Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
On completion of this chapter, you should be able to:
• List the current limitations of ultrasound imaging that may be overcome by the use of ultrasound contrast agents
• Describe the properties that an ultrasound contrast agent must have to be clinically accepted
• Describe the difference between tissue-specific ultrasound contrast agents and vascular agents
• Describe how nonlinear contrast imaging modes improve the clinical capabilities of ultrasound contrast agents
• Describe the current clinical applications of contrast agents
Since the 1980s, a significant amount of research has been conducted toward the development of ultrasound contrast agents (UCAs) . Most of the work has centered on developing agents that can be administered intravenously to evaluate blood vessels, blood flow, tumors, and solid organs.
The clinical utilization of contrast-enhanced ultrasound imaging (CEUS) has been shown to reduce or eliminate some of the current limitations of ultrasound imaging and Doppler blood flow detection. These include limitations of spatial and contrast resolution on B-mode ultrasound and the detection of low-velocity blood flow and flow in smaller vessels using Doppler flow detection modes, including color flow imaging and pulsed wave Doppler with spectral analysis. Advances in ultrasound technology following the development of UCAs have resulted in contrast-specific imaging modes, which allow detection, display, and quantification of blood flow without the limitations of Doppler. The use of CEUS is growing around the world, and published clinical guidelines describe the most appropriate use of CEUS for a variety of abdominal, retroperitoneal, and other applications. Ultrasound contrast agents (UCA) are increasingly being used to improve the sensitivity and specificity of ultrasound diagnoses and are expanding sonography’s already broad range of clinical applications.
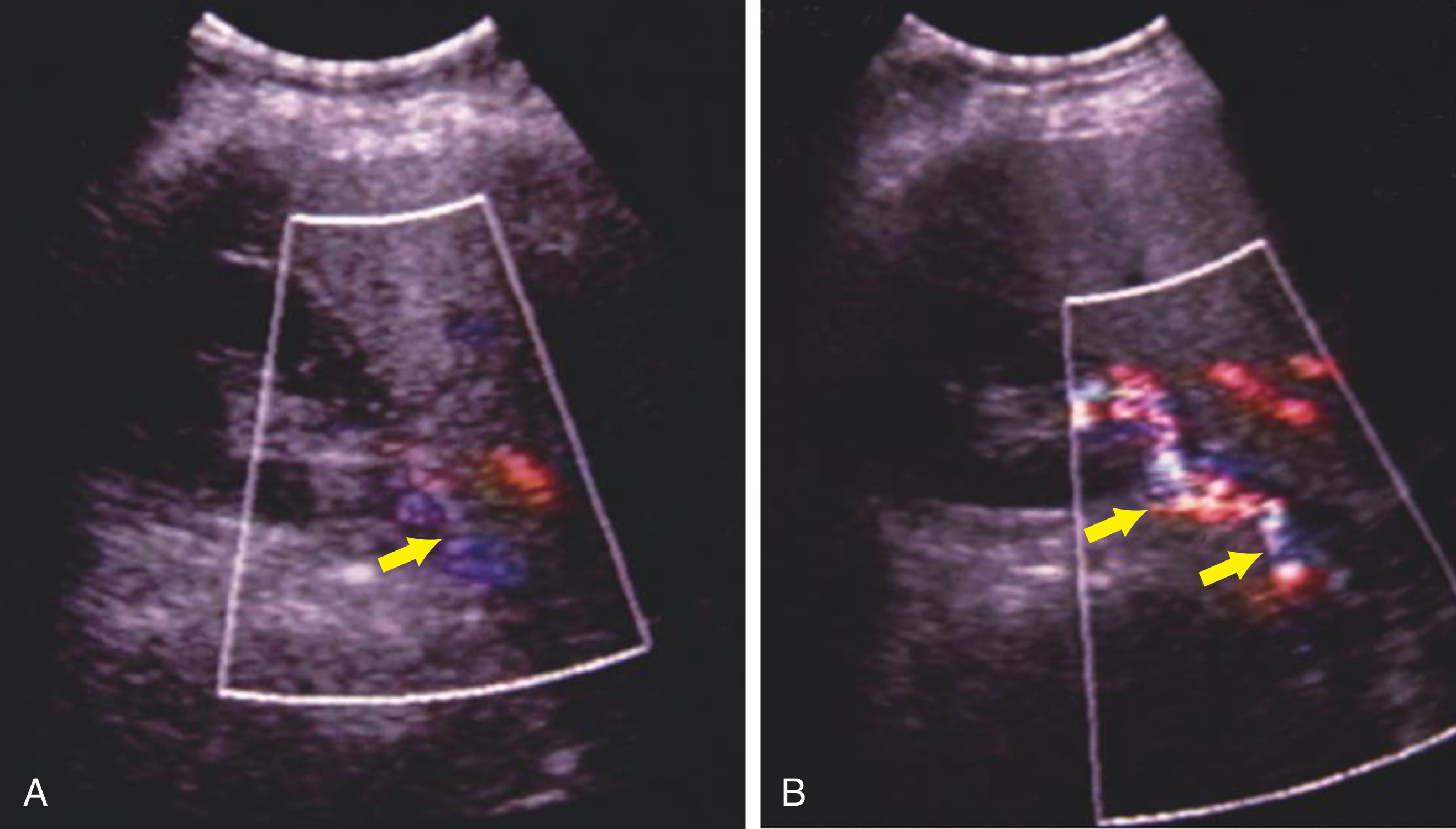
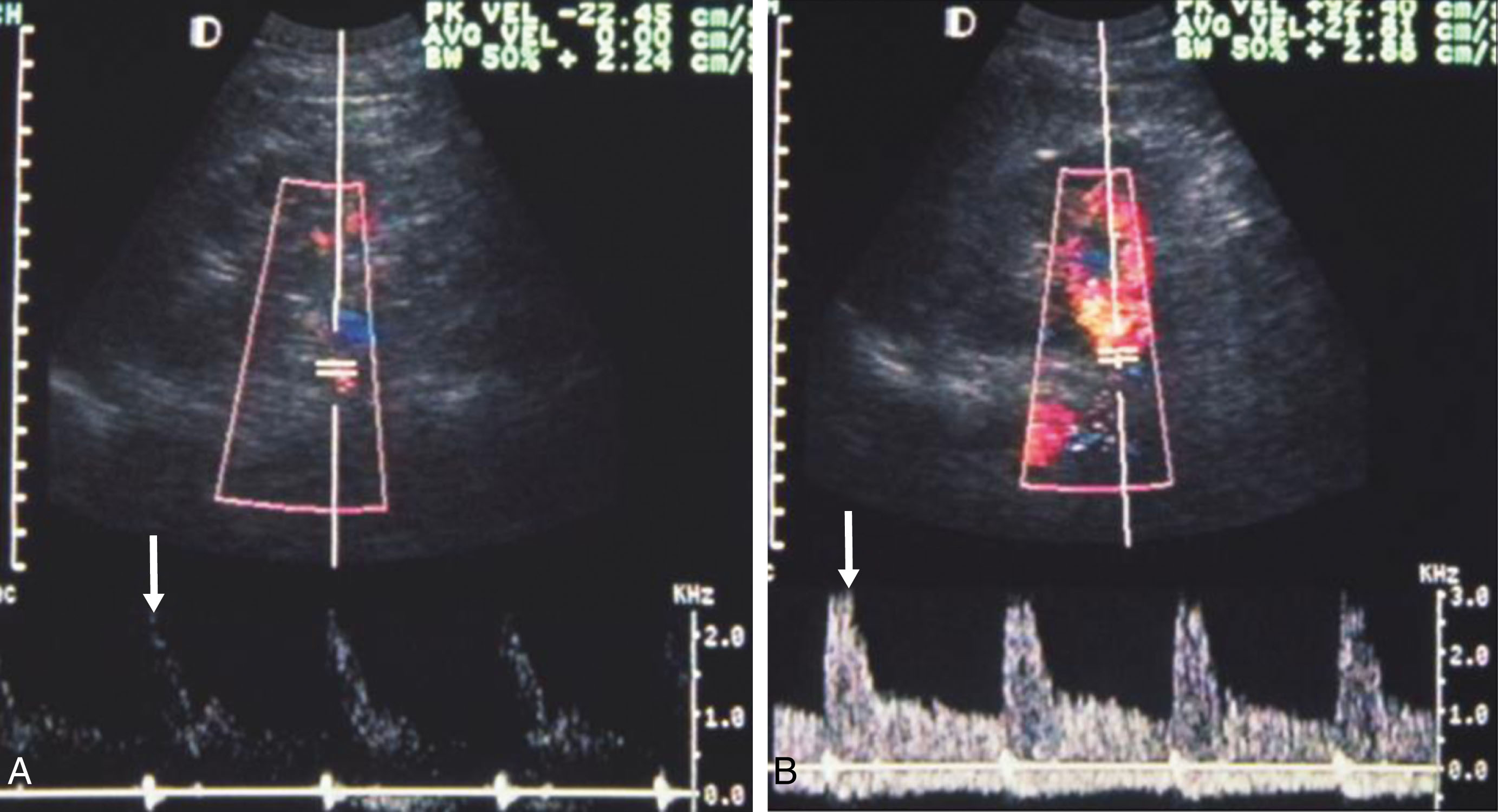
Sonographic detection of blood flow is limited by factors including the depth and size of a vessel, the attenuation properties of intervening tissue, or low-velocity flow. Limitations of ultrasound equipment sensitivity and the operator dependence of Doppler ultrasound are also factors that may affect the results of a vascular examination. UCA are gas microbubbles encapsulated by an outer shell for stability. When injected intravenously, the agents are small enough (<8 μm) to pass through the pulmonary capillary beds but large enough to remain trapped within the vasculature. Vascular or blood-pooling UCAs can enhance Doppler (color and spectral) flow signals by adding more and better acoustic scatterers to the bloodstream ( Figs. 17.1 and 17.2 ). The use of these UCAs improves the color flow imaging detection of blood flow from vessels that are often difficult to assess without their use, such as the renal arteries, intracranial vessels, and small capillaries within organs (i.e., tissue perfusion) ( Fig. 17.3 ). However, contrast-specific imaging modes, which utilize the nonlinear scattering properties of UCAs, provide substantial improvements in contrast-to-tissue signal and improved detection of smaller vessels relative to contrast-enhanced Doppler. These modes are the preferred approach for CEUS imaging and are now available on most mid- to high-end commercial ultrasound scanners.
The concept of a UCA was first introduced by Gramiak and Shah in 1968, who, in their initial work, injected agitated saline directly into the ascending aorta and cardiac chambers during echocardiographic examinations. The microbubbles formed by agitation resulted in strong reflections arising from within the normally echo-free lumen of the aorta and chambers of the heart. Eventually, other solutions were discovered that could produce similar effects. However, microbubbles produced by simple agitation are nonuniform in size, relatively large, and quickly diffuse, which makes them unsuitable for sonographic evaluations of the left heart and systemic circulation because the microbubbles do not persist through passage of the pulmonary and cardiac circulations. Furthermore, to provide contrast enhancement, agitated saline required direct injection into the vessel under evaluation (e.g., the aorta), and a more clinically practicable administration method, such as intravenous (IV) injection, was desired.
For a UCA to be clinically useful, it should be nontoxic, have microbubbles or microparticles that are small enough to traverse the pulmonary capillary beds (i.e., less than 8 microns in size), and be stable enough to provide multiple recirculations. Furthermore, the contrast agent should be administered via IV injection and provide enhancement of ultrasound signals. A number of agents possess these desirable traits, and presently several microbubble-based UCAs are commercially available worldwide ( Tables 17.1 and 17.2 ). Specific UCA properties and their instructions for reconstitution and administration are provided in the product package insert.
| Agent | Approved Indications |
|---|---|
| Optison, GE Healthcare | LVO/EBD |
| Definity, Lantheus Medical Imaging | LVO/EBD |
| Lumason, Bracco International | LVO/EBD, characterization of focal hepatic tumors in adult and pediatric patients, ultrasonography of the urinary tract for the evaluation of suspected or known vesicoureteral reflux in pediatric patients |
| Agent Name | Countries | Approved Indications |
|---|---|---|
| Definity, Lantheus Medical Imaging (marketed as Luminity in some countries) | Canada, Mexico, Israel, New Zealand, India, Australia, European Union, South Korea, Singapore, United Arab Emirates a | LVO/EBD, liver, kidney |
| Optison, GE Healthcare | European Union | LVO/EBD |
| Sonazoid, GE Healthcare AS | Japan, China, South Korea, and Norway |
|
| SonoVue, Bracco International, Milan, Italy | European Union, Norway, Switzerland, China, Singapore, South Korea, Iceland, India, Canada b | LVO/EBD, breast, liver, portal vein, extracranial carotid, peripheral arteries (macrovascular and microvascular) |
a Approved in these countries only for LVO/EBD.
b Approved in Canada for LVO/EBD and diagnostic assessment of vessels.
The specific type of gas contained within a UCA microbubble and its shell composition influence the microbubble’s acoustic behavior (e.g., reflectivity and elasticity), method of metabolism, and stability within the blood. In 1998, Optison (FSO 69; GE Healthcare) was approved by the United States Food and Drug Administration (FDA) for cardiac applications. The microbubbles of Optison are composed of a shell of 5% sonicated human serum albumen that contains a high-molecular-weight gas (perfluoropropane), which extends the stability and plasma longevity of the agent. Optison has shown potential for use with nonlinear harmonic imaging and Doppler modes for echocardiography, as well as systemic vascular, tumor characterization, and abdominal applications.
Similarly, Definity (Lantheus Medical Imaging; marketed as Luminity in some countries) is composed of octafluoropropane microbubble encapsulated in an outer lipid shell. The agent was cleared by the US Food and Drug Administration in 2001 and is indicated for patients with suboptimal echocardiograms to opacify the left ventricular chamber and to improve the delineation of the left ventricular endocardial border. Definity is approved for numerous other applications worldwide and can be used off-label for improved visualization of the vasculature in a variety of clinical applications.
SonoVue (Bracco Diagnostics; marketed as Lumason within the United States) is an aqueous suspension of phospholipid-stabilized sulfur hexafluoride microbubbles which have a low solubility in blood. SonoVue enhances the echogenicity of blood and provides opacification of the cardiac chambers resulting in improved left ventricular endocardial border definition. In clinical trials, it has been shown to increase ultrasound’s accuracy in detection or exclusion of abnormalities in intracranial, extracranial carotid, and peripheral arteries. SonoVue also increases the quality of Doppler flow signals and the duration of clinically useful signal enhancement in portal vein assessments. SonoVue improves the detection of liver and breast lesion vascularity resulting in more specific lesion characterization. SonoVue has been approved for use in Europe for echocardiography and macrovascular applications. In the United States, SonoVue is marketed as Lumason, and it received FDA approval for echocardiography applications in 2014. Lumason has also been studied for liver lesion characterization, and in April 2016, it became the first UCA to gain FDA approval for a radiologic application with the indication for the characterization of focal liver lesions in both adult and pediatric patients. It is also FDA approved for ultrasonography of the urinary tract for the evaluation of suspected or known vesicoureteral reflux in pediatric patients.
The kinetics of UCA microbubbles following IV injection is complex, and each agent has its own unique characteristics. In general, after IV administration, blood-pool UCAs are contained exclusively in the body’s vascular spaces. Once a vascular agent’s microbubbles are ruptured or otherwise destroyed, the microbubble shell products are metabolized or eliminated by the body, and the gas is exhaled.
Tissue-specific ultrasound contrast agents differ from vascular agents in that the microbubbles of these agents are removed from the blood pool and taken up by, or have an affinity toward, specific tissues, for example, the reticuloendothelial system (RES) in the liver and spleen, or thrombi in blood vessels. Over time the presence of contrast microbubbles within or attached to the target tissue changes its sonographic appearance. By changing the signal impedance (or other acoustic characteristics) of normal and abnormal tissues, these agents improve the detectability of abnormalities and permit more specific sonographic diagnoses. Tissue-specific UCAs are typically administered by IV injection. Most tissue-specific UCAs also enhance the sonographic detection of blood flow and are therefore potentially multipurpose. Because tissue-specific UCAs passively target specific types of tissues and their behavior is predictable, they can be considered in the category of molecular imaging agents .
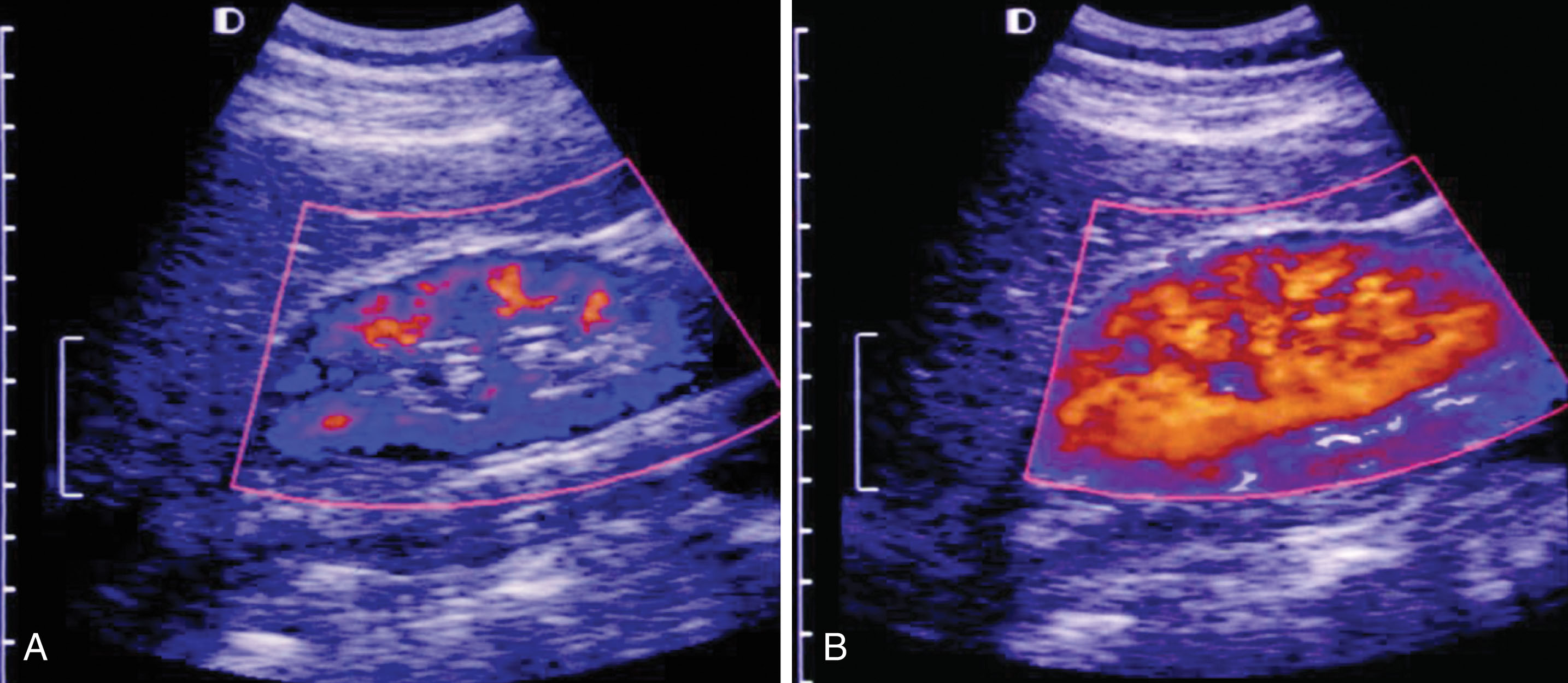
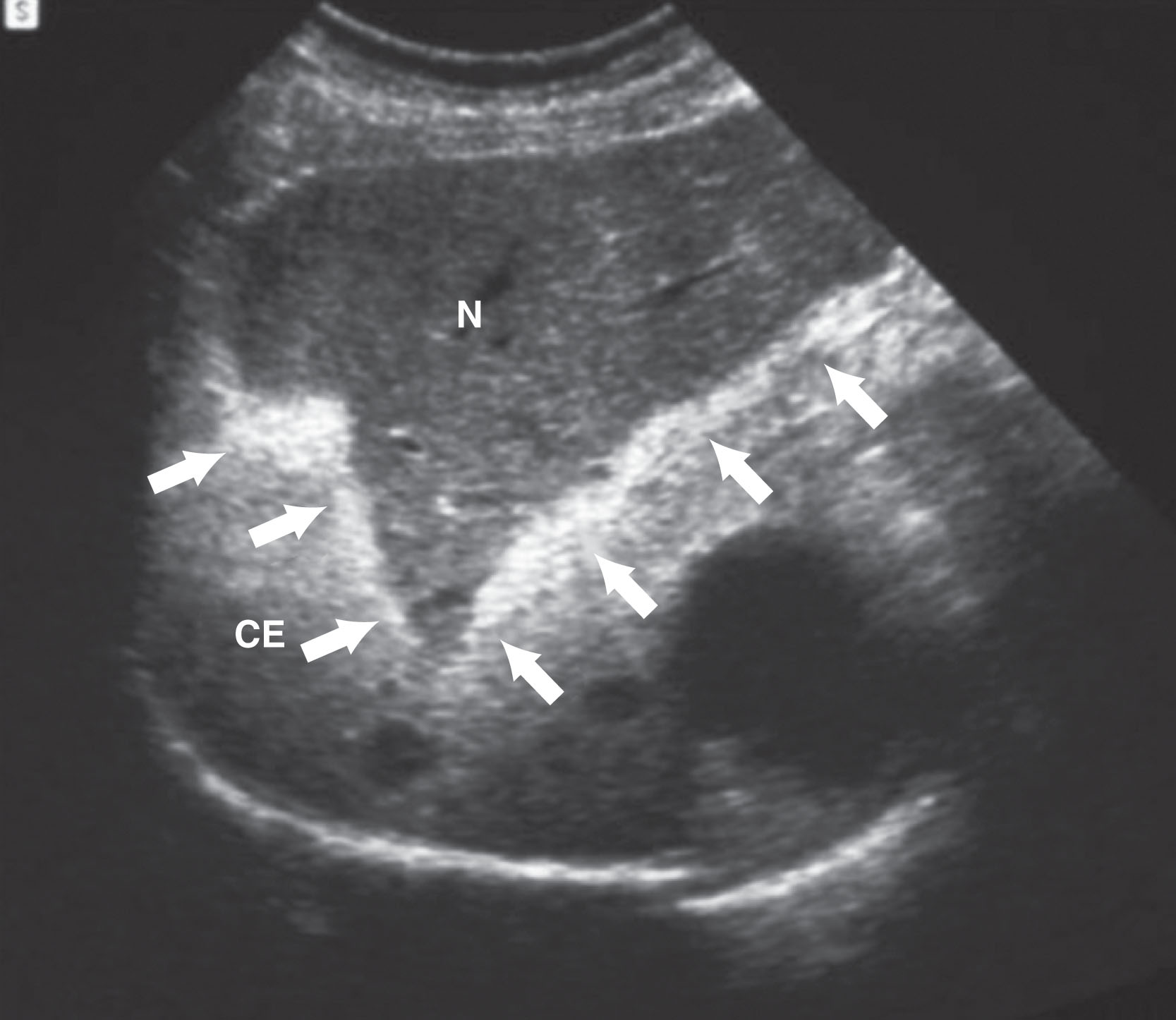
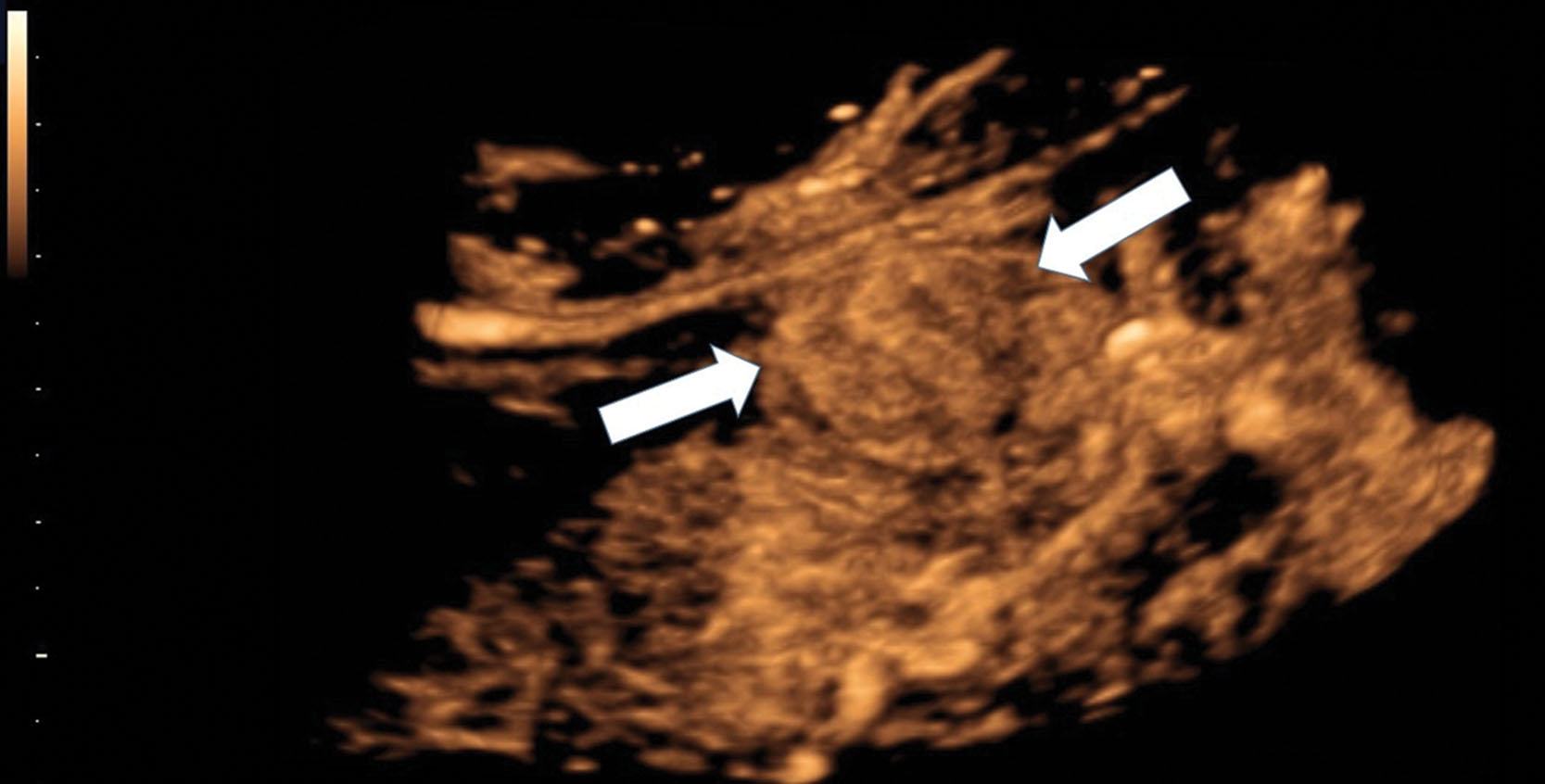
Sonazoid is a tissue-specific UCA that contains microbubbles of perfluorobutane gas in a stable lipid shell. Sonazoid is currently approved for use in Japan, China, Korea, Taiwan, and Norway. After being injected intravenously, Sonazoid behaves as a vascular agent (i.e., enhances the detection of flowing blood) and, over time, the microbubbles are phagocytosed by the RES (macrophage Kupffer cells) of the liver and spleen. The intact microbubbles may remain stationary in the tissue for several hours. When insonated after uptake, the stationary contrast microbubbles increase the reflectivity of the contrast-containing tissue. If an appropriate level of acoustic energy is applied to the tissue, the microbubbles first oscillate (emitting harmonic signals that can be detected with gray-scale CHI) and then rupture. The rupture of the microbubbles results in random Doppler shifts appearing as a transient mosaic of colors on a color Doppler display ( Fig. 17.4 ). This effect has been termed induced acoustic emission (IAE), stimulated acoustic emission (SAE), or simply acoustic emission (AE) . By exploiting the color Doppler–depicted AE phenomenon, masses that have destroyed or replaced the normal Kupffer cells will be displayed as color-free areas and thus become more sonographically conspicuous. These same AE effects can also be demonstrated using gray-scale CHI (see the CHI discussion below) ( Fig. 17.5 ). Improvements in contrast-specific ultrasound imaging technologies have obviated the use of Doppler modes with UCAs for the majority of applications.

Microbubble-based UCAs enhance the detection of blood flow when used with conventional ultrasound imaging techniques, including gray-scale ultrasound and Doppler techniques (i.e., color flow imaging and pulsed wave Doppler with spectral analysis). However, research and experience have led to a better understanding of the nonlinear interactions between acoustic energy (i.e., the ultrasound beam) and UCA microbubbles, which in turn has led to contrast-specific imaging modes that greatly improve the clinical utility of CEUS and obviate the need to use conventional imaging modes with UCAs. Contrast imaging features and capabilities vary by manufacturer, but all utilize proprietary technologies designed to maximize the signal intensity of echoes arising from UCA microbubbles while suppressing echoes from surrounding tissue.
Harmonic imaging (HI) uses the same broadband transducers used for conventional ultrasound, but in HI mode, the system is configured to receive only echoes at the second harmonic frequency, which is twice the transmit frequency (e.g., 7.0 MHz for a 3.5-MHz transducer). When using a microbubble-based UCA, the microbubbles oscillate (i.e., they get larger and smaller) when subjected to the acoustic energy present in the ultrasound field. The reflected echoes from the oscillating microbubbles contain energy components at the fundamental frequency and at the higher and lower harmonics (i.e., subharmonics). Contrast harmonic imaging (CHI) allows detection of UCA microbubbles by imaging the nonlinear harmonics. The use of CHI for CEUS avoids many of the limitations and artifacts encountered when using Doppler techniques and UCAs, such as angle dependence and “color blooming” artifacts. In CHI mode, the echoes from the oscillating microbubbles have a higher signal-to-noise ratio than would be provided by using conventional ultrasound so that regions with microbubbles (e.g., blood vessels and organ parenchyma) are more easily appreciated visually. Advanced CHI technology (e.g., coded-pulse HI, wideband HI, phase-inversion HI, and pulse-inversion HI) employ either image processing algorithms to subtract echoes arising from body tissues while echoes arising from contrast microbubbles are preferentially displayed or nonlinear pulses to maximize the generation of harmonic signal. Thus, CHI provides a way to better differentiate areas with and without contrast and has the potential to demonstrate real-time grayscale blood-pool imaging (i.e., perfusion imaging). Similarly, techniques using a combination of phase and amplitude pulse modulation, such as cadence contrast pulse sequencing (CPS), are commercially available to maximize nonlinear signals while reducing linear tissue signal. The benefits of using nonlinear imaging techniques for CEUS (e.g., higher frame rates, improved contrast resolution, reduced artifacts) are so great that conventional color flow imaging is neither necessary nor advised.
When using microbubble-based UCAs, the energy present within the acoustic field can have a detrimental effect on the contrast microbubbles. A significant number of the microbubbles can be destroyed by the acoustic pressure even though the actual pressure contained within the ultrasound field is relatively low. Once the microbubble is destroyed, contrast enhancement is no longer provided, which reduces the clinical utility and duration of contrast enhancement. Several approaches have been used to minimize this problem. One relatively easy technique is to use a low acoustic output power as defined by the mechanical index (MI) . However, reducing the MI also limits tissue penetration, so this is not always an adequate solution. Furthermore, the MI may be an imprecise predictor of the effect of acoustic energy on contrast microbubbles. Current scanners that have CEUS packages provide exam presets that use low (<0.2) MI values to avoid microbubble destruction during continuous imaging.
Some equipment manufacturers have incorporated intermittent imaging (also referred to as interval delay imaging ) capabilities on their systems to provide an additional option to the user seeking to reduce microbubble destruction during CEUS examinations. In this mode, the system is gated to only transmit and receive data at predetermined intervals. The gating may be triggered on a specific portion of the electrocardiogram (e.g., the r-wave) or a time interval such as once or twice per second.
A manual approach to intermittent imaging can also be used to reduce the exposure of contrast microbubbles to the acoustic energy and prolongs the duration of contrast enhancement. This approach is especially useful for evaluating late tumor washout as described in the hepatic applications below. Using this approach, scanning is paused for a duration (generally 20 to 30 seconds) with short clips of the area of interest obtained at set time intervals. A disadvantage to intermittent imaging is its lack of a real-time display of data, which can cause technical challenges, but this technique is helpful in detecting low levels of contrast enhancement and for prolonging the duration of contrast enhancement.
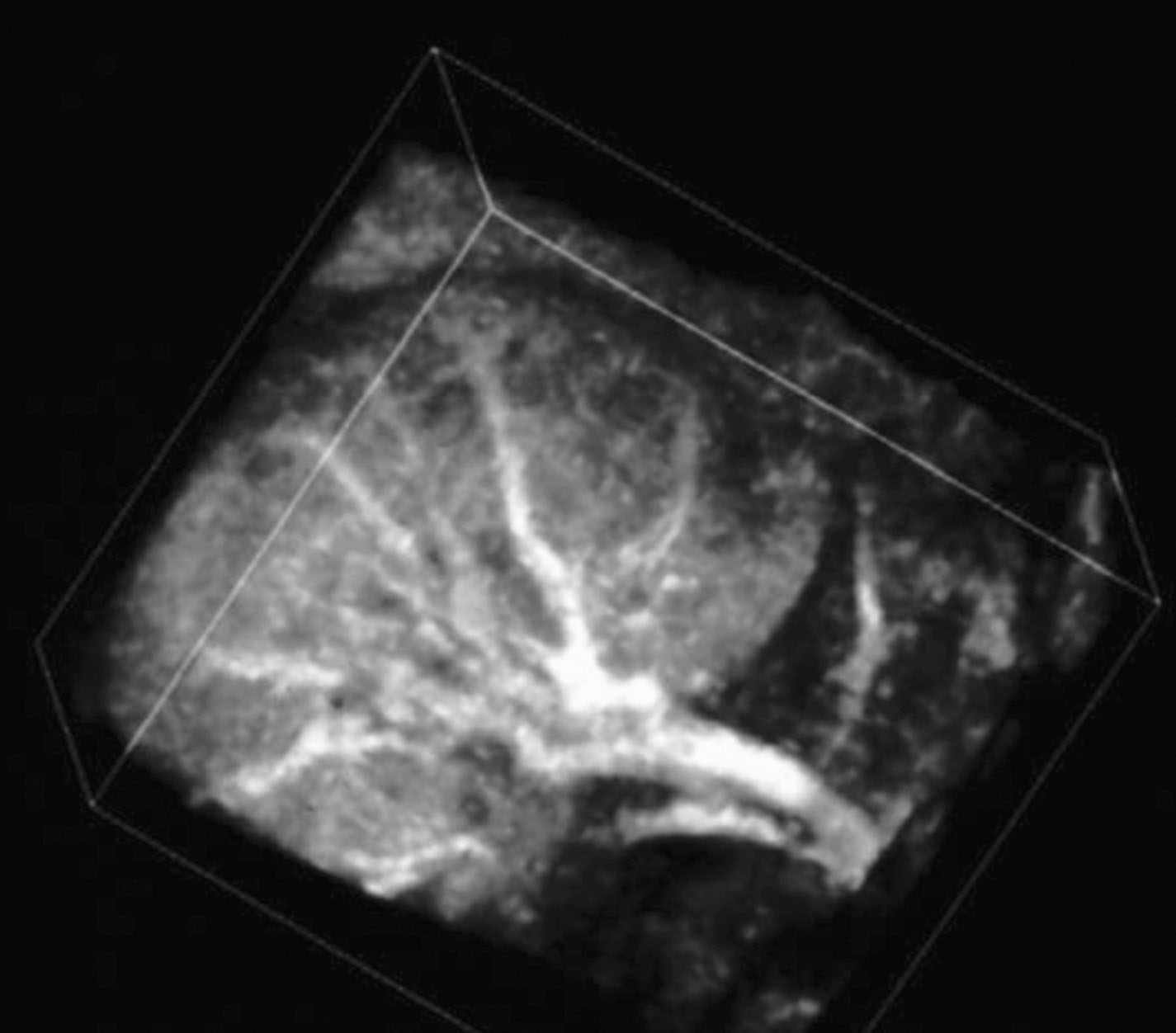
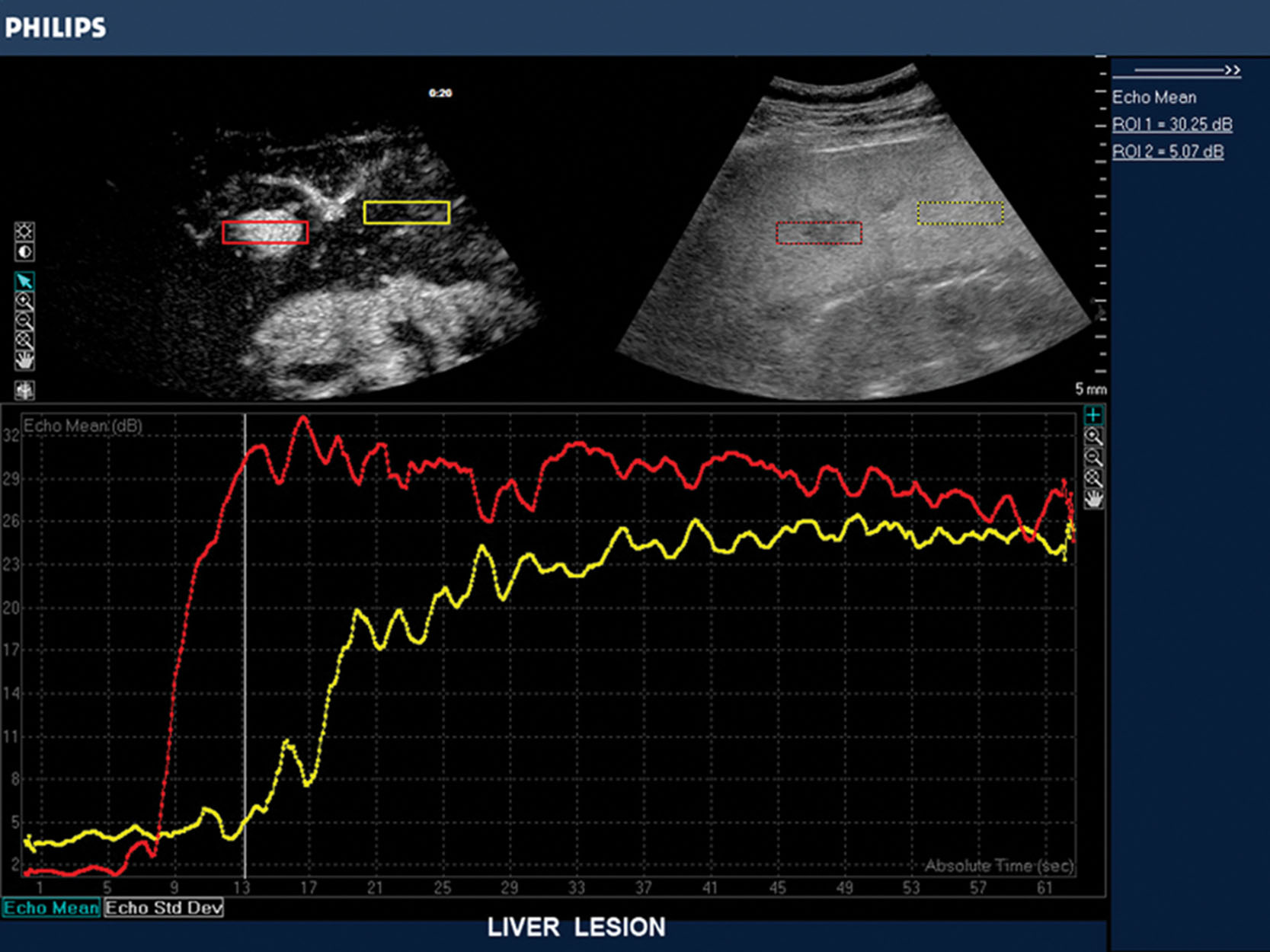
Other contrast-specific technologies include advanced three-dimensional (3D) and four-dimensional (4D) imaging ( Figs. 17.6 and 17.7 ). Furthermore, a number of contrast-specific measurements and calculations can be performed, including onboard video densitometry, calculation of the integrated backscatter from contrast, measurement of the transit time of contrast-containing blood through normal and diseased tissue, estimations of blood volume, and assessment of tissue perfusion differences in solid organs. Systems have been developed that allow onboard calculation of the unique data provided by the use of UCAs ( Fig. 17.8 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here