Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Access-site complications continue to be the most common adverse events after cardiovascular interventions, extending the patient’s hospital stay and increasing the associated procedural costs.
Selection of the appropriate access site is frequently a key issue for the successful completion of coronary, peripheral vascular, or structural procedures. Selection depends on the target vessel or structural intervention, the operator’s skills, and the patient’s preferences.
The ultrasound-guided common femoral artery puncture is safe and effective to reduce associated complications.
Several femoral access closure technologies are on the interventional field that offer equivalent or even better patient outcomes and satisfaction compared with manual and mechanical compression.
The most commonly used femoral closure devices provide two types of mechanisms for percutaneously controlling bleeding: deploying sutures or staples to close the femoral puncture site or using resorbable plugs to temporarily seal the arteriotomy.
When using closure devices, the operator should be careful in choosing the site of cannulation of the femoral artery.
Vascular closure devices have improved patient comfort by enabling early ambulation, and their use has decreased the burden on the medical staff with a potential reduction in groin complication rates.
In recent years, interventional cardiology has succeeded in further expanding its field of action for the treatment of cardiovascular diseases in a variety of vascular and nonvascular territories. In this context, the appropriate selection of vascular access, as well as its proper management, are fundamental for patient’s safety.
Percutaneous coronary interventions (PCI) have usually been performed by the femoral approach; however, to reduce complications and increase patient comfort, radial access is increasingly used and is becoming the preferred access site by many interventionalists. Moreover, the use of radial approach has demonstrated a reduction not only in major bleeding events but also in hospital stay when compared to femoral access using manual compression for hemostasis. Despite this, femoral access is still the preferred access in multiple settings, as in the case of complex PCI (e.g., chronic total occlusions or left main trunk interventions).
Furthermore, femoral access is especially necessary in interventions that require large-bore access. In this sense, the transfemoral approach is the commonly used access for transcatheter aortic valve replacement and for mechanical circulatory support (intraaortic balloon pump, Impella [Abiomed, Danvers, MA], or venoarterial extracorporeal membrane oxygenation).
In general, the most common noncardiac catheterization adverse event is related to the vascular access site. Vascular complications are also associated with an increased risk of nonfatal myocardial infarction or death in the year following the procedure, in particular when accompanied by significant bleeding. Additionally, major access-site complications increase medical costs and the length of hospital stay, and delay social reinsertion. Moreover, there is an increasing proportion of patients undergoing therapeutic interventions and being discharged the same day. Therefore, enhancing the safety of arterial access and hemostasis has become a priority in the catheterization laboratory.
The aggressive level of anticoagulation used during therapeutic procedures requires the achievement of safe and reliable hemostasis of the access site. The use of manual or mechanical compression was until recently the only way to control bleeding by allowing clot formation at the arteriotomy site. The appearance and clinical use of vascular closure devices (VCDs) for rapid hemostasis after femoral access started more than 25 years ago. Since then, these devices have improved patient comfort by enabling early ambulation, and their use has decreased the burden on the medical staff.
The use of passive femoral devices (pads impregnated with procoagulant material, and mechanical compression devices that replace manual compression) has not resulted in a reduction in groin complication rates. With the development of more refined devices, such as active femoral closure devices (including sutured-based, collagen-based, or patches), observational data has demonstrated a reduction of bleeding and vascular complication rates compared to manual compression. However, these effects were not always evident in randomized studies. The introduction of newer femoral closure devices, a better patient selection, as well as the development of a learning curve has probably improved the safety of this intervention.
This chapter summarizes the concepts of femoral access puncture, the use of arterial closure devices, and postprocedural management.
The selection of an appropriate access site is frequently a key issue for the successful completion of coronary, peripheral vascular, or structural procedures. Proficiency with all available vascular puncture techniques is a basic requirement for the interventionalist. The selection of a vascular access site is related to the interventional target, sheath diameter, access to target lesion length, atheromatosis burden of the route, and patient clinical characteristics.
It is important to review clinical reports and perform a high-quality preprocedural vascular assessment of all peripheral pulses, presence of bruits, blood pressure difference between arms, and other pertinent findings, such as skin color, trophic changes, ulcerations, or the presence of intermittent claudication. This important decision deserves full analysis of the target vessel for treatment, consideration of the patient’s preference, and assessment of the interventionalist’s skills. Some aspects of the vascular access are crucial to the safety and success of the procedure.
The retrograde femoral access and radial access are the two preferred approaches for coronary interventions. Ulnar and brachial accesses are seldom utilized. There are several techniques for endovascular peripheral therapies according to the target treatment vessel: crossover femoral approach for contralateral iliofemoral treatment; antegrade femoral puncture for ipsilateral treatment of below-the-knee arteries; femoral retrograde access for aortic, carotid, iliac, and renal vessels; local puncture for dialysis access treatment; and direct retrograde access from below-the-knee arteries. Moreover, the common femoral artery (CFA) is the preferred access for percutaneous aortic artery and aortic valve interventions.
The CFA is the preferred site for percutaneous arterial cannulation because it is large, accessible, and easily compressible. However, strict adherence to meticulous technique is necessary to avoid vascular complications, in particular when larger sheaths are being used.
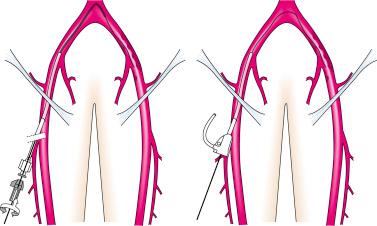
The reduction in the sheath size was presumed to result in fewer access complications, but there was not a clear association with a decrement in the bleeding rate. Retrograde femoral access can be considered the standard technique for coronary, renal, iliac, and crossover for contralateral femoral interventions ( Fig. 31.1 ). Endovascular repair of abdominal and thoracic aortic aneurysms has become the standard of care for anatomically appropriate patients. All the devices developed to date are deployed through relatively large (12- to 24-Fr) sheaths.
Transcatheter aortic valve implantation is the treatment of choice for patients with aortic valve stenosis and moderate to high surgical risk and its indication is rapidly expanding toward lower-risk patients. The fully transfemoral percutaneous approach with VCDs is considered the standard of care, as well as a fundamental component of the minimalistic approach. The use of larger sheaths for these interventions requires a meticulous puncture technique in the anterior wall of the CFA.
Any vascular puncture should be performed under sterile technique. The groin is shaved in the area that spans approximately 10 cm around the specified puncture site, preferably using electric clippers with a single-use sterile razor. A variety of antimicrobial agents are available, but povidone-iodine solutions and chlorhexidine-based preparations are most commonly used. There is evidence that chlorhexidine-based solutions are more effective and cause less irritation than povidone-iodine ones.
Since the vascular access is generally the only painful part of the procedure, generous local anesthesia with approximately 20 mL of 1% to 2% lidocaine is needed, as well as adequate pressure and rhythm monitoring to identify any possible vagal reaction. First, create an intradermal wheal with 3 to 4 mL of lidocaine at the desired level of entry. The remaining lidocaine will be used to infiltrate the deeper planes covering the anticipated path of the needle to the artery.
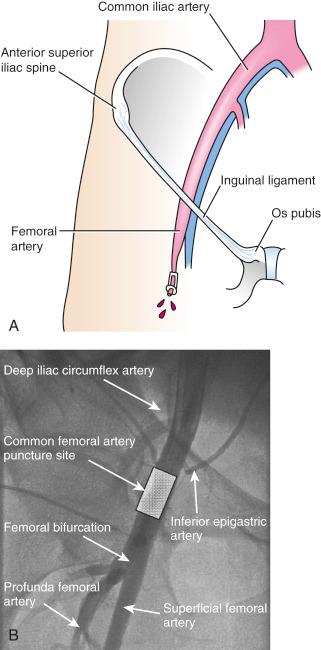
The CFA originates as a continuation of the external iliac artery immediately after the take-off of the inferior epigastric artery and after crossing the inguinal ligament, which represents an important anatomical landmark. When drawing an imaginary line between the anterior superior iliac supine and the pubis tubercle, it is near or at the midpoint of the line. Then, the CFA descends almost vertically down and ends at the hiatus of the adductor muscle, where it branches into the superficial femoral artery and the profunda femoral artery ( Fig. 31.2 ).
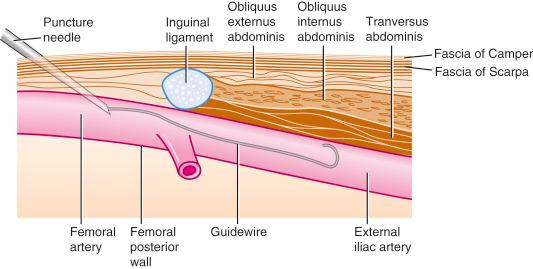
One important aspect is to puncture only the anterior wall of the femoral artery with open-bore needles, which have the advantage of demonstrating blood return immediately ( Fig. 31.3 ).
Based on angiographic evaluation, the mean luminal diameter of the CFA is 6.9 ± 1.4 mm and its mean length is 43.3 ± 16.2 mm. This is theoretically large enough to comfortably accommodate the typical range of femoral sheath sizes for most diagnostic and interventional procedures. Note that diabetics, women, and patients with small body surface area have disproportionately smaller CFA.
In order to avoid complications, the operator should be careful in choosing the site of cannulation at the level of the CFA (see Fig. 31.2 ). Puncture sites not located at the appropriate level are responsible for the majority of vascular access complications. Cannulation of the artery too low increases the chance of entering the superficial femoral artery rather than the CFA. This entry site may predispose to dissection, arterial occlusion, pseudoaneurysm, bleeding, and arteriovenous fistula formation. Entering the artery above the inguinal ligament may lead to problems in compressing the artery against the inguinal ligament, increasing the risk of hematoma formation and favoring retroperitoneal hemorrhage. It was reported that puncture performed above the inferior epigastric artery was associated with retroperitoneal bleeds.
The safest zone to puncture is located from 1 to 2 cm below the inguinal ligament (1 to 2 cm below the line traced from the anterosuperior iliac spine to the pubic tubercle) and above the femoral bifurcation (see Fig. 31.2 ). There are different ways to ascertain this location: palpatory method, fluoroscopic evaluation, and ultrasound-guided puncture. In a multinational survey, 60% of operators used the classic palpation technique, while fluoroscopic evaluation and ultrasound-guided puncture are used by only 11% and 2% of operators, respectively (60%).
This method is based on the identification of landmarks to identify the inguinal ligament and hence the position of the CFA distal to it: inguinal crease, the point of maximal pulsation, and bony landmarks.
The puncture at or just below the inguinal crease has been extensively used as a landmark based on the belief that it was closely related to the inguinal ligament, but there is a lot of evidence against that concept. First, the distance between both is highly variable, ranging from 0 to 11 cm with an average of 6.5 ± 1.9 cm. In addition, a significant variation between the inguinal crease and the femoral bifurcation has been reported. The point of maximal pulsation is more reliable than the inguinal crease to localize the CFA since it has been reported that it is projected over the CFA in 92.7% of limbs. Finally, bony landmarks are based on the midpoint of a line between the anterior superior iliac spine and the pubic symphisis, in particular a point located 2.5 cm distally to this line. It is important to note that the surface landmarks could be altered in many conditions, such as obesity, prior hematoma, scarring, and low blood pressure, making this traditional method very unreliable.
The CFA correlates well to the area that is at the mid-third of the femoral head in the majority of cases. Accessing the CFA using fluoroscopy compared to traditional anatomic landmark guidance has improved the arterial puncture site. To note, femoral artery bifurcation is below the inferior border of the femoral head in 65% to 80% of cases, lies on the medial third of the femoral head in 92% of patients, and only 8% have the arterial completely medial to the femoral head.
Ultrasound guidance has emerged as an alternative method to identify the puncture site. In the last decade, it has become the standard of care outside the cardiac catheterization laboratory for vascular access, especially for central venous catheterization with guideline recommendations endorsing its use. Multiple randomized trials and meta-analysis have demonstrated a reduction in complications rates, number of attempts, and time to access. However, few operators use ultrasound routinely for vascular access in the cardiac catheterization laboratory.
Ultrasound allows for direct visualization of the CFA and the identification of the origin of the inferior epigastric artery superiorly and the femoral bifurcation inferiorly. Furthermore, applying some pressure with a transducer allows for the differentiation between the femoral artery and the femoral vein ( Fig. 31.4 ).
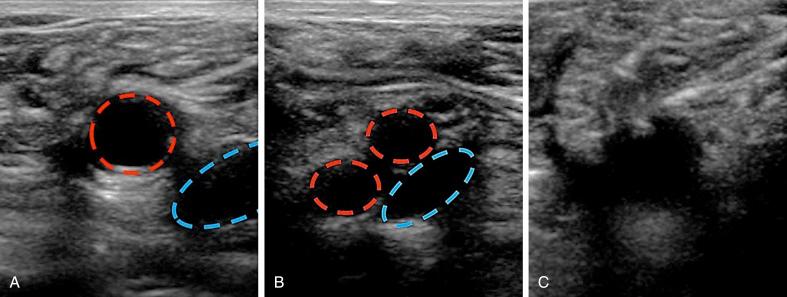
Several studies have examined the usefulness of ultrasound-guided femoral access. The largest study addressing this issue was FAUST (Femoral Arterial Access With Ultrasound Trial). It was a prospective, multicenter trial that randomized 1004 patients undergoing retrograde femoral approach to either fluoroscopic or ultrasound guidance. The primary end point was successful CFA cannulation. Secondary end points were time to sheath insertion, number of forward needle advancements, first pass success, accidental venipunctures, and vascular access complications at 30 days. Regarding the primary outcome, ultrasound guidance did not reach higher rates of CFA cannulation (86.4% vs. 83.3%, P .17). However, in patients with high femoral bifurcations, ultrasound-guided access was more likely to puncture at the level of the CFA (82.6% vs. 69.8%, P .01). With regard to secondary outcomes, ultrasound-guided puncture significantly improved first-pass success rate (83% vs. 46%, P .0001), and reduced the number of attempts (1.3 vs. 3.0, P .0001), venipuncture (2.4% vs. 15.8%, P .0001), and median time to access (136 s vs. 148 s, P .003). Moreover, vascular complications were less frequent in this group (1.4% vs. 3.4% P .04), a result driven by a significant reduction in groin hematomas >5 cm (0.6% vs. 2.2%, P .03).
A meta-analysis and systematic review with a total of 1551 subjects (782 in the ultra-sound–guided group and 769 in the palpation group) compared both femoral access techniques demonstrating that ultra-sound–guided femoral access was associated with 60% reduction in bleeding events, a 76% reduction in the number of puncture attempts, an 80% reduction in venipunctures, and similar rates of catheter insertion outside of the CFA boundaries ( Table 31.1 ).
| Outcomes | US-guided | Control | OR (95% CI) |
|---|---|---|---|
| Bleeding events | 11/782 | 26/769 | 0.41 (0.20–0.83) |
| ≥1 puncture attempt | 144/728 | 357/721 | 0.24 (0.19–0.31) |
| Venipunctures | 23/621 | 105/621 | 0.18 (0.11–0.29) |
| Puncture outside of the CFA | 76/558 | 87/549 | 0.84 (0.60–1.17) |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here