Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Human African trypanosomiasis, commonly known as sleeping sickness, is a vector-borne parasitic disease transmitted to humans and animals by the bite of the tsetse fly (genus Glossina ). Infection is caused by protozoa of the genus Trypanosoma and species brucei . In humans, two forms of illness are caused by two distinct subspecies that are morphologically identical but differ in their geographic range and clinical presentations. Trypanosoma brucei gambiense is typically found in West and Central Africa and Trypanosoma brucei rhodesiense in East Africa. T. b. gambiense has a more chronic course, whereas T. b. rhodesiense causes a rapid disease course; both have late stages marked by meningoencephalitis that results in coma and death if untreated. A third subspecies, Trypanosoma brucei , causes chronic infection called nagana in cattle, but humans are not susceptible to this organism. Chagas disease, or American trypanosomiasis, is covered in Chapter 318 .
The surface of the trypanosome is covered by a dense, homogeneous coat of variant surface glycoproteins (VSGs), which are immunodominant. Each individual trypanosome expresses only one VSG at a time but possesses more than 1000 different silent copies of the VSG gene, and switching to a new VSG occurs at a frequency of about 1 per million parasites. Hence, the trypanosomes expressing a given VSG will eventually be cleared by the host’s antibody response, but any individual trypanosome that has switched to a new VSG will evade immune clearance, thereby resulting in a new peak of parasitemia. Recombination between VSG alleles ensures a virtually limitless repertoire of new VSGs, so antibody-mediated parasite eradication is impossible.
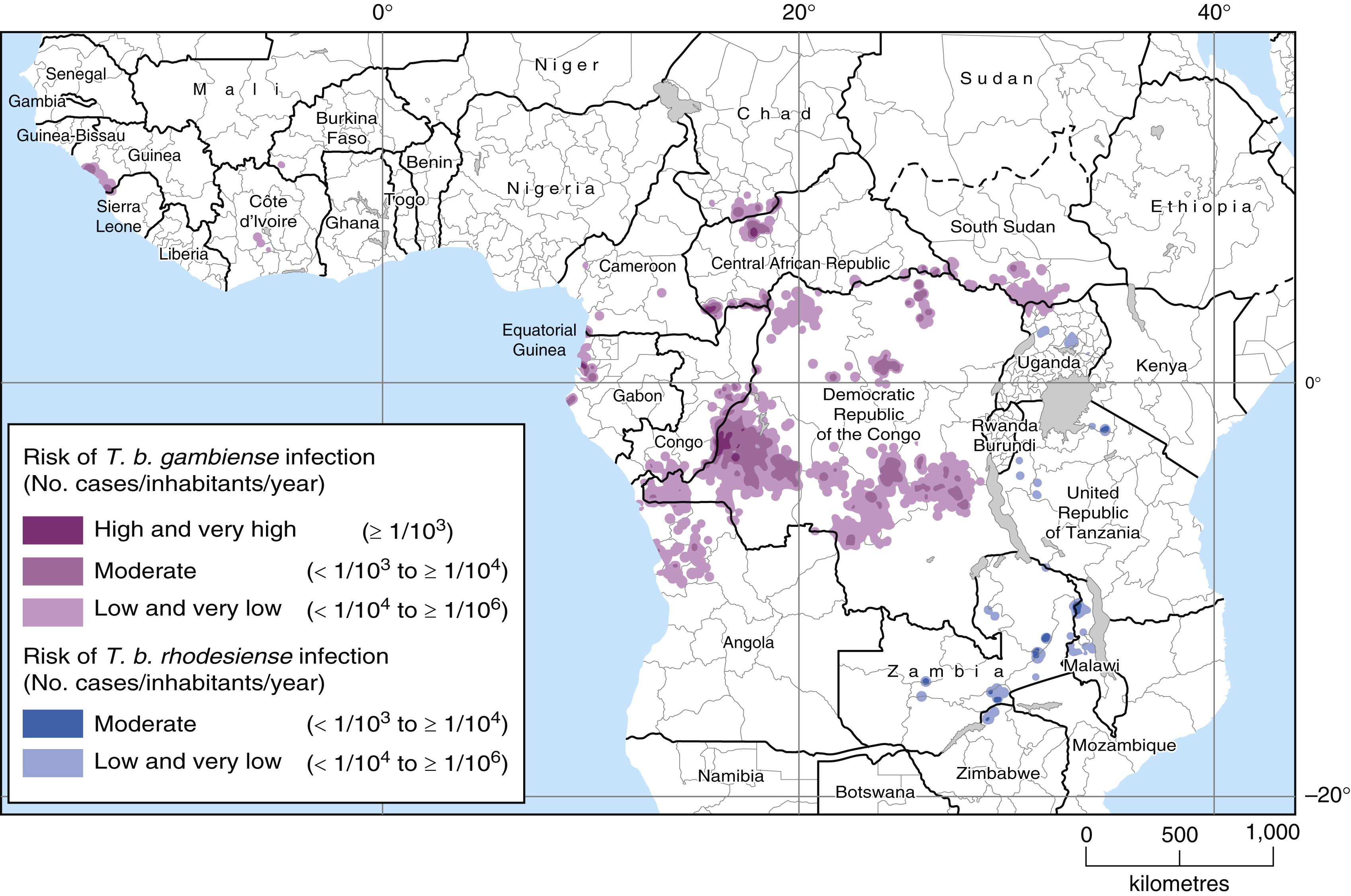
Human African trypanosomiasis is diminishing in importance as a result of increased in public health control efforts. In the past, major epidemics occurred in the Congo basin and Uganda between 1896 and 1906, in numerous endemic countries in the 1920s, and then again in the early 20th century. More recently, however, access of at-risk populations to diagnosis and treatment has led to a dramatic reduction to less than 2000 cases in 2017-2018. Since 2015, more than 90% of reported cases are due to T. b. gambiense , the majority being from the Democratic Republic of the Congo, and less than 100 cases of T. b. rhodesiense have been reported annually since 2015. However, many people are thought to die of human African trypanosomiasis without an accurate diagnosis, and African trypanosomiasis remains a looming threat to an estimated 60 million people who live in tsetse fly–inhabited areas among 36 countries of sub-Saharan Africa.
The geographic distribution includes areas where the vector, parasite, reservoir hosts, and human hosts cohabit ( E-Fig. 317-1 ). In general, these locales include focal areas on the African continent within 15 degrees north and 15 degrees south latitude, with a predilection for wooded rural areas. Humans at greatest risk for infection rely on animal husbandry, agriculture, fishing, and hunting for their livelihoods. Often, disease is concentrated among foci of rural areas, having significant socioeconomic impact on affected villages. With a few exceptions, this infection is never found in urban areas. Fewer than 50 cases are reported annually outside of Africa, usually the result of travel by North Americans or Europeans to African game reserves.
T. b. gambiense is transmitted by tsetse flies from the Glossina palpalis group. Tsetse flies are typically found along riverbanks of wooded areas in the more tropical areas of Central and West Africa. T. b. gambiense is not generally considered a zoonotic disease. The reservoir hosts and the focus of public health campaigns are mainly humans. The role of animal reservoirs for this organism remains undetermined, but natural infections have been reported in domestic animals such as dogs, sheep, cattle, and pigs.
T. b. rhodesiense is transmitted by tsetse flies that belong to the Glossina morsitans group and that are commonly found among woodland and savannah areas of East and Central Africa. T. b. rhodesiense is a zoonotic disease with numerous wild and domestic species of animals acting as reservoirs that sustain the parasite. Domestic species, especially cattle, can drive outbreaks and, as a result, are the focus of successful prevention campaigns.
After the bite of a tsetse fly carrying metacyclic trypomastigotes, a local reaction (chancre) may form at the inoculation site. This sign is seen with T. b. rhodesiense infection and is more frequently observed in travelers, but it is rarely seen with T. b. gambiense infection. Parasites subsequently disseminate into the blood and lymphatic systems in what is considered stage I of the disease. Spread of the parasites into the central nervous system (CNS) defines stage II of the disease, which is invariably fatal if untreated. The parasite appears to remain extracellular throughout the course of infection. As an extracellular microbe, the parasite must evade immune clearance to establish a persistent infection.
Peaks and waves of parasitemia occur during stage I disease and result in the classic symptom of intermittent fever. These bouts of fever correspond to a type 1 inflammatory response ( Chapter 36 ), in which classically activated macrophages produce high levels of tumor necrosis factor (TNF) and nitric oxide. This response helps control the parasitemia but also contributes to tissue damage. Type 2 inflammatory responses with high levels of interleukin-10 then limit the production of TNF and nitric oxide after the initial parasitemia has been controlled. Antibody responses are directed to VSGs and other trypanosome antigens (e.g., antigens from lysed parasites), but autoantibodies are also produced. Generalized febrile episodes are observed in association with lymphadenopathy, myocardial inflammation, and pericardial inflammation. Cardiac involvement is typically more severe with T. b. rhodesiense infection.
In stage II of the disease, parasites cross the blood-brain barrier and invade the CNS. Acute meningoencephalitis develops, and the variety of inflammatory cells that infiltrate the brain include macrophages, lymphocytes, plasma cells, Mott cells (plasma cells with spherical cytoplasmic inclusions composed of immunoglobulin), and morular cells (plasmacytoid cells with transparent hyaline vesicles in the cytoplasm). These inflammatory cells are found in the meninges, which become thickened, as well as in the perivascular spaces and neuropil. Edema, hemorrhage, and granulomatous lesions are often present; thrombosis and neuronal degeneration may also be observed.
Genetic resistance to African sleeping sickness is due to a common (in individuals of African descent) polymorphism in the gene for APOL 1 , which is a component of high-density lipoprotein. This gene product mediates serum resistance to the parasite. An untoward consequence of this polymorphism is that individuals with two copies of the variant allele (15% of African Americans) are at increased risk of chronic kidney disease ( Chapter 107 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here