Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acquired disorders of the stomach in children are uncommon and may be the result of an underlying congenital predisposition, such as gastric volvulus; an inflammatory process, such as peptic ulcer disease (PUD); or a neoplastic or neoplastic-like condition. In addition to fluoroscopic contrast studies, ultrasonography (US), computed tomography (CT), and, less frequently, magnetic resonance imaging (MRI) and nuclear medicine may be used for evaluation.
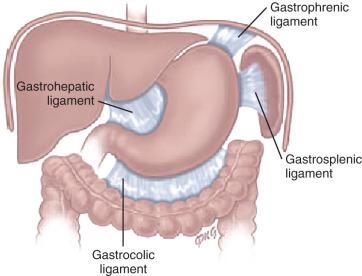
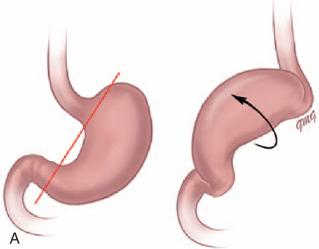
The stomach is normally fixed in the peritoneal cavity at the gastroesophageal (GE) junction and by the gastrohepatic, gastrosplenic, gastrocolic, and gastrophrenic ligaments ( Fig. 101.1 ). Gastric volvulus is defined as an abnormal rotation of the stomach of more than 180 degrees around its long (organoaxial) or short (mesenteroaxial) axes ( Figs. 101.2A and B ). In the organoaxial type of gastric volvulus, there is an inversion of the position of the greater and lesser curves of the stomach, with the greater curvature positioned to the right and superior to the lesser curvature. In the mesenteroaxial type, the stomach rotates on its short axis, leading to a reversal of the relationship between the gastroesophageal junction and the antrum.
Clinically, there are two primary scenarios. The first is the acute fulminant presentation, most often encountered in the mesenteroaxial type, with sudden and persistent vomiting and acute abdominal pain. The chronic intermittent presentation is more often associated with the organoaxial type, with less specific symptoms including recurrent abdominal pain, vomiting, and gastric distension. Predisposing factors for gastric volvulus include congenital or acquired absence of one or more of the fixating ligaments as isolated abnormalities, or occurring in association with a diaphragmatic defect, wandering spleen, or heterotaxy syndrome.
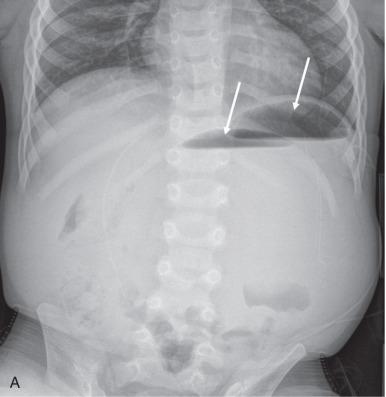
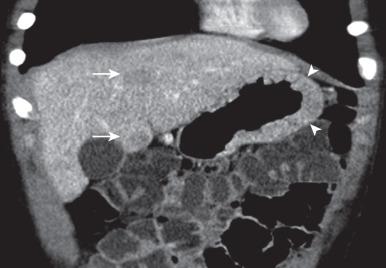
Abdominal radiographs in patients with gastric volvulus typically show marked gastric distension, often with a very unusual, “rounded” outline, or two air fluid levels on an upright view, with paucity of distal bowel gas indicating gastric outlet obstruction ( Fig. 101.3A ). Other findings include an unusual nasogastric tube course or diaphragmatic elevation. While plain radiographs are usually highly suggestive of the diagnosis, CT may be diagnostic in demonstrating the abnormal orientation and obstruction of the stomach and may detect the presence of heterotaxy or a wandering spleen ( Fig. 101.3B ). Upper gastrointestinal (UGI) confirms the presence of gastric outlet obstruction and characterizes the type of gastric volvulus present ( Fig. 101.3C ). As noted earlier, in organoaxial volvulus, there is an inversion of the relationship of the greater and lesser curvatures, while in mesenteroaxial volvulus, the antrum and pylorus projects over the gastric fundus at the level of the GE junction; mixed types can also occur.
Gastropexy is the treatment of choice and can be performed laparoscopically.
Perforation of the stomach is an uncommon event, mainly seen in preterm and full-term neonates as a cause of massive pneumoperitoneum. Potential etiologies include nasal ventilation, distal intestinal obstruction, ischemia, corticosteroid administration, or a combination of factors ; infants with esophageal atresia and distal fistula born prematurely are at particular risk if the diagnosis is not known before ventilatory support is instituted. Concomitant necrotizing enterocolitis has also been described. Beyond the neonatal period, perforation is rare and usually secondary to trauma such as iatrogenic insertion of tubes and catheters, surgery such as fundoplication, caustic ingestion, or PUD.
The most common presenting manifestations of perforation include sudden onset of abdominal distension, ileus, respiratory distress, and, less frequently, cyanosis, fever, vomiting, and bloody stool.
Abdominal radiography is the imaging method of choice when perforation of the GI tract is suspected. As in other locations of GI perforation, abdominal radiographs will typically demonstrate free intraperitoneal air.
Gastric perforations require surgical repair. A higher mortality rate is seen in preterm and low birth weight infants who present with gastric perforation.
Gastritis is a nonspecific term referring to conditions that result in inflammation of the gastric mucosa, such as PUD and/or Helicobacter pylori infection. In children, inflammatory changes in the stomach may also be the result of immunologic alterations (eosinophilic gastritis) or be related to other systemic entities such as Crohn disease or chronic granulomatous disease. Gastropathy is a disorder of the gastric mucosa that may demonstrate evidence of epithelial damage and regeneration but has little to no associated inflammatory change as seen in hypertrophic gastropathy (Menetrier disease).
PUD occurs less commonly in children than adults and, when seen, presents with duodenal ulceration more frequently than gastric ulceration (see Chapter 103 ). The two main risk factors for PUD in children are Helicobacter pylori infection and nonsteroidal antiinflammatory medications. Helicobacter pylori , a common human pathogen, is associated with both inflammatory conditions (chronic gastritis and PUD) and malignancy (gastric MALT “mucosa-associated lymphoid tissue” lymphoma). Zollinger-Ellison syndrome results in PUD, with multiple, recurrent ulcerations seen in the distal duodenum and proximal jejunum due to the increased acid production generated by a gastrin-secreting tumor ( Fig. 101.4 ).
Symptoms of ulcer disease are varied and include abdominal pain, anorexia, early satiety, recurrent vomiting, and anemia. In a few patients, PUD may result in severe gastrointestinal hemorrhage or acute abdominal pain due to perforation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here