how, and does. This concept can apply to the development of a procedural skill with an airway device such as an SGA. Equally, nontechnical skills can develop with this model. These stages can be conducted outside the operating room using simulation with assessment and feedback provided at each level. The final stage of “does” leads to the transfer of the newly developed skill into the clinical environment.
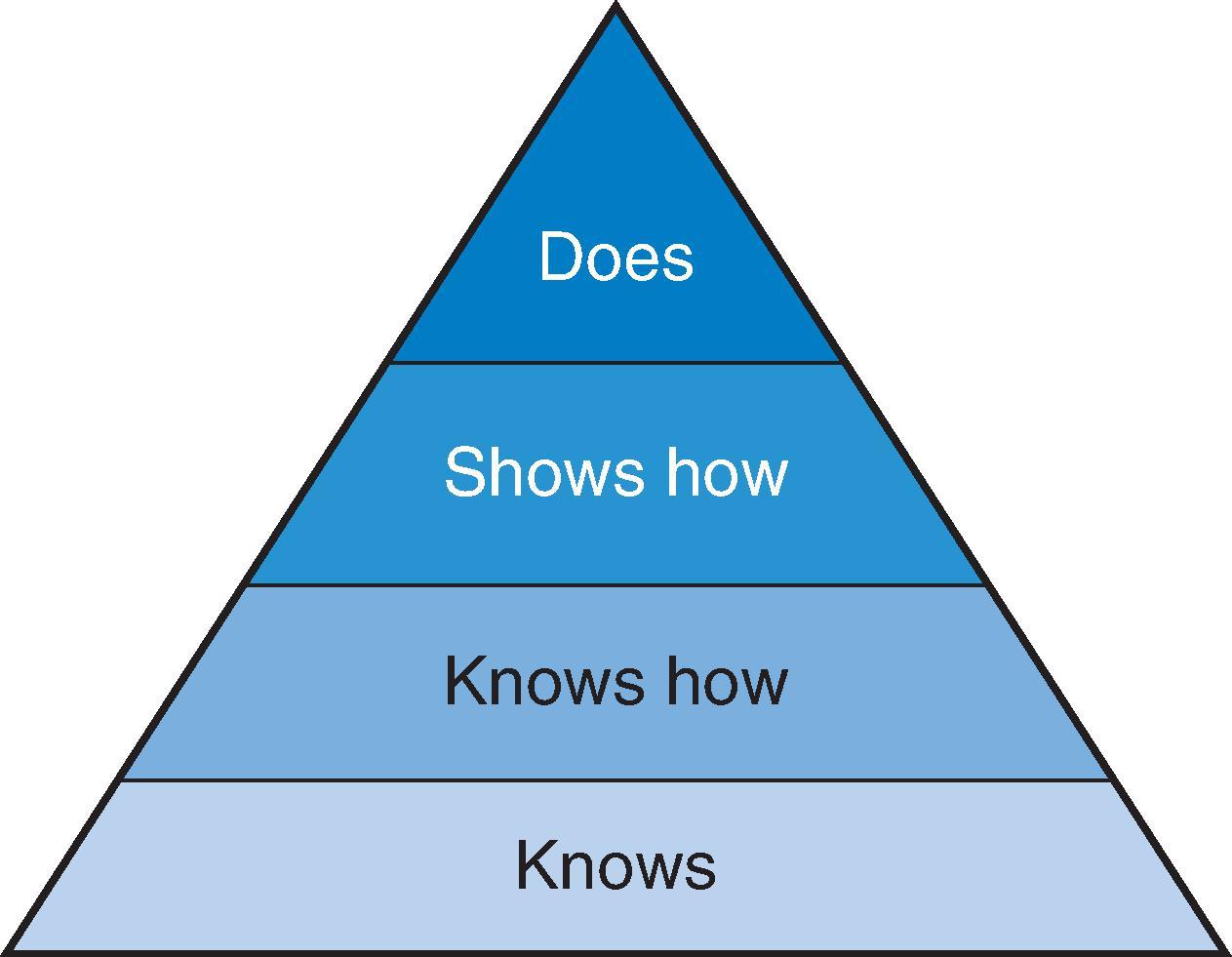
The base of Miller’s learning pyramid is the cognitive knowledge level, which forms the foundation upon which all other aspects of learning rest. This “knows” level is commonly assessed by using written objective tests. The “knows how” level requires the ability of the learner to manipulate and apply knowledge and the understanding of relationships between concepts in an appropriate way to suit the environment. This would require the learner to explain the context of use, the technical details of ancillary equipment. This “knows how” level usually is assessed by written and online (gaming) tests with problem solving or oral examinations. The “shows how” level may require a standardized simulation exercise on manikins, incorporating learners’ communication skills and a demonstration of the appropriate use of devices or techniques in a safe nonclinical environment. This demonstration is assessed mostly in standardized observations or measurements, like objective structured clinical exams (OSCE) in a simulation environment or with simulated patients, and often accompanied by feedback. The “does” level may occur under supervision at the workplace with assessment by the direct clinical observation of procedural skills (DOPS) or clinical encounters (Mini-CEX) in the clinical environment, including multisource feedback. Recently, a fifth top level has been proposed, namely, trust of clinical responsibilities in learners working without supervision or assistance. That means the readiness to cope and the capability to adapt to familiar and unfamiliar challenges in clinical practice as needed. That might be assessed during observation of clinical practice and risk assessment.
An expert airway practitioner needs to be able to manage a broad range of challenging and difficult airways. How can that expertise be acquired? Traditionally it has been assumed that with experience, expertise will follow. Similarly, training has been based on the volume of practice to reach a satisfactory level of competence. A study found that it took 200 tracheal intubations under supervision to achieve 95% success in the operating room. Based on the figures from Table 49.1 , it could take a very long time for a trainee or a young specialist to gain significant exposure to managing rare events such as difficult or failed intubation. Another study examined the learning curve for SGA and found that supervision was required for the first 40 insertions. This number might not include any impossible SGA insertions because of the 1.1% incidence of that problem. These figures highlight the problems associated with the apprenticeship model and experiential learning of airway management (learning by doing) in the operating room, where experience is ad hoc and based on the volume of cases seen by chance, the incidence of difficult cases, and the rate of learning by the individual practitioner.
Anders Ericsson is an educational psychologist who has studied expertise in various domains, including music, science, and sport. He argues that experience does not guarantee expertise. An individual may perform an activity poorly over a long period of time without ever developing expertise. In a systematic review of the relationship between clinical experience and quality of health care Choudhry et al. found decreasing performance with increasing years of practice. A systematic review of the effect of experience and exposure on expertise showed that exposure to cases is the driving factor to maintain competency that relates to better patient outcome.
Ericsson has identified the key behaviors of experts who excel in their field. Besides their positive attitude, these behaviors include deliberate practice, immediate feedback, problem solving, and evaluation with an opportunity to modify or repeat their performance, which means voluntary engagement in constant challenges to master beyond daily clinical practice: ideally, to have others provide formative feedback on the performance aiming for small but constant improvements and finally to rehearse and redo the professional and manual skills, if the clinical context permits. The development of airway management expertise can evolve with these same behaviors.
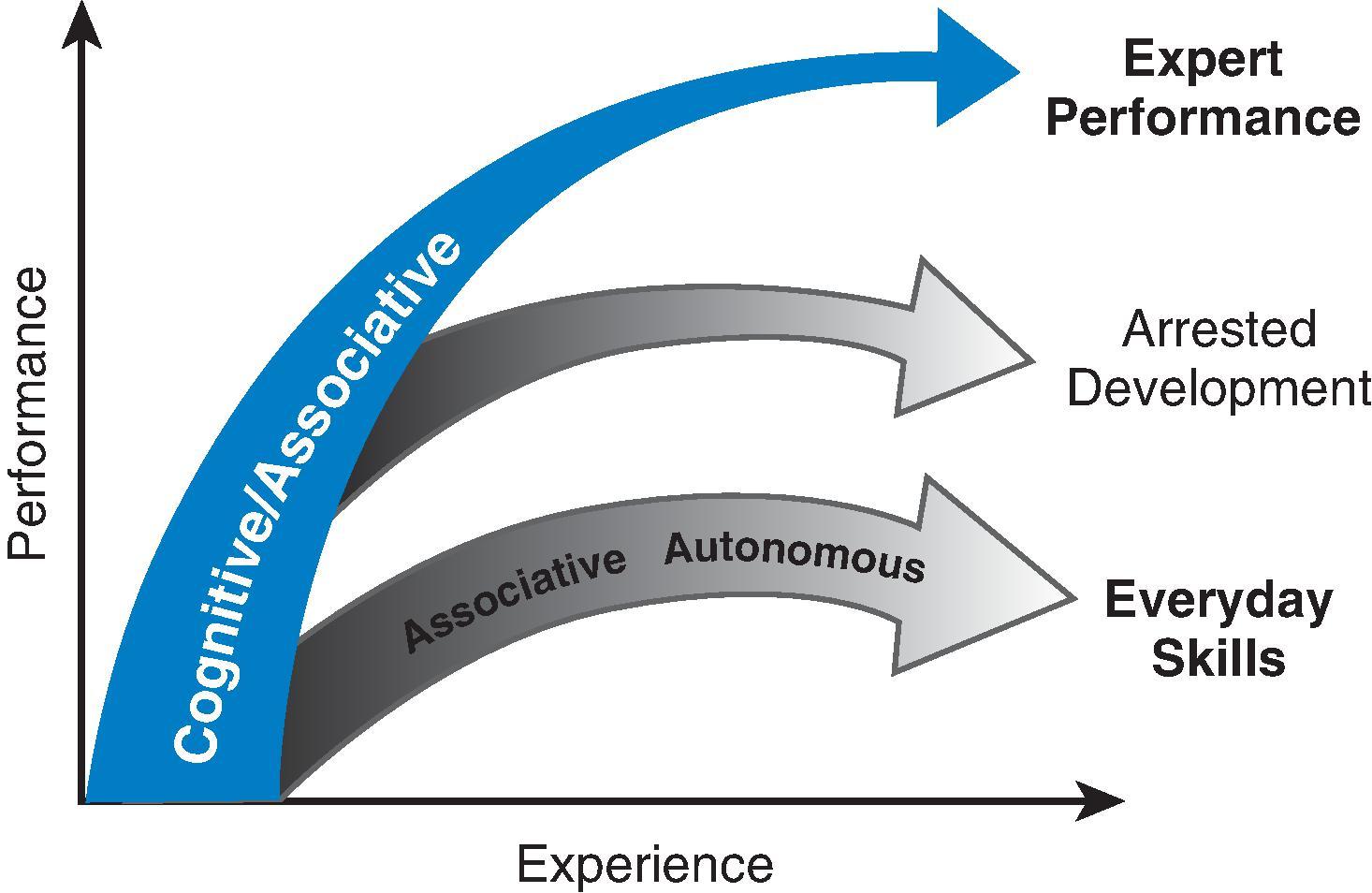
Learning how to use an airway device can initially show rapid improvement. This early formative period is associated with cognitive and associative phases where feedback from mentors, repeated performance, and problem solving are associated with the rapid advancement of ability. Eventually, this advancement tends to plateau, and the learner enters a phase of automaticity. At this stage, the practitioner can perform with little effort, but the development of behavior can stall with little further improvement toward expertise ( Fig. 49.2 ). Experience gained at this stage may decrease the effort of performance by producing automaticity, but this does not necessarily improve the quality of performance. This can be a problem encountered by senior practitioners who mostly compensate by experience, if gained from case load. To break away from automated behavior, the learner should embark on Ericsson’s described “deliberate practice,” where they take on challenges and difficult cases that provide new exposure and push the learner beyond their comfort zone. This process is further enhanced by distributed learning, where new challenging experiences are spread out and occur at regular intervals.
Even with a concerted effort by the learner to engage in deliberate practice, the development of expertise takes time (the so-called 10,000 hours of training or 10 years of clinical practice). Hampered by the constraints of clinical practice, some airway practitioners struggle to achieve the requirements of deliberate practice and distributed learning. Under these circumstances, simulation can play a role in rapidly accelerating the learning experience by providing multiple procedures of varying difficulty in a short time. A study with the AccuTouch bronchoscopy simulator (CAE Montreal, Canada) found that novice residents performed an average of 17 oral virtual flexible bronchoscopy intubations in 39 minutes. These residents were able to increase their dexterity with the flexible bronchoscope after this short exposure.
Internationally, there has been a shift away from the time-based apprenticeship model to competency-based medical education (CBME). Defined quite simply, the words competence and competency can be used as they are defined in the Oxford Dictionary of English, meaning the ability to do something successfully. An example of a CBME curriculum is that adopted by the Australian and New Zealand College of Anaesthetists (ANZCA) or the Anaesthesiology European Training Requirements by the Anaesthesiology Section of the European Union Medical Specialities (EBA UEMS). These curricula define clinical fundamentals and competencies, including airway management. Airway management competencies, including tracheal intubation, SGA use, bag-mask ventilation, flexible scope intubation and flexible bronchoscopy, awake intubation, and emergency airway management (or cannot intubate, cannot oxygenate [CICO]), are part of that clinical fundamental. A series of assessments are used throughout a trainee’s progress to ensure that they have met the criteria to proceed to the next level of training. In order for this system to function there is a requirement for teachers to engage in direct observation, coaching, feedback, and reliable valid assessment. Attendance by specialist anesthesiologists at CICO courses is also encouraged by ANZCA.
CBME has not escaped criticism. Critics suggest that CBME applies primarily to trainees and focuses too much on the development of competencies that some regard as a minimum standard of ability. In airway management our goal should be to educate practitioners to be experts at managing difficult airways. This requires a lifelong commitment to keeping up to date with new knowledge, skills, and techniques. Basic competence may not be enough to reach the standard required of an airway expert in anesthesiology. With the constant barrage of new concepts and devices, trainees and specialists need to be fully versed in the recommendations of current airway management practice guidelines.
Practice guidelines for airway management are usually the result of a detailed analysis of medical literature and a summary of current opinion. The development should follow recognized methodological standards and, wherever possible, be evidence based from reputable sources. They are usually a good resource for teaching content and teaching strategies, provided they are kept up to date with regular reviews.
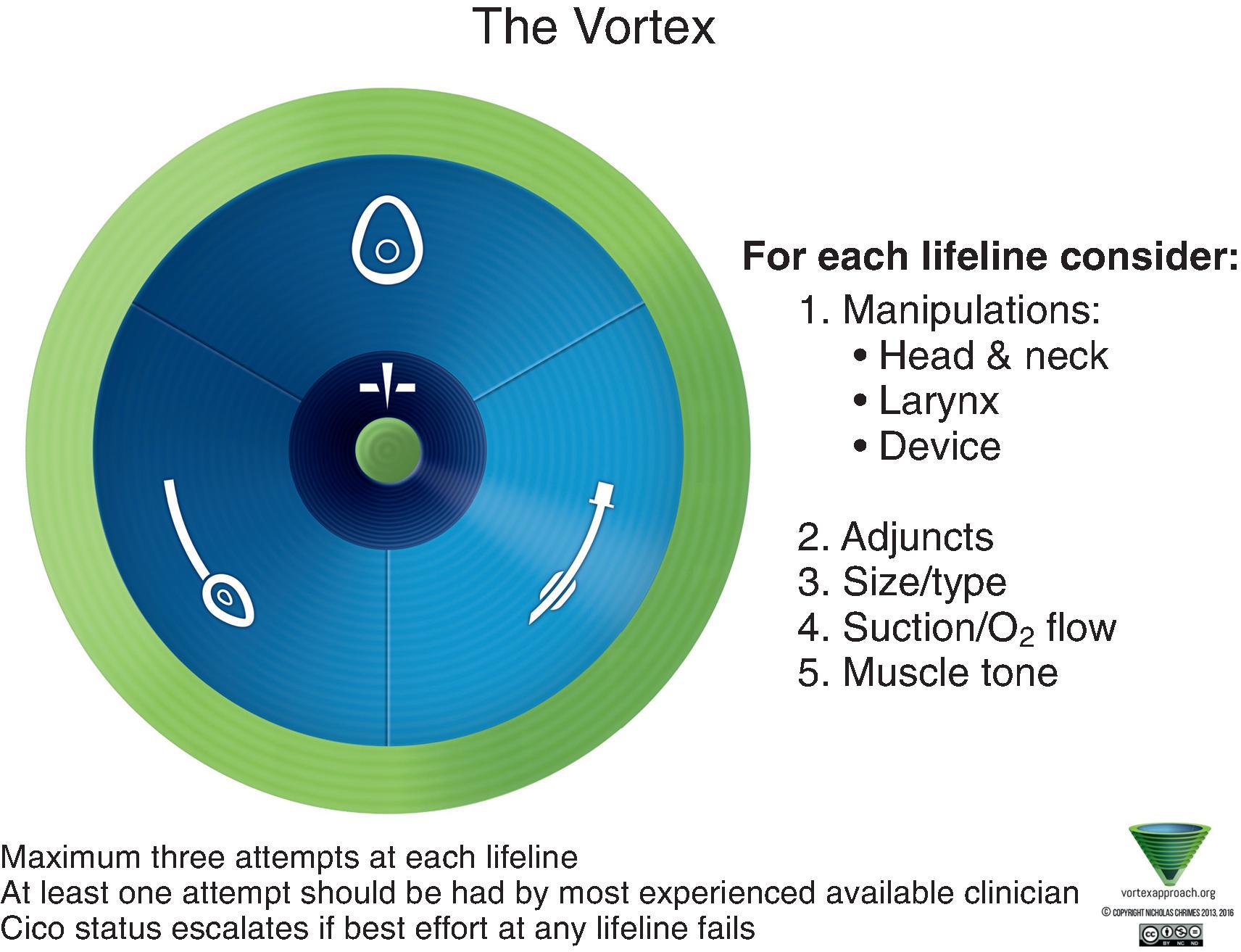
Airway management guidelines often contain algorithms as a form of graphically distilled information derived from the practice guideline and serve as a cognitive aid. The algorithms are not only a useful source of information during didactic teaching sessions, but they are also a great tool during the debriefing of airway simulations, where critical steps and decisions can be discussed and changes in approaches to difficult airways can be rehearsed. In the same manner an algorithm can guide a morbidity and mortality conference on difficult airway management. Due to the complexity of some algorithms, there has been a trend toward simpler cognitive aids, which are used as resources for group simulation sessions as well as applied during clinical cases.
Cognitive aids are prompts, mnemonics, charts, and graphics designed to improve performance, especially during emergencies. An example of an airway management cognitive aid is the Vortex Approach, which prompts the user to progress through each nonsurgical airway technique using a limited number of attempts at each step before improvement or an emergency surgical airway ( Fig. 49.3 ).
Mastery learning is a strict form of CBME where the learner is required to meet predetermined goals before progressing to the next instructional objective. The aim of mastery learning is for learners to achieve a consistent standard and complete all educational goals, irrespective of the time required to reach those goals. At least seven complementary features have been described for mastery learning: (1) baseline or diagnostic assessment; (2) clear learning objectives sequenced as units in increasing difficulty; (3) engagement in powerful and sustained educational activities (e.g., deliberate skills practice, data interpretation, reading) focused on reaching objectives; (4) a fixed minimum passing standard (e.g., test score, checklist percentage); (5) formative assessment with feedback to determine the unit’s completion at the minimum passing standard for mastery; (6) advancement to the next educational unit, given measured achievement, at or above the mastery standard (summative assessment); and (7) continued practice or study on an educational unit until the mastery standard is reached.
A meta-analysis and systematic review was published by Cook et al. on mastery learning for health professionals using technology-enhanced simulation. Results showed that mastery in SBME was associated with large effects on skills but moderate effects on patient outcomes.
The CBME changes introduced by ANZCA and similar colleges and certification boards will inevitably demand more training programs. This increase in airway residency programs or airway fellowships has already occurred within the United States and Canada with associated changes in content and teaching techniques. , These changes place an increased demand for teachers required to instruct trainees and senior practitioners.
The training program should follow a graduated system where training builds on existing knowledge and skills in a stepwise manner, following an agreed syllabus. An example of an airway management syllabus is presented in Table 49.3 . The components of an airway management syllabus might be derived from airway practice guidelines.
|
|
|
|
|
|
Airway training programs typically include a combination of written material, didactic and practical instruction, simulation and clinical training, and assessment of competencies reached. The content of the training program should comply with best practices and ideally correspond with operating procedures and equipment held within the trainee’s hospital ( Table 49.4 ). It is ideal to standardize training and equipment throughout a hospital to focus airway education not only on a variety of devices but much more on the team performance and patient safety issues during training.
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here