Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Adrenal masses may be neoplastic, infectious, or hemorrhagic ( Box 71-1 ). Neoplasia is the most common cause for an adrenal mass seen on imaging. An incidentally detected adrenal mass as well as an adrenal mass in a patient with known malignancy elsewhere is most commonly due to a benign adenoma.
In one large autopsy series of more than 1000 patients, an incidence was reported of 1.4% to 5.7% with an adrenal mass. However, adrenal masses are increasingly being encountered on cross-sectional imaging done for evaluation of both abdominal symptoms and cancer staging. The overall prevalence of adrenal masses on computed tomography (CT) approaches 3% in middle age and increases to as much as 10% in the elderly.
The imaging features of adrenal masses are listed in Table 71-1 .
| Adrenal Masses | Adenoma (Lipid-Rich) | Adenoma (Lipid-Poor) | Myelolipoma | Pheochromocytoma | Metastasis | Carcinoma | Neuroblastoma | Ganglioneuroma | Cyst | Hematoma |
|---|---|---|---|---|---|---|---|---|---|---|
| Size | Small, usually <3 cm | Small, usually <3 cm | Usually <3 cm | Large, >3 cm | Variable | Large, >4 cm | Large, >4 cm | Large, >4 cm | Large, >3 cm | Variable |
| Shape | Round or oval | Round or oval | Round or oval | Round or oval | Oval or irregular | Irregular | Irregular | Oval or irregular | Round or oval | Round or oval |
| Margins | Smooth | Smooth | Smooth | Well defined | Ill defined | Ill-defined | Ill-defined | Variable | Smooth | Variable |
| Consistency | Homogeneous | Homogeneous | Heterogeneous | Heterogeneous | Heterogeneous | Heterogeneous | Heterogeneous | Heterogeneous | Homogeneous | Heterogeneous |
| Computed tomography | ||||||||||
| Unenhanced | <10 HU | >10 HU | <−50 HU | >10 HU | >10 HU | >10 HU, ± calcification | >10 HU, ± calcification | >10 HU, ± calcification | 10 to 20 HU | Variable, acute >50 HU |
| Enhanced | Mild enhancement | Mild enhancement | No to mild enhancement | Intense enhancement | Moderate to intense enhancement | Variable enhancement and necrotic areas | Variable enhancement | Variable enhancement | No enhancement | No enhancement |
| Washout | RPW ≥40% | RPW ≥40% | Variable | RPW ≤40% | RPW ≤40% | RPW ≤ 40% | Variable | Variable | No washout | No washout |
| APW ≥60% | APW ≥60% | APW ≤60% | APW ≤60% | APW ≤ 60% | ||||||
| Magnetic resonance imaging | ||||||||||
| T1 | Iso to hypo | Iso to hypo | Hyper | Iso to hypo | Iso to hypo | Iso to hypo | Iso to hypo | Iso to hypo | Hypo | Hyper or hypo |
| T2 | Iso to mild hyper | Iso to mild hyper | Iso to hypo | Intense hyper in 70% | Hyper | Hyper | Hyper | Hyper | Hyper | Hypo |
| Chemical shift | >20% drop in SI | <20% drop in SI | India ink artifact around the macroscopic fat | No drop in SI | No drop in SI | No drop in SI | No drop in SI | No drop in SI | No drop in SI | No drop in SI |
| Post Gd-T1 | Nonspecific | Nonspecific | No or heterogeneous enhancement | Intense enhancement | Mild to moderate enhancement | Heterogeneous enhancement | Heterogeneous enhancement | Heterogeneous enhancement | No enhancement | No enhancement |
| Positron emission tomography | ≤Liver uptake | ≤Liver uptake | ≤Liver uptake | ≤Liver uptake | ≥Liver uptake | ≥Liver uptake | ≥Liver uptake | ≥Liver uptake | ≤Liver uptake | ≤Liver uptake |
| ≤4 SUV | ≤4 SUV | ≤4 SUV | ≤4 SUV | ≥4 SUV | ≥4 SUV | ≥4 SUV | ≥4 SUV | ≤4 SUV | ≤4 SUV |
Adrenal cortical adenomas are common benign tumors arising from the cortex of the adrenal gland. The majority of adrenal adenomas are nonfunctional incidentalomas. A small percentage of adenomas that produce excessive steroid hormones will cause symptoms manifesting as Cushing's syndrome or Conn's syndrome or with excess acne and hair growth. Therefore, all incidentally detected adenomas or adrenal masses on imaging should be correlated with the clinical presentation and, if necessary, serum and urine biochemical analysis for the presence of a functional adenoma. The overall prevalence of adrenal adenomas increases with advancing age.
Computed tomography (CT) is the primary imaging modality used in establishing a diagnosis of adenoma. Histologically, two types of adrenal cortical adenomas are identified: those that contain a high percentage of intracytoplasmic lipid (lipid rich), which represent approximately 70% of all adrenal cortical adenomas, and those that are lipid poor, which represent the remaining approximately 30%. Calcifications, necrosis, and hemorrhage are atypical but can occur, especially in larger lesions. The vast majority of lipid-rich adenomas can be accurately identified by CT density. Typically, adenomas demonstrate a density of less than 10 Hounsfield units (HU) on unenhanced images ( Figure 71-1, A ). Approximately 10% to 40% of all adenomas demonstrate CT density greater than 10 HU and are considered lipid-poor adenomas. Some of the lipid-poor adenomas can be characterized on washout characteristics on delayed-phase contrast-enhanced images. On analysis of washout characteristics, adenomas have relative percentage washout (RPW) and absolute percentage washout (APW) values of more than 38% and 52%, respectively, after a 10-minute delay or 40% and 60%, respectively, after a 15-minute delay. These washout patterns are diagnostic for adenoma. Both lipid-rich and lipid-poor adenomas have a similar washout pattern.
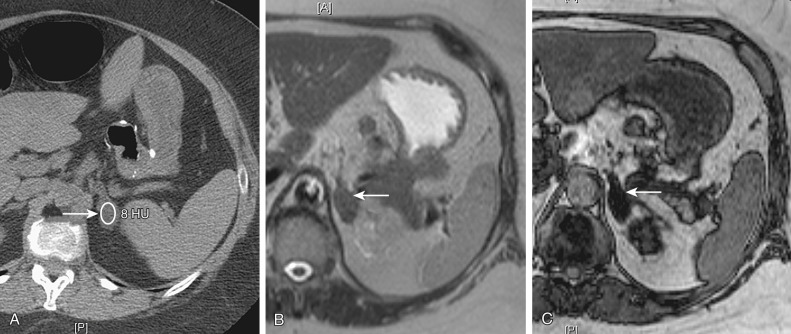
Adenomas on T1-weighted, T2-weighted, and post–gadolinium-enhanced T1-weighted imaging have varied signal intensity and, consequently, these sequences are generally not used for characterization. The most important and specific finding of lipid-rich adenoma on magnetic resonance imaging (MRI) is signal “drop out” on out-of-phase (opposed-phase) imaging compared with in-phase imaging on chemical-shift T1-weighted images (see Figure 71-1, B and C ). A signal drop of more than 20% has a sensitivity of 71% and a specificity of 100%. Again, lipid-poor adenomas may not be accurately characterized on MRI.
Ultrasonography has very limited role.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here