Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Transcatheter aortic valve implantation (TAVI) may be performed for conditions that are outside the currently labeled indication of symptomatic severe stenosis of trileaflet aortic valve. TAVI in bicuspid aortic stenosis was excluded from the major commercial randomized controlled trials and instead has been investigated in single-arm registries. There is limited experience with TAVI in pure native aortic regurgitation, though dedicated devices are in development. TAVI for failed bioprosthetic valves has been investigated in registries and is an attractive alternative to redo surgery. Additional procedures, such as transcatheter electrosurgical laceration of aortic valve leaflets (BASILICA), may be required to prevent coronary artery obstruction and optimize hemodynamics. Finally, transcatheter valves may be implanted in the mitral and tricuspid positions if certain anatomic considerations are met. This chapter discusses these advanced indications for transcatheter valve implantation.
In the United States, even though bicuspid morphology was an exclusion criterion for the pivotal randomized trials, the Food and Drug Administration (FDA) did not expressly preclude patients with bicuspid aortic stenosis from undergoing TAVI when it was approved, rather adding a precaution to the “Instructions for Use.” This allowed physicians to perform TAVI in bicuspid patients and to accumulate data in the US national Society of Thoracic Surgeons/American College of Cardiology (STS/ACC) Transcatheter Valve Therapy (TVT) registry. The FDA removed the bicuspid valve precaution in 2018 for intermediate- and high-risk patients and in 2020 for low-risk patients.
TAVI has never been tested in a rigorous randomized controlled trial versus surgery in patients with a congenital bicuspid aortic valve.
Nonetheless, a number of multicenter prospective registries have evaluated the safety and effectiveness of TAVI in bicuspid patients—including in low-risk patients who would typically have undergone surgery.
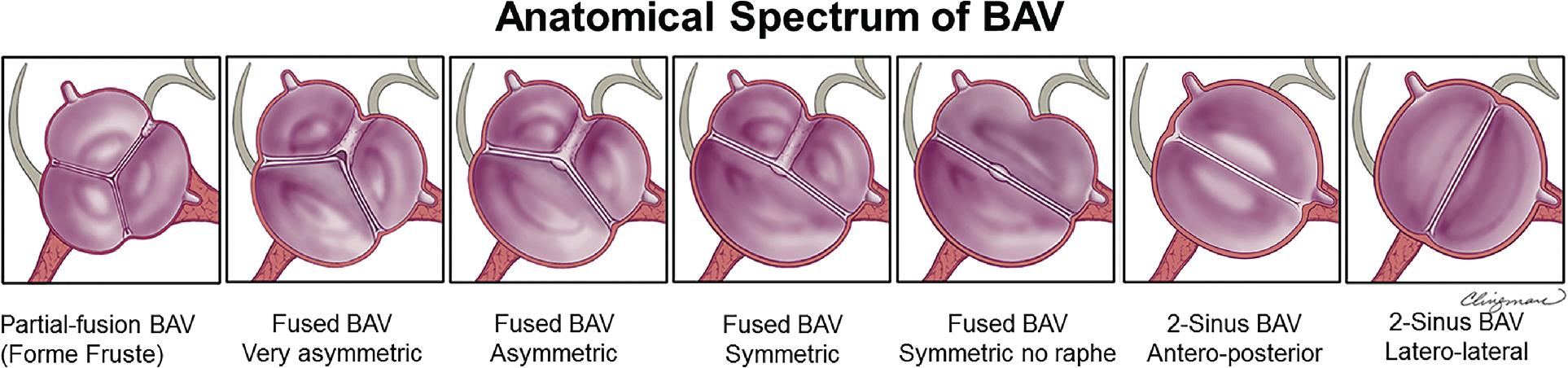
Although bicuspid valve disease often is initially diagnosed on echocardiography, computed tomography (CT) is the best imaging modality to confirm aortic valve morphology (bicuspid vs. tricuspid) and, if applicable, the number of aortic sinuses, leaflet fusion phenotype, presence of a raphe, and pattern of leaflet calcification to plan a TAVI procedure ( Fig. 12.1 ).
A congenital bicuspid valve with only two sinuses and leaflets (no raphe) is the least well represented morphology in the bicuspid TAVI registries. Caution should be taken when extrapolating the results for patients with this type of bicuspid valve.
A major limitation of the STS/ACC TVT registry is that it only includes a checkbox for “bicuspid” and does not collect aortic valve morphologic classification from the preprocedure CT scan ( Table 12.1 ).
| Risk | Authors | Year of Publication | Number of Patients | Type of TAVI Valve | 30 DAYS | 1 YEAR | ||
|---|---|---|---|---|---|---|---|---|
| Death | Stroke | Death | Stroke | |||||
| Extreme, high, and intermediate risk | Makkar et al. [CR] | 2019 | 2691 | BEV | 2.6% | 2.5% | 10.5% | 3.4% |
| Forrest et al. [CR] | 2020 | 932 | SEV | 2.6% | 3.4% | 10.4% | 3.9% | |
| Low risk | Waksman et al. [CR] | 2020 | 72 | BEV and SEV | 0% | 0% b | 1.5% c | 0% b , c |
| Forrest et al. [CR] | 2021 | 150 | SEV | 0.7% | 0.7% b | — | — | |
| Williams et al. a | 2020 | 71 | BEV | 0% | 0% b | 1.4% | 0% b | |
| Williams et al. a | 2020 | 98 | BEV | 0% | 0% b | — | — | |
| Makkar et al. [CR] | 2021 | 3243 | BEV | 1.0% | 1.4% | 4.5% | 2.0% | |
Makkar RR, Yoon S-H, Leon MB, et al. Association between transcatheter aortic valve replacement for bicuspid vs tricuspid aortic stenosis and mortality or stroke. JAMA. 2019;321(22):2193-2202.
Forrest JK, Kaple RK, Ramlawi B, et al. Transcatheter aortic valve replacement in bicuspid versus tricuspid aortic valves from the STS/ACC TVT registry. JACC Cardiovasc Interv. 2020;13(15):1749-1759.
Waksman R, Craig PE, Torguson R, et al. Transcatheter aortic valve replacement in low-risk patients with symptomatic severe bicuspid aortic valve stenosis. JACC Cardiovasc Interv. 2020;13(9):1019-1027.
Forrest JK, Ramlawi B, Deeb GM, et al. Transcatheter aortic valve replacement in low-risk patients with bicuspid aortic valve stenosis. JAMA Cardiol. 2021;6(1):50-57.
Makkar RR, Yoon SH, Chakravarty T, et al. Association between transcatheter aortic valve replacement for bicuspid vs tricuspid aortic stenosis and mortality or stroke among patients at low surgical risk. JAMA. 2021;326(11):1034-1044.
a Oral presentation at Transcatheter Cardiovascular Therapeutics (TCT) Connect online meeting, 2020.
c Oral presentation at Cardiovascular Research Technologies (CRT) Virtual online meeting, 2021.
There are two main schools of thought for sizing TAVI valves in the setting of bicuspid aortic stenosis ( Fig. 12.2 ).
The first uses the same annular sizing algorithms for the commercially available transcatheter aortic valves (based on either annular perimeter or area measurement).
The second uses measurements above the true aortic annulus toward the leaflet tips (so-called “supraannular sizing”), which typically results in smaller perimeters and areas and may lead to downsizing the implanted transcatheter aortic valve.
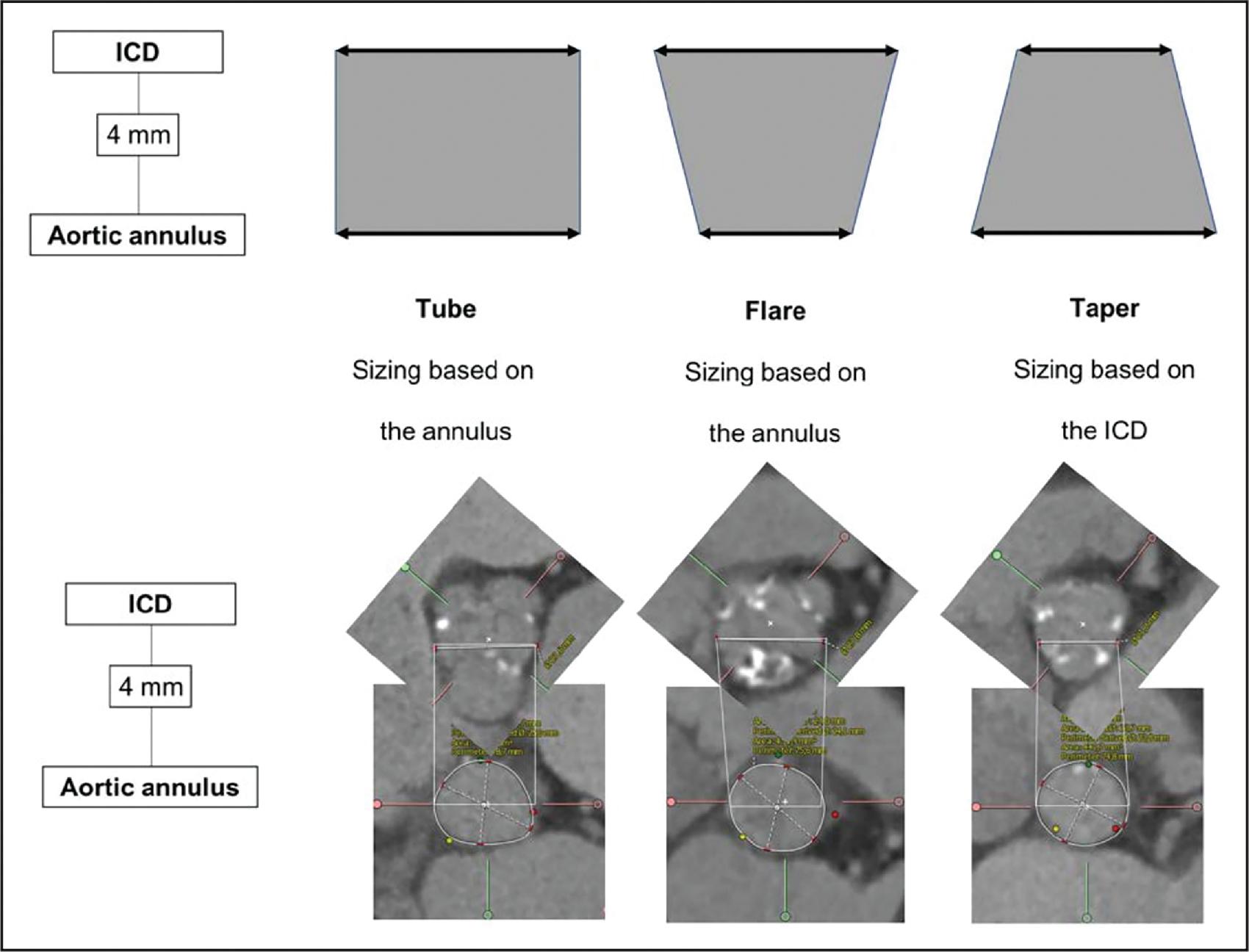
A number of groups have attempted to compare the two methodologies. On balance of evidence, there is probably no clinically meaningful difference in procedural success rates or clinical outcomes. The conventional annular methodology is more reproducible and therefore remains the most widely used.
Bicuspid aortic stenosis is often associated with heavy-to-extreme calcification of the leaflets, raphe, annulus, and/or left ventricular outflow tract (LVOT).
There is some evidence that extreme leaflet plus raphe calcification is associated with increased aortic root injury, moderate-to-severe paravalvular leak, and both short- and long-term mortality.
In young patients with severe calcification, surgery should be reconsidered as these patients probably experience more paravalvular leak and require more permanent pacemakers.
Finally, bicuspid aortic stenosis often goes hand in hand with ascending aortopathy. If a young patient meets criteria for ascending aorta replacement, the patient should preferentially undergo surgery rather than TAVI.
Early experience with TAVI comparing outcomes in patients with bicuspid versus tricuspid aortic stenosis demonstrated higher rates of aortic root injury when using a balloon-expandable valve, and higher rates of moderate-to-severe paravalvular leak when using a self-expanding valve.
More contemporary analyses from the STS/ACC TVT registry using the latest-generation TAVI valves demonstrated equivalent outcomes using both balloon-expandable and self-expanding valves.
Using the balloon-expandable SAPIEN 3 valve (Edwards Lifesciences, Irvine, CA) there was no significant difference in 30-day or 1-year mortality but there was a signal for increased stroke at 30 days.
Using the self-expanding CoreValve Evolut valve (Medtronic, Minneapolis, MN), all-cause mortality, stroke, and valve hemodynamics did not differ at 30 days or 1 year between groups. More recent data in low-risk patients undergoing TAVI for bicuspid aortic stenosis have demonstrated excellent clinical outcomes at 30 days and 1 year (see Table 12.1 ).
One theoretical concern with TAVI in the setting of bicuspid stenosis is the inability of the transcatheter aortic valve metallic frame to fully expand to its intended shape and size, which in turn may affect leaflet function and durability. In practice, we find that the balloon-expandable valve typically achieves a mostly circular configuration in all but the most extreme calcification cases.
The self-expanding valve is more often constrained at the annulus with an elliptical inflow, but at the level of the supraannular leaflets the valve is circular, which should guarantee normal leaflet function.
Further data are required on TAVI durability in patients with bicuspid, particularly those with Sievers type 0 morphology or type 1/2 with raphe in whom annulus ellipticity, thickened and stiffened leaflets, and heavy calcification are common. Indeed, some reports show reduced procedural success rates with type 0 valves.
Subclinical leaflet thrombosis has been observed in a similar proportion of bicuspid TAVI patients at 30 days but does not appear to be associated with clinical events.
Longer follow-up is needed to determine whether leaflet thrombosis affects valve durability.
In most respects, the actual TAVI implantation technique is no different with bicuspid aortic stenosis compared with tricuspid aortic stenosis.
It may be more difficult to determine the optimal coplanar implantation view using CT when there are only two sinuses.
Most operators agree that routine predilation is preferable in bicuspid TAVI. The aims are twofold:
Ease deliverability of the TAVI valve between the stenosed bicuspid aortic valve leaflets
Maximize expansion of the valve frame (particularly with self-expanding TAVI valves)
Few data are available on long-term outcomes after TAVI for bicuspid aortic stenosis. The large US multicenter STS/ACC TVT registry does not collect outcomes beyond 1 year. The low-risk bicuspid registries embedded in the pivotal low-risk trials will follow patients for up to 10 years so these data will become available in the future.
Commercially available TAVI valves are not indicated for isolated native aortic regurgitation. This does not mean that TAVI is not feasible in this setting, but dedicated devices are needed with the main challenge being anchoring the TAVI valve in the annulus.
Most commercial valves rely on outward radial force against a calcified annulus, which is not present in the setting of isolated aortic regurgitation, for anchoring.
For this reason, outside of clinical trials testing novel TAVI valves designed for aortic regurgitation, surgery remains the therapy of choice for patients with isolated native aortic regurgitation.
In contrast:
TAVI is an excellent solution for failing bioprosthetic surgical aortic valves, homografts, or stentless valves where the predominant lesion is aortic regurgitation because the surgical ring and or calcified root/surgical suture line provides sufficient anchoring for the TAVI valve.
TAVI is also a good solution for patients with degenerative calcific mixed aortic stenosis and regurgitation because the calcified aortic annulus provides sufficient anchoring for the TAVI valve.
Finally, TAVI may be a solution for patients with paravalvular leak around a surgical or transcatheter bioprosthesis, wherein the sealing skirt TAVI valve is positioned within the LVOT just below the old valve, or the radial force of the new TAVI valve is used to further expand the underexpanded metallic frame of the old TAVI valve around which the paravalvular leak occurs.
One particularly challenging patient group is those with left ventricular assist devices (LVADs) and associated aortic regurgitation, in whom TAVI has been shown to be reasonably effective, albeit with significant associated morbidity ( Table 12.2 ).
| Authors | Year of Publication | Number of Patients | Type of TAVI Valve | 30-Day Mortality | 1-Year Mortality |
|---|---|---|---|---|---|
| Yehya et al. [CR] | 2019 | 9 (LVAD patients) | SEV | 0% | 44% |
| Yoon et al. [CR] | 2017 | 331 | BEV and SEV | 10.9% | 24.1% |
| De Backer et al. [CR] | 2018 | 254 | SEV | 11.7% | n/a |
| Rawasia et al. [CR] , a | 2019 | 998 (meta-analysis) | BEV and SEV | 11.9% | n/a |
| Anwaruddin et al. [CR] , a | 2019 | 230 | SEV | 13.3% | n/a |
Yehya A, Rajagopal V, Meduri C, et al. Short-term results with transcatheter aortic valve replacement for treatment of left ventricular assist device patients with symptomatic aortic insufficiency. J Heart Lung Transplant. 2019;38(9):920-926.
Yoon SH, Schmidt T, Bleiziffer S, et al. Transcatheter aortic valve replacement in pure native aortic valve regurgitation. J Am Coll Cardiol. 2017;70(22):2752-2763.
De Backer O, Pilgrim T, Simonato M, et al. Usefulness of transcatheter aortic valve implantation for treatment of pure native aortic valve regurgitation. Am J Cardiol. 2018;122(6):1028-1035.
Rawasia WF, Khan MS, Usman MS, et al. Safety and efficacy of transcatheter aortic valve replacement for native aortic valve regurgitation: a systematic review and meta-analysis. Catheter Cardiovasc Interv. 2019;93(2):345-353.
Anwaruddin S, Desai ND, Szeto WY, et al. Self-expanding valve system for treatment of native aortic regurgitation by transcatheter aortic valve implantation (from the STS/ACC TVT registry). Am J Cardiol. 2019;124(5):781-788.
a Some overlap of patient populations may exist between studies.
In most respects, preprocedural evaluation is no different than for patients undergoing TAVI for aortic regurgitation compared with patients with aortic stenosis. However, isolated native aortic regurgitation is often associated with aortic root dilation and therefore aortic annular dimensions may exceed the upper recommended limit of the transcatheter aortic valve instructions for use. For those patients whose annulus does fall within the recommended range, oversizing of the TAVI valve is routinely practiced to improve valve anchoring in the noncalcified annulus.
Several registries and meta-analyses reported rather disappointing clinical outcomes using early-generation commercially available TAVI valves with high rates of paravalvular leak, need for more than one valve implantation, rates of valve migration or embolization, and rates of permanent pacemaker implantation (see Table 12.2 ). These same registries and meta-analyses demonstrated better results using newer-generation valves. The difference is likely multifactorial.
First, improvements in valve technology, in particular the inclusion of sealing skirts, likely reduced paravalvular leaks.
Second, systematic CT measurements likely improved valve sizing.
Third, oversizing algorithms likely improved valve anchoring and reduced migrations and embolizations.
And fourth, procedural techniques targeting shallower implantation depth likely reduced permanent pacemaker requirements.
Most agree that the ideal solution will be dedicated TAVI valves for treatment of aortic regurgitation. Two valves that achieve anchoring by “clipping” onto the leaflets of the regurgitant aortic valve have been tested in patients with isolated native aortic regurgitation: the JenaValve and the J-Valve. Initially implanted via transapical approach, the latest transfemoral version of the JenaValve is currently undergoing clinical evaluation in the United States.
Procedural steps for the implantation of commercially available TAVI valves (designed to treat aortic stenosis) are essentially the same in the setting of isolated native aortic regurgitation.
Caution should be used during valve positioning as migration/embolization toward the ventricle or into the aorta is more common, particularly when using oversized valves.
Procedural steps for the implantation of the dedicated valves that “clip” onto the aortic valve leaflets are distinct and specific to each device.
It is important to emphasize that these valves remain investigational in the United States to date.
In published series of TAVI for isolated native aortic regurgitation, the need for a second valve because of persistent aortic regurgitation was as high as 25%. However, rates are lower with newer-generation valves. Need for permanent pacemaker is higher after TAVI for isolated aortic regurgitation than for aortic stenosis, with reported rates of up to 20%. This rate does not appear to have fallen with newer-generation valves. The etiology is likely multifactorial, but valve oversizing is likely part of the problem. Permanent pacemaker rates with the dedicated valves that anchor by “clipping” onto the aortic valve leaflets may be lower because they exert less outward mechanical force onto the annulus, outflow tract, membranous septum, and underlying conduction system.
Very few data are available on long-term outcomes after TAVI for isolated aortic regurgitation because it is either performed off-label using commercially available TAVI valves that are intended to treat aortic stenosis, or because the investigational valves designed to treat isolated aortic regurgitation are still in the early phases of their clinical evaluation (see Table 12.2 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here