Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The concentrations of hydrogen and bicarbonate ions in plasma must be precisely regulated to optimize enzyme activity, oxygen transport, and rates of chemical reactions within cells. Each day approximately 15,000 mmol of carbon dioxide (which can generate carbonic acid as it combines with water) and 50 to 100 mEq of nonvolatile acid (mostly sulfuric acid) are produced and must be eliminated safely. The body is able to maintain this intricate acid–base balance by utilizing buffers, pulmonary excretion of carbon dioxide, and renal elimination of acid. This chapter will define concepts important for understanding acids and bases, discuss clinical measurements of blood gases and their interpretation, and present a diagnostic approach to common acid–base disturbances.
Bronsted and Lowry defined an acid as a molecule that can act as a proton (H + ) donor and a base as a molecule that can act as a proton acceptor. In physiologic solutions a strong acid is a substance that readily and irreversibly gives up an H + , and a strong base avidly binds H + . In contrast, biologic molecules are either weak acids or bases, which reversibly donate H + or reversibly bind H + .
A blood pH less than 7.35 is called acidemia, and a pH greater than 7.45 is called alkalemia, regardless of the mechanism. The underlying process that lowers the pH is called an acidosis, and the process that raises the pH is known as an alkalosis . A patient can have a mixed disorder with both an acidosis and an alkalosis concurrently but can only be either acidemic or alkalemic. The last two terms are mutually exclusive.
Base excess (BE) is usually defined as the amount of strong acid (hydrochloric acid for BE greater than zero) or strong base (sodium hydroxide for BE less than zero) required to return 1 L of whole blood exposed in vitro to a P co 2 of 40 mm Hg to a pH of 7.4. Instead of an actual titration, the blood gas machine calculates the BE with algorithms utilizing plasma pH, blood P co 2 , and hemoglobin concentration. The number is supposed to refer to the nonrespiratory or metabolic component of an acid–base disturbance. A BE less than zero (also called a base deficit ) suggests the presence of a metabolic acidosis, and a value greater than zero suggests the presence of a metabolic alkalosis. In vitro, the number has been accurate but in the living organism, because ions do cross beyond vascular and cellular boundaries, a primary acute change in Pa co 2 sometimes can cause the BE to move in the opposite direction, despite an unchanged metabolic acid–base status. In clinical practice the BE is often used as a surrogate measure for lactic acidosis, which is one measurement to help determine adequacy of intravascular volume resuscitation.
At 37°C, the normal hydrogen ion concentration in arterial blood and extracellular fluid is 35 to 45 nmol/L, which is equivalent to an arterial pH of 7.45 to 7.35, respectively. The normal plasma bicarbonate ion concentration is 24 ± 2 mEq/L. Physiologic changes to acid–base disturbances are corrected by three systems: buffers, ventilation, and renal response. The buffer systems provide an immediate chemical response, and the ventilatory response occurs in minutes whenever possible. The renal response can take days but can provide nearly complete restoration of the pH.
A buffer is defined as a substance within a solution that can prevent extreme changes in pH. A buffer system is composed of a base molecule and its weak conjugate acid. The base molecules of the buffer system bind excess hydrogen ions, and the weak acid protonates excess base molecules. The dissociation ionization constant (pK a ) indicates the strength of an acid and is derived from the classic Henderson-Hasselbalch equation ( Fig. 22.1 ). The pK a is the pH at which an acid is 50% protonated and 50% deprotonated. Hydrochloric acid, a strong acid, has a pK a of −7, whereas carbonic acid, a weak acid, has a pKa of 6. The most important buffer systems in blood, in order of importance, are the (1) bicarbonate buffer system (H 2 CO 3 /HCO 3 − ), (2) hemoglobin buffer system (HbH/Hb − ), (3) other protein buffer systems (PrH/Pr − ), (4) phosphate buffer system (H 2 PO 4 − /HPO 4 2 − ), and (5) ammonia buffer system (NH 3 /NH 4 + ).
![Fig. 22.1, Henderson-Hasselbalch equation. [Base], Concentration of base; [Conjugate acid], concentration of conjugate acid. Fig. 22.1, Henderson-Hasselbalch equation. [Base], Concentration of base; [Conjugate acid], concentration of conjugate acid.](https://storage.googleapis.com/dl.dentistrykey.com/clinical/AcidBaseBalanceandBloodGasAnalysis/0_3s20B978032379677400022X.jpg)
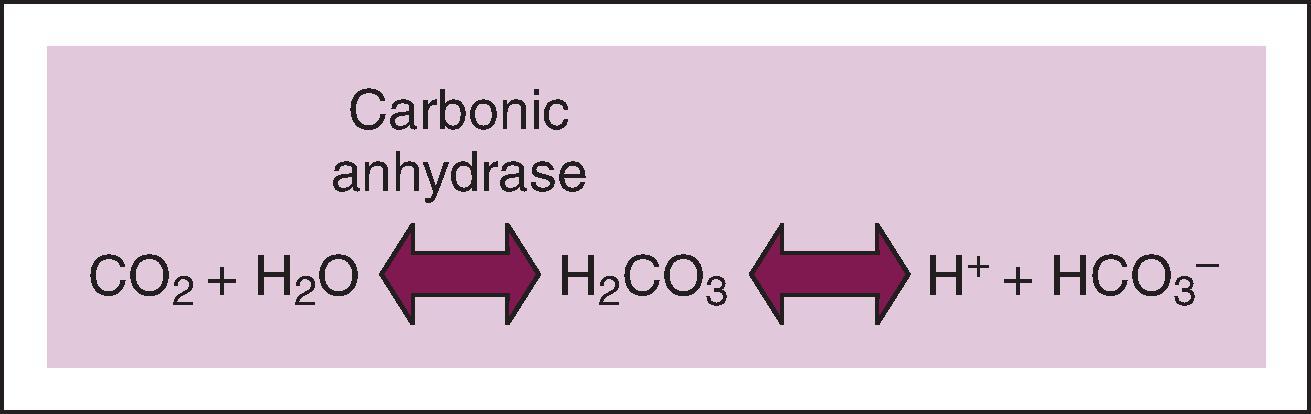
Carbon dioxide, generated through aerobic metabolism, slowly combines with water to form carbonic acid, which spontaneously and rapidly deprotonates to form bicarbonate ( Fig. 22.2 ). In this system the base molecule is bicarbonate and its weak conjugate acid is carbonic acid. Less than 1% of the dissolved carbon dioxide undergoes this reaction because it is so slow. However, the enzyme carbonic anhydrase, present in the endothelium, erythrocytes, and kidneys, catalyzes this reaction to accelerate the formation of carbonic acid and make this the most important buffering system in the human body when combined with renal control of bicarbonate and pulmonary control of carbon dioxide.
The hemoglobin protein serves as an effective buffering system because it contains multiple histidine residues. Histidine is an effective buffer from pH 5.7 to 7.7 (pK a 6.8) because of multiple protonatable sites on the imidazole side chains. Buffering by hemoglobin depends on the bicarbonate system to facilitate the movement of carbon dioxide intracellularly. ( Fig. 22.3 ). At the lungs, the reverse process occurs. Chloride ions move out of the red blood cells as bicarbonate enters for conversion back to carbon dioxide. The carbon dioxide is released back into plasma and is eliminated by the lungs. This process allows a large fraction of extrapulmonary carbon dioxide to be transported back to the lungs as plasma bicarbonate.
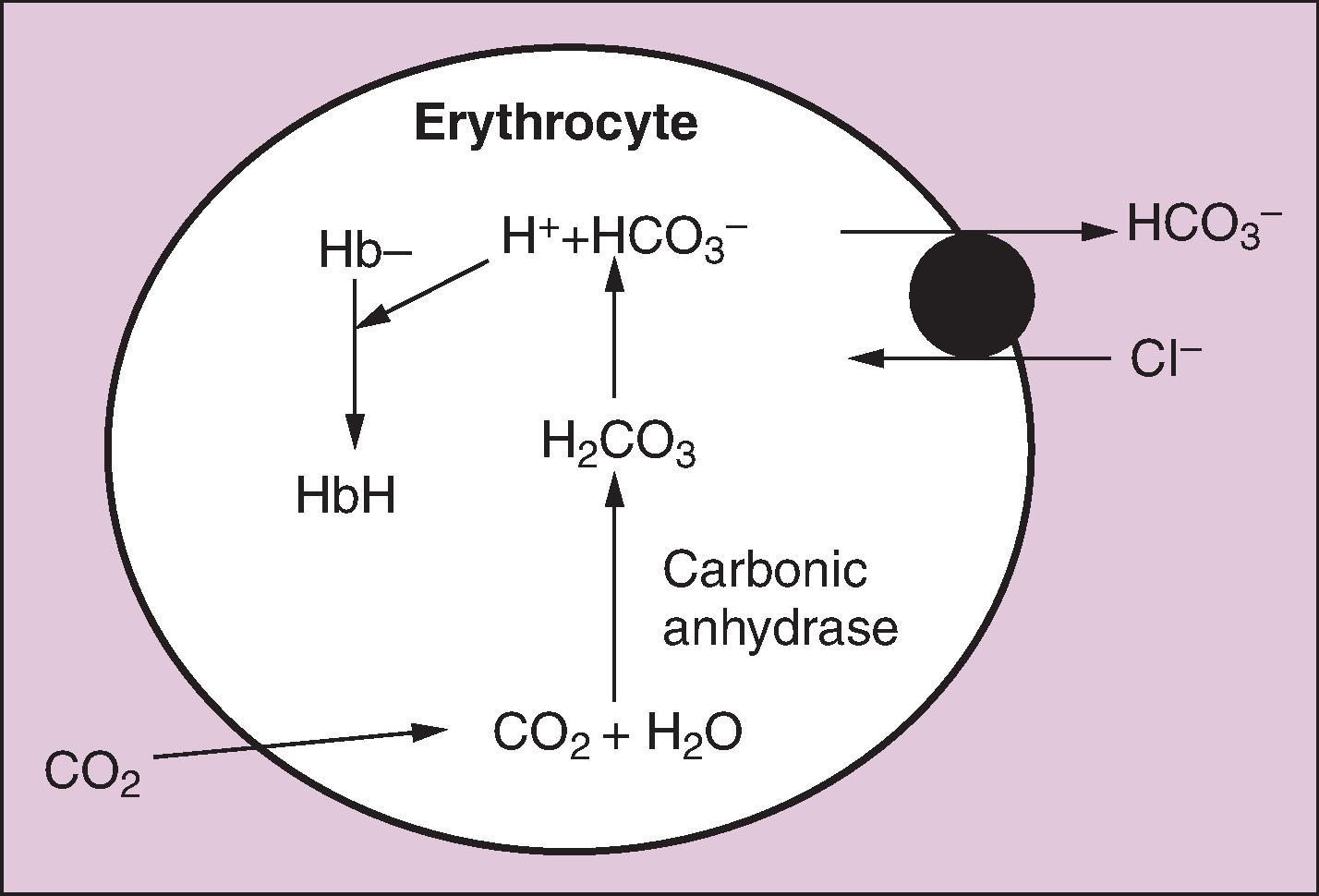
Oxygenated and deoxygenated hemoglobin have different affinities for hydrogen ions and carbon dioxide. Deoxyhemoglobin takes up more hydrogen ions, which shifts the carbon dioxide/bicarbonate equilibrium to produce more bicarbonate and facilitates removal of carbon dioxide from peripheral tissues for release into the lungs. Oxyhemoglobin favors the release of hydrogen ions and shifts the equilibrium to more carbon dioxide formation. At physiologic pH, a small amount of carbon dioxide is also carried as carbaminohemoglobin. Deoxyhemoglobin has a greater affinity (3.5 times) for carbon dioxide, so venous blood carries more carbon dioxide than arterial blood (Haldane effect). These two mechanisms combine to account for the difference in carbon dioxide content of arterial versus venous plasma (25.6 mmol/L vs. 27.7 mmol/L, respectively).
Central chemoreceptors lie on the anterolateral surface of the medulla and respond to changes in cerebrospinal fluid (CSF) pH. Carbon dioxide diffuses across the blood–brain barrier to elevate CSF hydrogen ion concentration, which activates the chemoreceptors and increases alveolar ventilation. The relationship between Pa co 2 and minute ventilation is almost linear except at very high arterial Pa co 2 , when carbon dioxide narcosis develops, and at very low arterial Pa co 2 , when the apneic threshold is reached. There is a very wide variation in individual Pa co 2 /ventilation response curves, but minute ventilation generally increases 1 to 4 L/min for every 1 mm Hg increase in Pa co 2 . During general anesthesia, spontaneous ventilation will cease when the Pa co 2 decreases to less than the apneic threshold, whereas in the awake patient, cortical influences prevent apnea, so the apneic threshold is not ordinarily observed.
Peripheral chemoreceptors are located at the bifurcation of the common carotid arteries and surrounding the aortic arch. The carotid bodies are the principal peripheral chemoreceptors and are sensitive to changes in Pa o 2 , Pa co 2 , pH, and arterial perfusion pressure. They communicate with the central respiratory centers via the glossopharyngeal nerves. Unlike the central chemoreceptors, which are more sensitive to hydrogen ions, the carotid bodies are most sensitive to Pa o 2 . Bilateral carotid endarterectomies abolish the peripheral chemoreceptor response, and these patients have almost no hypoxic ventilatory drive.
The stimulus from central and peripheral chemoreceptors to either increase or decrease alveolar ventilation diminishes as the pH approaches 7.4 such that complete correction or overcorrection is not possible. The pulmonary response to metabolic alkalosis is usually less than the response to metabolic acidosis. The reason is because progressive hypoventilation results in hypoxemia when breathing room air. Hypoxemia activates oxygen-sensitive chemoreceptors and limits the compensatory decrease in minute ventilation. Because of this, Pa co 2 usually does not rise above 55 mm Hg in response to metabolic alkalosis for patients not receiving oxygen supplementation.
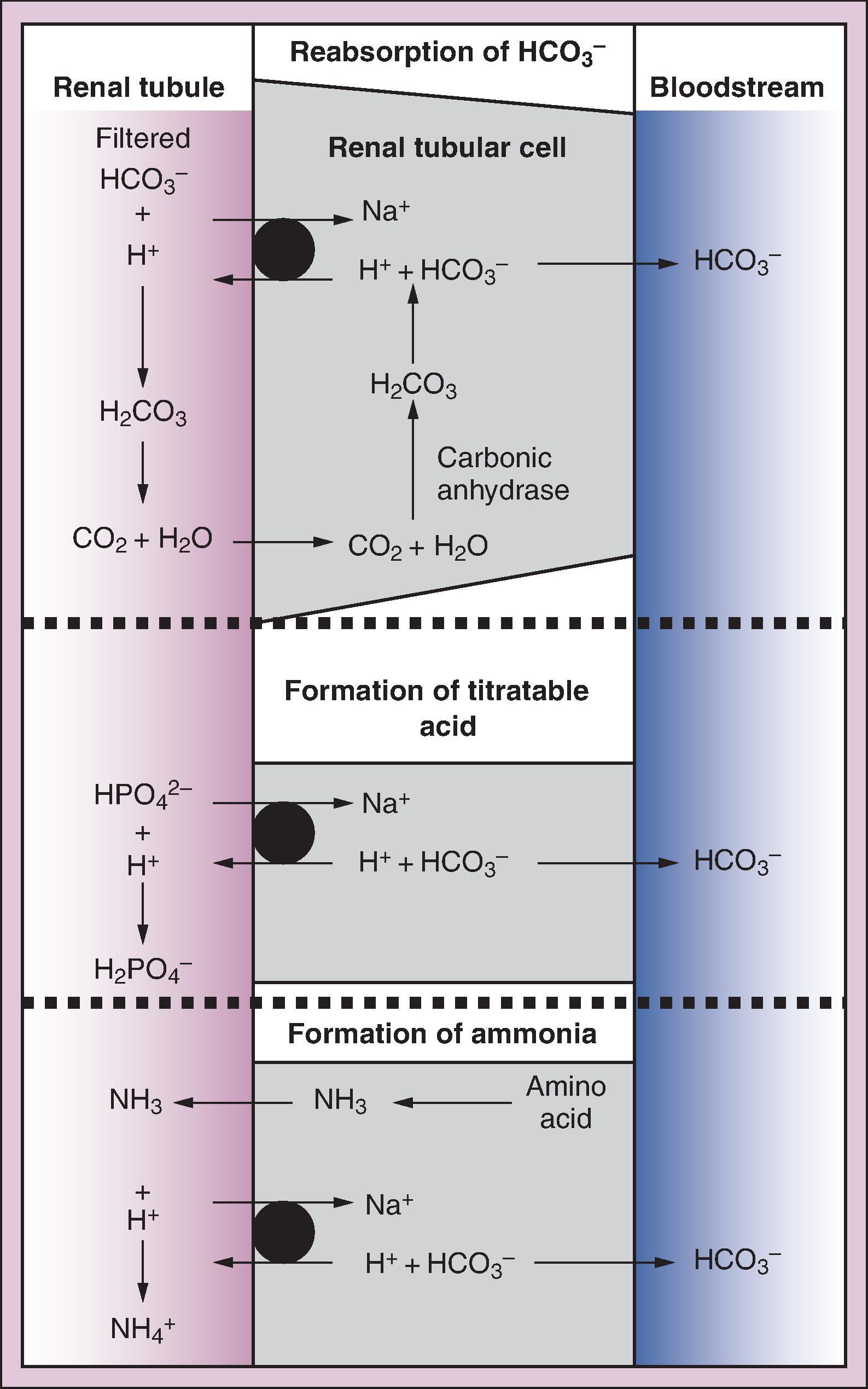
Renal effects are slower in onset and may not be maximal for up to 5 days. The response occurs via three mechanisms: (1) reabsorption of the filtered HCO 3 − , (2) excretion of titratable acids, and (3) ammonia ( Fig. 22.4 ). Carbon dioxide combines with water in the renal tubular cell. With the help of carbonic anhydrase, the bicarbonate produced enters the bloodstream while the hydrogen ion is exchanged with sodium and is released into the renal tubule. There, H + combines with filtered bicarbonate and dissociates into carbon dioxide and water with help from carbonic anhydrase located in the luminal brush border, and the carbon dioxide diffuses back into the renal tubular cell. The proximal tubule reabsorbs 80% to 90% of the bicarbonate this way, and the distal tubule takes care of the remaining 10% to 20%. Once the bicarbonate is reclaimed, further hydrogen ions can combine with HPO 4 2 − to form H 2 PO 4 − , which is eliminated in the urine. The last important urinary buffer is ammonia. Ammonia is formed from deamination of glutamine, an amino acid. The ammonia passively crosses the cell membrane to enter the tubular fluid. In the tubular fluid it combines with hydrogen ion to form NH 4 + , which is trapped within the tubule and excreted in the urine. All of these steps allow for the generation and return of bicarbonate into the bloodstream. The large amount of bicarbonate filtered by the kidneys allows for rapid excretion, if necessary, for compensation during alkalosis. The kidneys are highly effective in protecting the body against alkalosis except in association with sodium deficiency or mineralocorticoid excess.
The ability to measure arterial blood gas (ABG) and venous blood gas has revolutionized patient care during anesthesia and in the intensive care unit (ICU). Although pulse oximetry and capnography can be monitored continuously, analysis of ABGs has increased our diagnostic ability and the accuracy of our measurements.
Arterial blood is most often obtained percutaneously from the radial, brachial, or femoral artery. In certain clinically stable situations venous pH, bicarbonate, and BE have sufficient agreement to be clinically interchangeable for arterial values and save an arterial puncture. Venous pH is usually only 0.03 to 0.04 less than arterial values. Venous blood cannot be used for estimation of oxygenation for two reasons: venous Po 2 (Pvo 2 ) is significantly less than Pao 2 and depending on the site of the venous blood draw, differences in tissue metabolic activity may alter Pvo 2 . Agreement between arterial and venous P co 2 is too unpredictable to be clinically useful as a single test, but trends in P co 2 may be helpful. Periodic correlations of arterial and venous measurements should be performed, especially when venous measurements are used for serial monitoring in critically ill patients.
A heparinized, bubble-free, fresh blood sample is required for blood gas analysis. Air bubbles should be removed because equilibration of oxygen and carbon dioxide in the blood with the corresponding partial pressures in the air bubble could influence the measured results. A delay in analysis can lead to oxygen consumption and carbon dioxide generation by the metabolically active white blood cells. Usually this error is small and can be reduced by placing the sample on ice. In some leukemia patients with a markedly increased white blood cell count this error can be large and lead to a falsely low P o 2 even though the patient's oxygenation is acceptable. This phenomenon is often referred to as leukocyte larceny .
Decreases in temperature decrease the partial pressure of a gas in solution, even though the total gas content does not change. Both P co 2 and P o 2 decrease during hypothermia, but serum bicarbonate is unchanged. This leads to an increase in pH if the blood could be measured at the patient's temperature. A blood gas with a pH of 7.4 and P co 2 of 43 mm Hg at 37°C will have a pH of 7.5 and a P co 2 of 31 mm Hg at 30°C. Unfortunately, all blood gas samples are measured at 37°C, which raises the issue of how to best manage the ABG measurement in hypothermic patients. This has led to two management strategies: alpha-stat and pH-stat.
Alpha-stat theory advocates measuring all blood gases at 37°C. Alpha refers to the protonation state of the imidazole side chain of histidine. The pKa of histidine changes with temperature so that its protonation state is relatively constant regardless of temperature. The term alpha-stat developed because as the patient's pH was allowed to drift with temperature, the protonation state of the histidine residues remained static. During cardiopulmonary bypass, an anesthesia provider using alpha-stat would manage the patient based on an ABG measured at 37°C and strive to keep that pH at 7.4, but the patient's true pH would be higher. No extra adjustments would be made for the patient's hypothermia.
pH-stat is different from alpha-stat in that it requires keeping a patient's pH static at 7.4 based on the core temperature. During cardiopulmonary bypass, an anesthesia provider using pH-stat would manage the patient based on an ABG that is corrected for the patient's temperature. With hypothermia, this usually means adding carbon dioxide so that the patient's temperature-correct (hypothermic) blood gas has a pH of 7.4. In the ICU during targeted temperature management pH-stat management would mean lowering the patient's minute ventilation. The lower pH and higher P co 2 maintained during pH-stat may improve cerebrovascular perfusion during hypothermia; however, there is still debate about which method provides better outcomes.
Decreases in temperature decrease the partial pressure of oxygen in solution. Because hypothermia causes the oxygen–hemoglobin dissociation curve to shift to the left, there is a higher affinity of hemoglobin to oxygen, making it easier for oxygen to attach to hemoglobin, but more difficult for it to diffuse to the tissues.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here