Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Neuroblastoma is the most common extracranial solid neoplasm in children and accounts for almost 10% of all childhood neoplasms. Neuroblastoma arises in the abdomen in two-thirds of cases; of these, about two-thirds of lesions occur in the adrenal gland, whereas the remainder may arise anywhere along the sympathetic nerve chains.
Neuroblastoma, ganglioneuroblastoma, and ganglioneuroma belong to a group of related neurogenic neoplasms arising from neural crest tissue that are distinguished by their degree of cellular maturation and differentiation. Neuroblastoma accounts for the vast majority and has the most primitive and malignant cells. Ganglioneuroma represents the most differentiated end of the spectrum and is benign. Ganglioneuroblastomas represent an intermediate group with mixed histology and behavior.
Most children with neuroblastoma present between 1 and 5 years of age, with a median age of almost 2 years, although tumors may be uncommonly congenital and present at birth. Neuroblastoma is more common in patients with neurofibromatosis type 1, Beckwith-Wiedemann syndrome, Hirschsprung disease, central hypoventilation syndrome, and DiGeorge syndrome.
Neuroblastomas typically present as palpable masses or with symptoms and signs related to local tumor invasion, metastatic disease, and the effects of hormone production (e.g., catecholamines) or autoimmune response (opsoclonus-myoclonus syndrome). Metastatic disease is seen in up to 70% of patients at presentation. The most common sites include local and distant lymph nodes, bone, bone marrow, liver, and skin.
The diagnosis of neuroblastoma can be made by tissue biopsy, but a combination of positive bone marrow aspirate and increased urinary catecholamine metabolites (vanillylmandelic acid and homovanillic acid) is sufficient to confirm the diagnosis. The urinary level of catecholamine metabolites is increased in almost 90% of cases of neuroblastoma. The International Neuroblastoma Staging System has been the most commonly used worldwide for staging neuroblastoma. However, its application has encountered many difficulties, as it relies on the extent of tumor resected at surgery. For this reason, the International Neuroblastoma Risk Group Staging System was developed in 2009 and relies on preoperative imaging findings and detection of metastatic disease. Specific involvement of vital structures represent image-defined risk factors (IDRFs) and upstage tumors from L1 to L2 ( Box 122.1 ). In general, IDRFs represent encasement of vessels and nerves, contiguous organ invasion or significant intraspinal extension, airway compression, and tumor in more than one body compartment ( Box 122.2 ).
Stage L1: Localized tumor confined to one body compartment without involvement of vital structures (no image-defined risk factor [IDRF])
Stage L2: Locoregional tumor with at least one IDRF
Stage M: Distant metastasis (excluding stage MS)
Stage MS: Child <18 months of age with metastasis confined to skin, liver, and/or bone marrow
Ipsilateral tumor extension into another body compartment
Neck-chest, chest-abdomen, abdomen-pelvis
Neck
Major artery or vein encasement
Skull base extension
Tracheal compression
Thorax
Brachial plexus or major vessel encasement
Tracheal or principal bronchial compression
Costovertebral junction invasion between T9 and T12
Abdomen and Pelvis
Porta hepatis or hepatodeuodenal ligament invasion
Superior mesenteric artery origin or proximal branch encasement
Aorta, inferior vena cava, celiac axis, or iliac vessel encasement
Pelvic tumor crossing sciatic notch
Intraspinal extension with >⅓ of spinal canal invaded, or perimedullary leptomeningeal spaces effaced, or abnormal spinal cord signal
Adjacent organ infiltration
Including liver, kidney, pancreas, duodenum, diaphragm, mesentery, pericardium
Note: vessel encasement is defined as ≥50% circumference contact or complete compression of venous lumen.
The prognosis of neuroblastoma depends on stage at presentation, patient's age (children younger than 12 to 18 months have better prognosis), histologic category, grade of tumor differentiation, status of the MYCN oncogene, chromosome 11q status, and deoxyribonucleic acid ploidy.
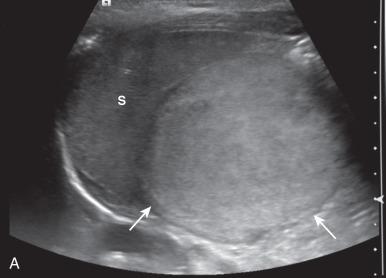
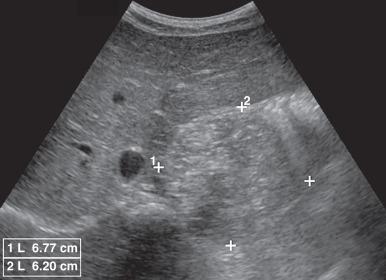
Adrenal neuroblastomas and those arising from the adjacent retroperitoneum are usually easily identified with ultrasound (US), computed tomography (CT), or magnetic resonance imaging (MRI) because the mass is generally quite large by the time of presentation ( Fig. 122.1 ). Very small masses are uncommon, and in those cases seen beyond the neonatal age, CT and MRI play a more important role than ultrasonography ( Fig. 122.2 and e-Fig. 122.3 ). The masses have a variety of appearances by US with the most characteristic being that of a solid, heterogeneous, hyperechoic mass, often with small hyperechoic calcifications with or without posterior acoustic shadowing ( Fig. 122.4 and e-Fig. 122.5 ). Anechoic areas resulting from cystic, hemorrhagic, or necrotic changes may be present ( e-Fig. 122.6 ).
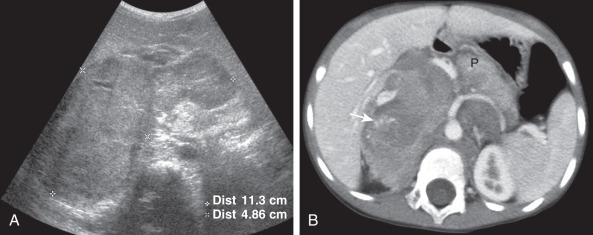
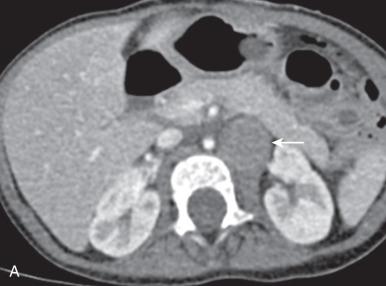
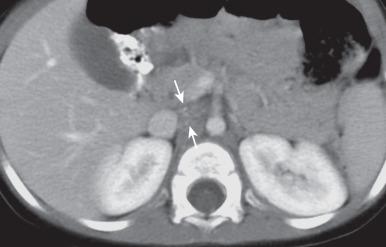
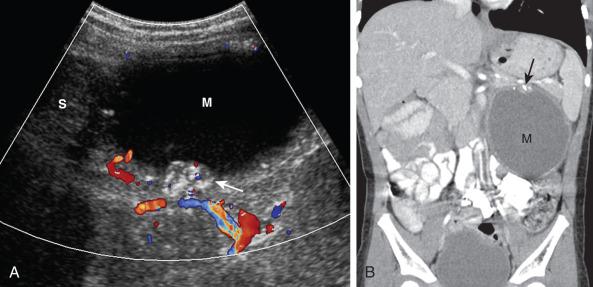
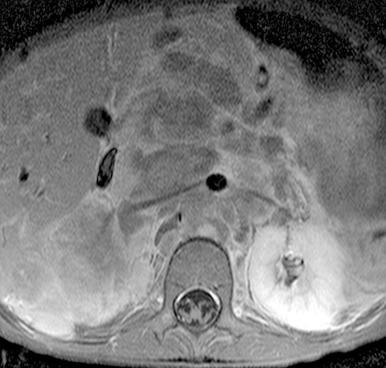
The new International Neuroblastoma Risk Group Staging System requires the use of CT, MRI, or both for staging. On CT, neuroblastomas usually show heterogeneous enhancement, depicting solid areas along with areas of necrosis, hemorrhage, and cystic change (see Fig. 122.1 ). Calcification is present in more than 90% of cases (see Fig. 122.1 and e-Fig. 122.6 ). On MRI, the lesions are usually heterogeneous, with predominantly low signal on T1-weighted images and high signal on T2-weighted images, and with variable degrees of enhancement ( Fig. 122.7 ).
A characteristic imaging feature of neuroblastoma is the displacement of adjacent organs and the displacement or encasement of adjacent major vessels (see Figs. 122.1 and 122.7 ). Local spread may be to lymph nodes. Less frequently, direct invasion into the kidneys ( Fig. 122.8 ) or liver may occur, and the tumor may extend into the spinal canal.

Neuroblastoma liver metastases may be single or multiple nodules, or may present with an infiltrative pattern, particularly in neonates ( Fig. 122.9 ) (see Chapter 121 ). Metastases to bone are best identified with metaiodobenzylguanidine (MIBG) scintigraphy.
![Figure 122.9, Metastatic liver disease in neuroblastoma in an 8-day-old girl (stage MS [formerly 4S]). Figure 122.9, Metastatic liver disease in neuroblastoma in an 8-day-old girl (stage MS [formerly 4S]).](https://storage.googleapis.com/dl.dentistrykey.com/clinical/AcquiredConditions/8_3s20B9780323497480001222.jpg)
If the lesion responds to chemotherapy, the mass regresses and shrinks to a very small amount of soft tissue that often becomes calcified. Certain neuroblastomas in very young children, including individuals with metastatic disease, may undergo spontaneous regression.
Ganglioneuroma represents the mature, benign form of neural crest neoplasm. This is far less frequent compared with neuroblastoma; it may develop from the maturation of a known malignant neuroblastoma, or it may be found de novo.
Ganglioneuromas most frequently occur in the posterior mediastinum followed by the extra-adrenal retroperitoneum ( e-Fig. 122.10 ) and the adrenal gland. These tumors usually occur in older children, are frequently asymptomatic, and are often found incidentally on imaging. Occasionally, symptoms may result from tumor growth into the intervertebral foramina, causing spinal cord compression. Urinary catecholamine levels are usually normal.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here