Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Cholelithiasis, previously thought rare in children without hemolytic anemia, is diagnosed with increasing frequency since the increased ultrasound use. Gallstones have been reported in the fetus, although most resolve spontaneously.
Development of gallstones in infants may be related to immature physiologic regulation of bile salt secretion. Chronic cholestasis likely plays a role in the pathophysiology of cholelithiasis. Although infantile gallstones are often discovered incidentally, many predisposing conditions have been described ( Box 88.1 ). Infantile gallstones resolve spontaneously less often than in the fetus and are rarely complicated by biliary tract perforation and peritonitis.
Obstructive congenital biliary tree anomalies
Total parenteral nutrition
Diuretics (furosemide)
Gastrointestinal dysfunction (short-gut syndrome or terminal ileal disease)
Prolonged fasting
Phototherapy
Dehydration
Infection
Hemolytic anemia
Umbilical venous catheterization
Antibiotics
Although most gallstones seen in older children are idiopathic, a number of underlying states are associated ( Box 88.2 ). Prominent among these are sickle cell disease and intestinal problems that interfere with normal enterohepatic circulation. Patients with sickle cell disease have an increased incidence of gallstones with advancing age. Gallstones have also been reported after surgery and antibiotic therapy.
Sickle cell disease
Cystic fibrosis or other pancreatic disease
Malabsorption
Total parenteral nutrition
Inflammatory bowel disease (Crohn disease)
Short-gut syndrome (intestinal resection)
Hemolytic anemia
Choledochal cyst
Antibiotics
Cholelithiasis is usually asymptomatic in most infants and young children with an increased incidence of symptoms in older children. When symptoms occur in older children and adolescents, they are similar to those seen in adults and include bloating, nausea, vomiting, and postprandial right upper quadrant colicky pain radiating to the shoulder. Younger children may present with nonspecific symptoms such as irritability and may be unable to verbalize or relate their discomfort to the right upper quadrant or to a recent meal.
Choledocholithiasis results from migration of stones from the gallbladder into the common duct. Stones are more likely to be symptomatic when they pass into the cystic duct or the common bile duct. The most common complication of gallstones in children is pancreatitis, although the most common cause of pancreatitis is idiopathic or posttraumatic.
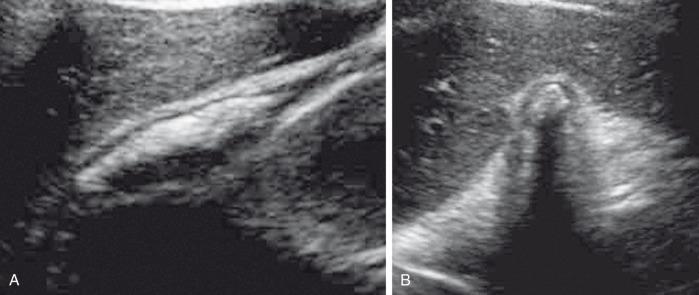
While radiolucent cholesterol stones are the most common type overall, they are rare in children and many pediatric gallstones are visible radiographically. Even so, sonography remains the primary imaging modality for the evaluation of cholelithiasis. Gallstones are seen as echogenic focus with posterior acoustic shadowing ( Fig. 88.1 ), and most demonstrate twinkling artifact on color Doppler images. Most stones move with change in patient position, which should be a routine maneuver during hepatobiliary sonography ( Fig. 88.2 ). Four general sonographic patterns of cholelithiasis are described here.

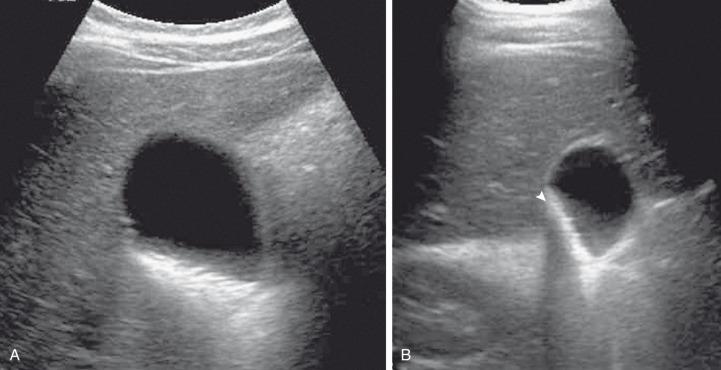
The first is the simple echogenic, shadowing, mobile stone, which may be single or multiple. The second describes collections of very tiny, sandlike stones, termed milk of calcium , which may mimic gallbladder sludge. Acoustic shadowing may be seen only in the aggregate (see Fig. 88.2 ). Third, if bile within the gallbladder is of high density, stones may seem to float on the surface, giving an apparent fluid-fluid level. The fourth pattern of cholelithiasis relates to stones within a contracted gallbladder when the stones produce an echogenic double arc known as the wall echo shadow (WES) complex. This pattern may also be seen in patients who have not fasted sufficiently ( Fig. 88.3 ). Careful scrutiny must be employed so as not to confuse the WES complex with emphysematous cholecystitis, which is far more common in adults than in children.
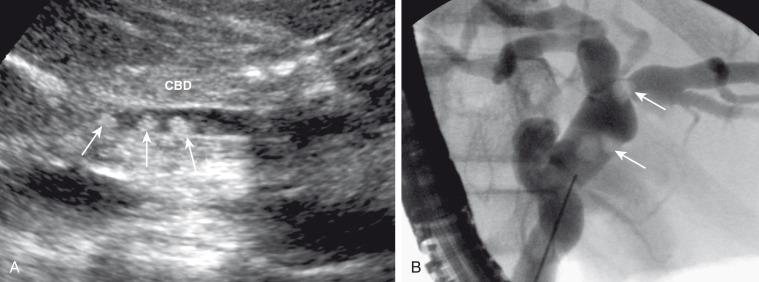
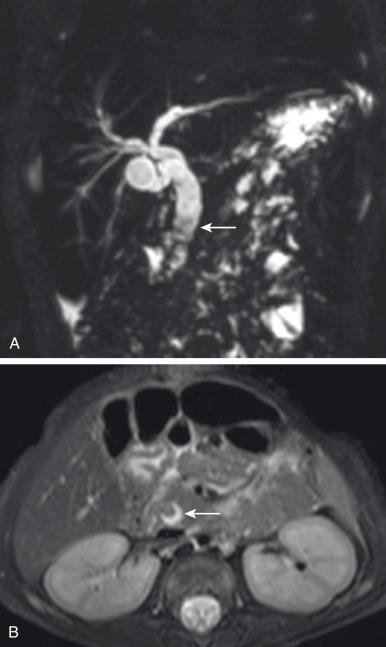
Sonography is less successful detecting choledocholithiasis than cholelithiasis due to interference from adjacent bowel gas. Dilated bile ducts ( Fig. 88.4 ) may be the only sonographic sign of a more distal obstructing stone. If no stone is seen on sonography, yet there is evidence of biliary ductal dilation, magnetic resonance cholangiopancreatography (MRCP) is the next modality of choice. With MRCP, most stones are seen as hypointense filling defects within the gallbladder and the biliary tree ( Fig. 88.5 ). Some stones, such as pigment stones, are hyperintense on T1-weighted 3D gradient echo sequences.
Treatment of infantile gallstones is generally conservative and includes addressing the underlying cause of disease. Surgery, particularly laparoscopic surgery, is the usual treatment of choice for symptomatic patients and patients with choledocholithiasis. Obstructive stones in the distal common bile duct (CBD) may be treated via endoscopic retrograde cholangiopancreatography (ERCP).
Biliary sludge, particulate matter within the bile produced by cholestasis, is of debated clinical significance. Although the majority of biliary sludge is a transient finding, particularly if associated with a transient predisposing condition, it may evolve into gallstones. Occasionally, the sludge itself may cause obstructive jaundice, which is termed as inspissated bile syndrome.
Sludge is formed predominantly of calcium bilirubinate particles and, depending on the underlying process, cholesterol crystals. Predisposing conditions that share the common pathway of biliary stasis include biliary outflow obstruction, intravenous hyperalimentation, hemolysis, treatment with ceftriaxone, and prolonged fasting.
Biliary sludge is usually asymptomatic; however, it may cause symptoms if associated with microlithiasis or if “bile balls” course into the biliary ducts. When this happens, symptoms are similar to those produced by cholelithiasis.
On sonography, sludge is echogenic without acoustic shadowing; it typically layers in the dependent portion of the gallbladder or other part of the biliary tree, such as a choledochal cyst, and demonstrates a fluid-sludge level ( e-Fig. 88.6 ). Inspissated bile may be slightly more echogenic than regular sludge, but it does not cause any posterior acoustic shadowing. Occasionally, sludge coalesces within the gallbladder lumen, forming a tumefactive “sludge ball” that, when fixed, may mimic a polyp or mass. Differential considerations include uncommon conditions such as hemobilia, biliary mucus, and parasitic infection.

Because biliary sludge is generally asymptomatic and resolves spontaneously with resolution of the underlying condition, it does not require separate treatment. However, follow-up in patients in whom the underlying condition does not remit is important, particularly if the patient becomes symptomatic. Inspissated bile syndrome may resolve with removal of predisposing factors but has also been treated with mucolytic agents and laparoscopic surgery.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here