Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Nasal obstruction in neonates can cause respiratory distress and feeding difficulty, as newborns rely heavily on nasal breathing.
Mild cases of nasal obstruction can be observed, but severe obstructive lesions can be life-threatening and usually require early surgical intervention.
Further workup may be needed to identify any associated conditions and syndromes.
Neonatal rhinitis may respond to short-term intranasal corticosteroid treatment.
Early reduction of severe neonatal nasal septal deformity can relieve nasal airway obstruction.
Ophthalmology and otolaryngology evaluations are helpful for the management of dacryocystoceles.
Infants with congenital pyriform nasal aperture stenosis and midnasal stenosis can often be observed, but severe cases of obstruction may require intranasal surgery with stenting.
Choanal atresia is usually repaired through a transnasal endoscopic approach, and bilateral choanal atresia is repaired in the neonatal period.
A neonate with an intranasal mass requires imaging with computed tomography and/or magnetic resonance imaging before biopsy or excision to define anatomy and look for intracranial extension.
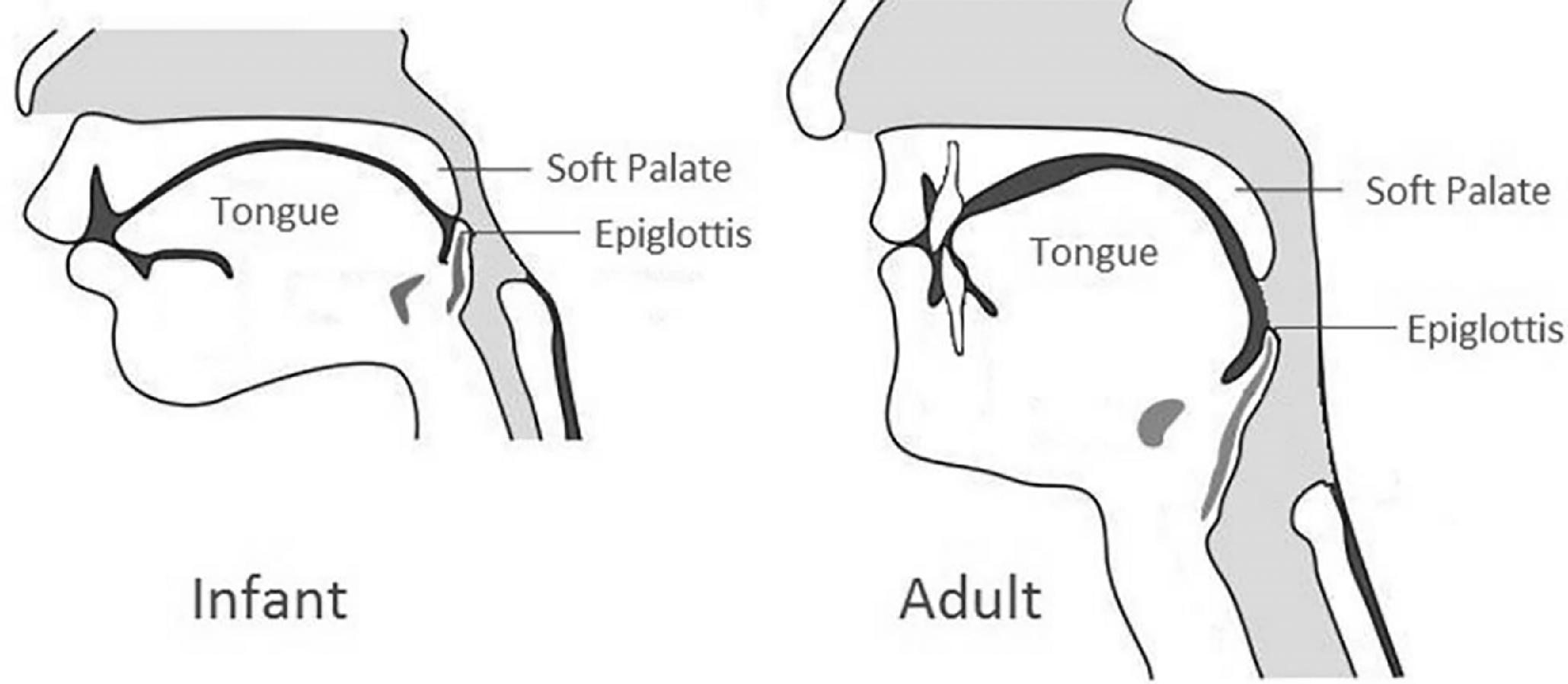
Neonates are generally considered obligate, or at least preferential, nasal breathers. The neonatal upper airway anatomy predisposes to such obligate nasal breathing ( Fig. 70.1 ). The tongue sits in contact with the soft and hard palate, which obstructs oral breathing. The larynx is higher, putting the epiglottis superior to the soft palate and separating the nasal breathing passage from the passage of liquid from the mouth. This neonatal anatomy maximizes the ability to breathe during oral feeding. Neonatal nasal obstruction may not be apparent until respiratory difficulties are noted during oral feeding. Nasal obstruction in a newborn usually requires prompt evaluation, typically with otolaryngology consultation. Although the potential underlying causes of nasal obstruction are numerous, congenital and traumatic causes are most common ( Table 70.1 ).
| Congenital Nasolacrimal duct cyst/dacryocystocele Midnasal stenosis Congenital pyriform aperture stenosis (CNPAS) Choanal atresia Midfacial hypoplasia Nasal hypoplasia Nasal dermoid Glioma Encephalocele Thornwaldt cyst Cleft lip nasal deformity Traumatic Nasal septal deviation from intrauterine pressure or difficult delivery Iatrogenic Nasal septal deviation from assisted delivery Irritation and scarring from: traumatic nasal suctioning nasal cannula or noninvasive positive pressure ventilation prongs nasogastric tubes Rhinitis medicamentosa from long-term topical decongestant use Infectious Viral or bacterial upper respiratory infection Vertical transmission of sexually transmitted infection (chlamydia, gonorrhea, syphilis) Neoplasms Teratoma Hamartoma Sarcoma Neurofibroma Lipoma Chordoma Lymphoma Hemangioma Lymphovascular malformations Endocrine Rhinitis from circulating maternal estrogen Hypothyroidism Other Rhinitis Idiopathic |
The following causes of neonatal nasal obstruction will be reviewed more in depth: neonatal rhinitis, nasal septal deviation, nasolacrimal duct cyst/dacryocystocele, congenital nasal pyriform aperture stenosis (CNPAS), midnasal stenosis, choanal atresia, and midline congenital nasal masses.
Neonatal nasal obstruction can present with various signs of abnormal breathing and feeding ( Table 70.2 ).
| Noisy breathing—stertor or snoring |
| Grunting or snorting |
| Nasal flaring |
| Retractions |
| Cyclic respiratory distress that is temporarily relieved with crying |
| Perioral cyanosis, may be cyclic |
| Apnea |
| Difficulty feeding |
| Nasal drainage |
| Inability to pass a suction or scope through the nose and into the pharynx |
| External nasal deformity |
| Epiphora |
When nasal obstruction is suspected, examination should begin with evaluation of the external nasal and facial appearance. The exam should focus on the nasal contour and identifying any other facial anomalies. Anterior rhinoscopy can be performed with an otoscope or nasal speculum. Attempts should be made to pass a 5 or 6 French suction catheter through each side of the nose into the nasopharynx. Because these catheters may coil in the nose against an obstruction, visualizing the catheter in the posterior pharynx is reassuring. Attempts to pass a catheter should not be made if there is any concern for a skull base defect. An alternative is the mirror test, where a mirror is placed in front of each nostril; fog should appear if the nasal airway is patent. If a catheter cannot be passed or other concerning findings are present, then an otolaryngology consultation should be obtained.
The consulting otolaryngologist will likely examine the nasal cavities and nasopharynx with nasal endoscopy with a flexible fiberoptic scope. This is a simple bedside procedural examination that can be performed without sedation and with minimal risks. Endoscopy may be done before and after decongesting with topical oxymetazoline or phenylephrine to determine the impact of mucosal edema compared with a fixed, anatomic obstruction.
Imaging is usually performed before surgical intervention on any nasal mass or congenital obstruction, with the exception of septal deviation. Computed tomography (CT) scan is best to delineate bony anatomy and is usually the best initial study when CNPAS, midnasal stenosis, or choanal atresia are suspected. Magnetic resonance imaging (MRI) is preferred for lesions that may extend intracranially, such as dermoid cysts, gliomas, or encephaloceles ( Table 70.3 ).
|
Fetal imaging, including ultrasound and/or MRI, may suggest craniofacial anomalies or airway obstruction prior to delivery. When severe anomalies are present and airway obstruction at delivery is predicted, ex-utero intrapartum treatment at delivery can be planned to secure the airway while maintaining maternal-fetal circulation before completing delivery. Ex-utero intrapartum treatment is not usually needed for anomalies that are limited to the nose.
Additional airway or pulmonary abnormalities should be identified. Stridor, wheezing, and persistent hypoxia are unusual for isolated nasal obstruction and should raise suspicion for another condition.
In cases of mild or unilateral nasal obstruction, the need for and timing of intervention may be unclear. Polysomnography can be performed to determine the severity of obstruction during sleep and the presence of apnea/hypopnea, oxygen desaturation, or hypercarbia. A normal polysomnogram can support initial observation rather than early surgery for newborns with low-grade nasal obstruction.
Many neonates with nasal obstruction may not be able to coordinate breathing and effective swallowing. Swallowing dysfunction can persist even after treatment of the nasal obstruction. A clinical swallowing assessment by a speech-language pathologist or occupational therapist should be considered, supplemented by a videofluoroscopic swallow study or fiberoptic endoscopic evaluation of swallowing when swallow dysfunction is apparent. Severe feeding difficulties may indicate earlier surgery for correctable nasal lesions.
Gastroesophageal reflux (GERD) is seen in many newborns with airway obstruction. Airway obstruction for nasal pathology can increase intrathoracic pressure and worsen GERD. Untreated GERD may contribute to restenosis of a nasal obstruction after surgical management if refluxate comes in contact with the healing surgical site. Pharmacologic and nonpharmacologic management of GERD should be considered, as well as gastroenterology consultation in recalcitrant cases.
Genetics evaluation with appropriate testing is indicated for many neonates with nasal obstruction as we recognize the association of some nasal pathology with syndromic diagnoses. Specific indications will be reviewed in this chapter as related to specific clinical findings.
Initial management of any critical nasal airway obstruction involves maintaining an adequate airway with either appropriate positioning, an oral airway, a McGovern nipple (an oropharyngeal airway made by cutting off the end of a large feeding nipple and securing it in the mouth with tape around the head), or intubation. When using an oral airway or McGovern nipple, feeding can be done with intermittent removal of the airway or with gavage feeds. Nasal trumpets (for newborns with narrow but not totally occluded nasal airways), and noninvasive positive pressure ventilation can be used to temporize until definitive treatment or resolution of the obstruction.
Neonatal rhinitis is considered the most common cause of neonatal nasal obstruction. More neonates present with this in the fall and winter months. There is no apparent race or gender propensity.
Inflammation of the nasal mucosa in neonatal rhinitis can range from mild to severe and be due to both maternal and neonatal factors ( Table 70.4 ). , ,
| Viral upper respiratory infection |
| Vertical transmission of sexually transmitted infection (chlamydia, gonorrhea, syphilis) |
| Maternal estrogen |
| Maternal medications (methimazole, methyldopa, opiates, tricyclic antidepressants, propranolol) |
| Maternal cocaine |
| Cow’s milk allergy |
| Gastroesophageal reflux |
| Cystic fibrosis |
| Kartagener’s syndrome |
| Hypothyroidism |
| Idiopathic |
Anterior rhinoscopy and nasal endoscopy show edematous nasal mucosa and rhinorrhea. However, a 5 or 6 French suction catheter can still be passed through the edematous soft tissue.
Close observation is recommended because resolution is common. A short trial of topical decongestant (oxymetazoline or phenylephrine) may be helpful. Phenylephrine has been given safely to infants 3 weeks to 12 months of age for viral bronchitis in a randomized controlled trial. Hemodynamic effects on blood pressure and heart rate have been seen intraoperatively and postoperatively with oxymetazoline use in surgery. Oxymetazoline has been given safely to children in an observational study of nasolacrimal surgery and a randomized controlled trial of nasal surgeries on the sinuses, turbinate, and adenoids, but clinical studies have not evaluated it in neonates. , These medications should be dosed judiciously in neonates who are also being clinically monitored. Regular use of topical decongestants for more than a few days should be avoided because of the risk of causing rhinitis medicamentosa with worsened nasal obstruction.
Nasal saline drops and suction can help, especially in the setting of thick or dried nasal drainage. If breathing and feeding do not improve, then dexamethasone ophthalmic drops in the nose usually result in a rapid improvement over days. The majority of 20 neonatal intensive care unit patients in one case series showed improvement with this stepwise medical management of nasal saline and topical decongestants and then a topical steroid for persistent symptoms. Imaging is not usually needed but is reserved for cases where symptoms persist and other obstructive lesions need to be ruled out.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here