Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Clinical practice in obstetrics and gynecology, based upon the principles of safe, ethical and value-based care, is facilitated by viewing wellness and sickness in the context of a life-course perspective. Effective clinical care of mother and child must begin early, even before conception, and continue throughout life.
Adaptive developmental plasticity and epigenetic modification of genes during and after pregnancy can have a significant impact on chronic diseases later in life.
Clinicians should incorporate the major ethical principles of nonmaleficence, beneficence, autonomy, and justice into their practices, along with the duties and ideals of confidentiality and multidisciplinary collaboration.
Regulatory, economic, and public pressure make assessment and improvement of safety and value essential in the delivery of women's health care. Optimal health outcomes can only be achieved when principles from continuous quality assessment and high reliability organizations are combined with the systematic approach of safety science and evidence-based medicine.
The promising area of clinical preventive services in obstetrics and gynecology, as in all heath care, is transforming the practice of medicine in a very positive way.
This chapter of Essentials of Obstetrics and Gynecology is being revised at a time when the health and wellness of the population of the United States and some other developed countries of the world are being evaluated and questioned. A recent study by the Harvard Business School conducted by Professor Michael Porter and his team ranked the United States only 70th in the world in terms of overall health and wellness. Despite the fact that the United States spends far more on health care (nearly 18% of gross domestic product or GDP) than any other nation, it continues to be ranked only about 37th out of 191 nations for health status and health system performance. Further, the United States is ranked only 46th for average life-expectancy and 42nd for infant mortality by the World Health Organization (WHO). Clearly, the United States must strive to improve its standing on these and other measures of performance. This is especially important at a time when the health care delivery system enters the era of the Affordable Care Act (ACA), and efforts to provide care to all citizens at a reasonable cost are underway.
Obstetrics and gynecology is one of the most exciting and challenging areas of health care, with a number of significant opportunities for improvement such as infant and maternal mortality. The specialty provides students and young physicians in training with the knowledge and skills necessary to improve the health of women and their children very early in their lives. In this first chapter of the book, some basic principles and guidelines for improving health care are provided, and several important factors that are influencing the health of women and their children are suggested.
There are four basic principles for practicing and improving health care. First, the safety of our patients must always be paramount. In recent years we have made major improvements in patient safety, in large part by emphasizing teamwork and implementing practices proven to be effective in the airline industry. Second, we must be true to our personal pledge made when taking the Hippocratic Oath—to adhere to ethical practices. Third, we must transform to a value-based system of health care delivery. Because medicine has become very complex, we must be open to a more cost-effective multidisciplinary approach to both diagnostic and therapeutic practice. Performance improvement efforts, practice management skills, and effective communication are all necessary to efficiently optimize clinical outcomes and value. Fourth, and perhaps most importantly, we must focus on the prevention and early mitigation of disease, in addition to our continued focus on its treatment. This should occur in a patient-centered manner, meeting their needs and expectations.
For this reason, we emphasize an approach called a life-course perspective for clinical practice, beginning with preconception health, continuing throughout pregnancy, the postpartum period (interconception health), and then giving children and their mothers a health perspective for adopting and maintaining healthy living.
Before delving more deeply into these principles of practice (safety, ethics, value, and prevention), some newer concepts about the origins of disease are important to mention.
When does disease begin and lead to pathology and illness during the course of life?
First, although genetics is beginning to provide a much better understanding of the etiology of poor health, it probably accounts for only about one-third of the direct causes. Imprinted genes from both the mother and the father play an important role in passing on characteristics to the offspring. This imprinting process maintains the phenotype of the family in subsequent generations. However, some imprinted and nonimprinted genes can be upregulated or downregulated by subsequent epigenetic modifications, due to environmental influences. For example, person X with gene A has a disease but person Y with the same gene does not. Clearly there is more to human development and disease risk than genetic makeup. Currently it is thought that factors such as poverty or abnormal health behaviors (poor nutrition and smoking) and/or environmental conditions can influence the expression of gene A without actually changing its genomic makeup. This may occur directly or these factors may activate another gene, A-2 downstream, which may then affect gene A. This process whereby human cells can have the same genomic makeup but different characteristics is referred to as epigenetics (literally meaning “on top of genetics”), an exciting new frontier.
The developmental origins of adult disease hypothesis (Barker hypothesis) postulates that perturbations in the gestational environment may influence the development of adult diseases such as cardiovascular disease, obesity, diabetes, and stroke. Current evidence suggests that this occurs through the reprogramming of gene expression via epigenetic changes in chromatin structure. Epigenetic changes in chromatin structure include altered DNA methylation by both histone acetylation and methylation.
Since the last edition of this text, investigators have determined that alterations in the in utero environment during pregnancy may result in modifications to the chromatin structure. These modifications may lead to persistent changes in postnatal gene expression which may render the child more susceptible to early onset adult disease. The conditions during pregnancy that account for these epigenetic changes are preeclampsia, preterm birth, intrauterine growth restriction (IUGR), obesity, diabetes, poor nutrition, smoking, and some cancers. Even the mothers with these pregnancy conditions are themselves at greater risk for cardiovascular disease, hypertension, and diabetes later in life. The onset for these conditions occurs earlier in life compared to those women who have normal pregnancies. Thus having a normal pregnancy may be protective of disease later in life.
It is now thought that the effect of harmful behaviors and our environment on the expression of our genes may account for up to 40% of all premature deaths in the United States. Two of the top behavioral factors related to this premature death rate are obesity (and its usual physical inactivity) and smoking. Environmental exposures to metals, solvents, pesticides, endocrine disruptors, and other reproductive toxicants are also major concerns.
Second, in human biology, a phenomenon called adaptive developmental plasticity plays a very important role in helping to adjust behavior to meet any environmental challenge. In order to understand human development over time (a life-course perspective), one must first understand what is normal and what adverse circumstances may challenge and then change normal development of the fetus. These protective modifications of growth and development which are programmed in utero to prevent fetal death, may become permanent. The price the fetus may pay for short-term survival is later vulnerability to conditions such as obesity, hypertension, insulin resistance, atherosclerosis, and even diabetes.
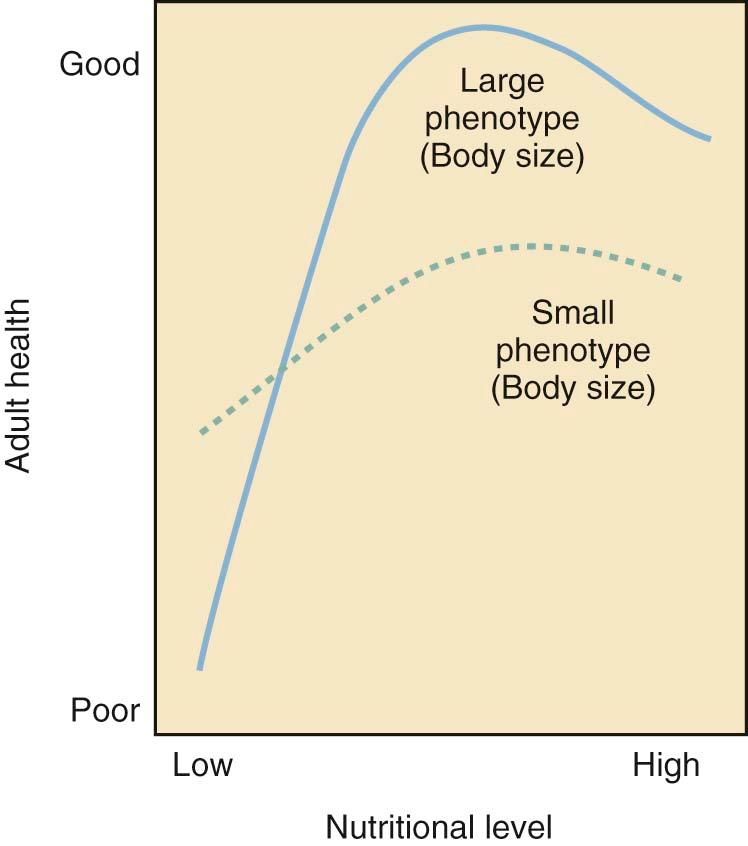
In relation to individual X and individual Y with the same genomic makeup but different in utero environmental influences, metabolic changes that may be initiated in utero in response to inadequate nutritional supplies ( Figure 1-1 ) can lead to insulin resistance and eventually the development of type 2 diabetes. These adaptive changes can even result in a reduced number of nephrons in the kidneys as a stressed fetus conserves limited nutritional resources for more important organ systems in utero. This can then lead to a greater risk of hypertension later in life.
This series of initially protective but eventually harmful developmental changes was first described in humans by David Barker, a British epidemiologist, who carefully assessed birth records of individuals and linked low birth weight (<2500 grams) to the development of hypertension, diabetes, atherosclerosis, and stroke later in life. The association between poor fetal growth during intrauterine life, insulin resistance, and cardiovascular disease is known as the Barker hypothesis. The process whereby a stimulus or insult, at a sensitive or critical period of fetal development, induces permanent alterations in the structure and functions of the baby's vital organs is now commonly referred to as developmental programming.
Third, another important concept in the life-course perspective is allostasis, which describes the body's ability to maintain stability during physiologic change. A good example of allostasis is found in the body's stress response. When the body is under stress (biological or psychological), it activates a stress response. The sympathetic system kicks in and adrenalin flows to make the heart pump faster and harder (with the end result of delivering more blood and oxygen to vital organs including the brain). The hypothalamic-pituitary-adrenal (HPA) axis is also activated to produce more cortisol, which has many actions to prepare the body for fight or flight.
Normally, as soon as the fight or flight is over, the stress response is turned off. The body's sympathetic response is counteracted by a parasympathetic response, which fires a signal via the vagal nerve to slow down the heart, and the HPA axis is shut off by cortisol via negative feedback mechanisms. Negative feedback mechanisms are common to many biological systems and work very much like a thermostat. When the room temperature falls below a preset point, the thermostat turns on the heat. Once the preset temperature is reached, the heat turns off the thermostat. Stress turns on the HPA axis to produce cortisol. Cortisol, in turn, turns off the HPA axis to keep the stress response in check.
This stress response works well for acute stress but it tends to break down under chronic stress. In the face of chronic and repeated stress, the body's stress response is always turned on, and over time will wear out. The body goes from being “stressed” to being “stressed out”—from a state of allostasis to allostatic overload. This describes the cumulative wear and tear on the body's adaptive systems from chronic stress. Helpful physiologic mechanisms that initially protect may eventually be harmful.
The life-course perspective synthesizes both the developmental programming mechanisms of early life events and allostatic overload mechanisms of chronic life stress into a longitudinal model of health development. It is a way of looking at life not as disconnected stages, but as an integrated continuum. Thus to promote a healthy first pregnancy, preconception health should be a priority. To promote preconception health, adolescent health must be provided to young girls so that as women having children, they are free of diseases such as diabetes, hypertension, and obesity and have been encouraged to eat a healthy diet and to abstain from using tobacco products. Rather than episodic care that many women now receive, as a specialty we must strive toward disease prevention and health promotion over the continuum of a woman's life.
The public health implications of the Barker hypothesis and other life-course events are significant. This is the beginning of an exciting era in medicine where young physicians and other health care professionals can begin to take charge of these events and change our health care delivery system in a very positive way. Patients should be encouraged to take responsibility for improving their own health, particularly by practicing healthy behaviors early in life. They should also be encouraged to improve and maintain a healthy “green” environment. Currently there are only a few environmental and behavioral factors that have been clearly identified as part of the Barker hypothesis. Many others are yet to be discovered.
Adaptive developmental plasticity will take place secondary to changes in genes as a result of environmental and behavioral practices. Even the controversial concept of climate change may play a role in this phenomenon. Biological processes are very powerful and frequently unpredictable. Physicians must increasingly strive for a safe, ethical, and value-based practice.
In order to facilitate the improvement of the health and wellness of women and children, four basic principles of practice should guide our strategy: patient safety, ethical practice, value, and the need for a patient-centered focus on prevention, as follows.
Safety in health care is not a new concept. Facilities have had safety programs in place since the early 1900s, but these programs have traditionally focused on emergency preparedness, environmental safety, security, and infection control. The term patient safety, meaning avoidance of medical error, was first coined by the American Society of Anesthesiologists in 1984, when they inaugurated the Anesthesia Patient Safety Foundation to give assurance that the effects of anesthesia would not harm patients.
Medical errors now rank as the fifth leading cause of death in the United States. The Institute of Medicine (IOM) published an alarming report in 1999 called To Err Is Human: Building a Safer Health System . This report estimated that between 44,000 and 98,000 Americans die each year as a result of medical errors. Error is defined as failure of a planned action to be completed as intended (e.g., failing to operate when obvious signs of appendicitis are present) or the use of a wrong plan to achieve an aim (e.g., wrong diagnosis, wrong medication administered). Medication errors alone, occurring either in or out of the hospital, are estimated to account for over 7,000 deaths annually. According to the National Council on Patient Information and Education, “more than 2/3 of all physician visits end with a prescription.” An estimated 39-49% of all medication errors occur at the stage of drug ordering. Patient noncompliance also contributes to medical errors.
The U.S. Pharmacopoeia (USP) MedMARx error tracking service estimates that as many as 100,000 medication errors occur annually. Because reporting is voluntary and does not include all medical facilities in the United States, the scope of the problem is likely to be much larger. A preventable adverse drug event (ADE) is one type of medication error. Administering the incorrect drug, an incorrect dose, wrong frequency, or incorrect route may cause an ADE.
A drug that cures one patient's condition may be the one that causes another patient's injury or death due to an adverse drug reaction (ADR). The latter may account for 1 out of 5 injuries or deaths for hospitalized patients. ADRs commonly occur from an overdose, a side effect, or an interaction among several concomitantly administered drugs. In order to minimize ADRs, health care providers should avoid the following actions:
Prescribing unnecessary medications
Treating mild side effects of one drug with a second, more toxic drug
Misinterpreting a drug's side effect for a new medical problem and prescribing another medication
Prescribing a medication when there is any uncertainty about dosing
In the absence of automated systems, providers should strive to write legibly and use only approved abbreviations and dose expressions. Most health care facilities publish and circulate an acceptable list of appropriate abbreviations, as a means of reducing medication errors.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here