Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Brain malformations are a significant source of morbidity and death in neonates.
Advances in imaging and genetics now allow more specific diagnoses.
Early and specific diagnosis allows more precise prognostication, including improved monitoring for complications and treatment decisions.
Early diagnosis and management of patients with brain malformations require multidisciplinary team management.
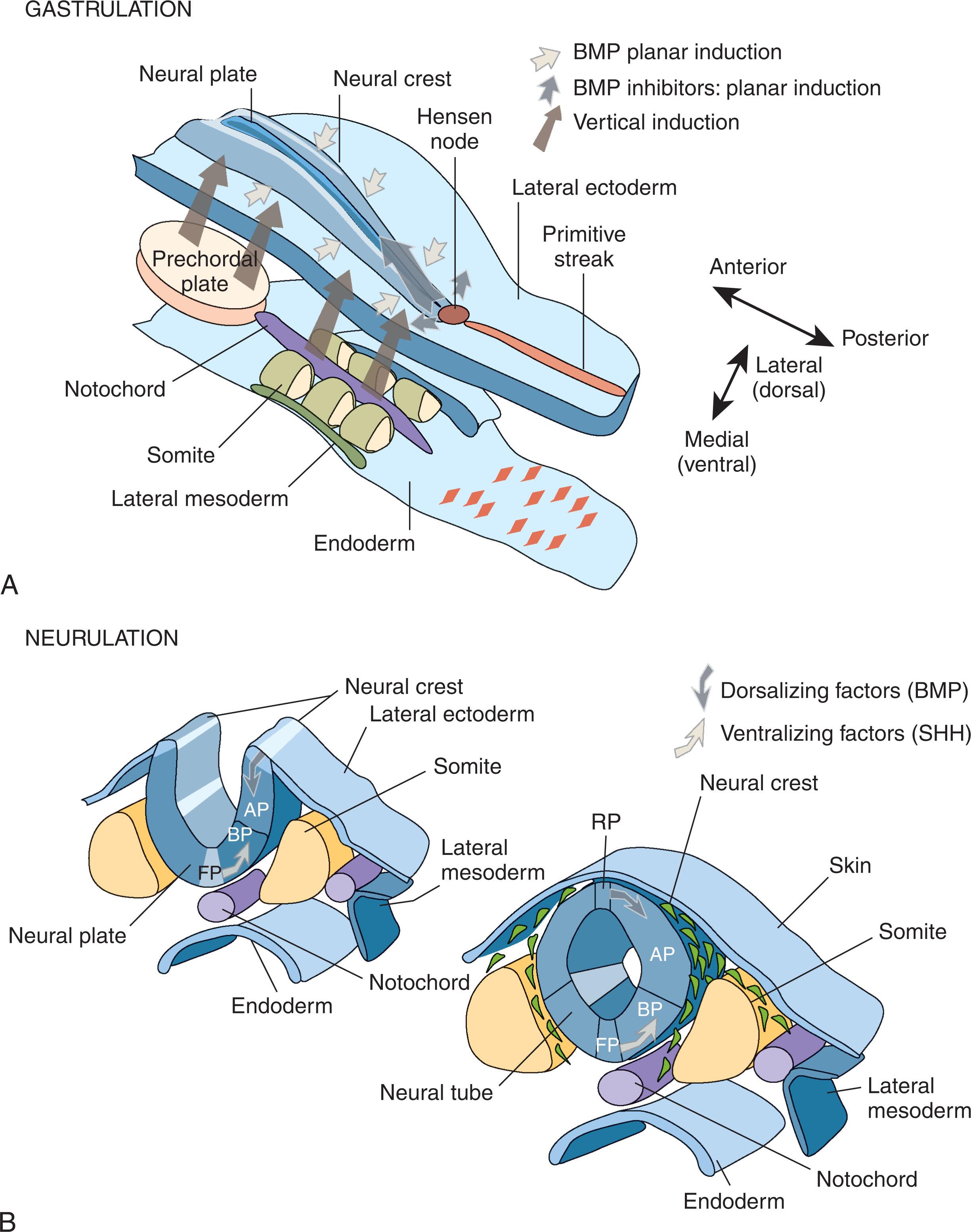
The prosencephalon refers to the future forebrain, which includes the telencephalon and the diencephalon; these structures give rise to the cerebral hemispheres, thalamus, and hypothalamus. The prosencephalon develops after the closure of the anterior neuropore, through processes that induce the bifurcation of the rostral extent of the fluid-filled neural tube ( Fig. 53.1 ) to form the right and left forebrain structures. During the fifth and sixth weeks of development, the structure of the forebrain is defined by cleavage along three major planes. As the anterior neuropore is closing, the first major event is the formation of the optic vesicles and nasal placodes, separated along the horizontal plane. When the embryo has reached a length of about 5 mm, both anterior and posterior neuropores have closed, isolating the developing ventricular system from the amniotic fluid. The retinal and lens placodes also develop at this time. In the hindbrain, the cerebellum begins to form, along with somatic and visceral efferent nuclei, the common afferent tract, and the ganglia for most of the cranial nerves. At about day 32 of gestation, when the embryo is 5 to 7 mm long, the forebrain divides in the sagittal plane to give rise to the paired structures. Specific areas, including the hypothalamic, amygdala, hippocampal, and olfactory regions, are identifiable at this time. The third major event in forebrain development occurs shortly thereafter when the forebrain divides in the coronal plane. This event separates the telencephalon from the diencephalon, defining the epithalamus, subthalamus, and hypothalamus. During the remainder of the second and third months of gestation, multiple midline structures form, including the corpus callosum, anterior and hippocampal commissures, optic nerves, optic chiasm, and hypothalamus.
Disorders of development of the prosencephalon include the severe malformations: atelencephaly, aprosencephaly, and holoprosencephaly (HPE). Milder defects include agenesis of the corpus callosum (ACC), septo-optic dysplasia (SOD), and isolated absent cavum septi pellucidi (CSP).
Aprosencephaly and atelencephaly are two rare and very severe cerebral malformations. In aprosencephaly, neither telencephalic nor diencephalic structures develop. In atelencephaly, there remains a rudimentary prosencephalon. Craniofacial abnormalities associated with this condition are secondary to deformation brought on by the absence of the telencephalon, rather than true malformation. These disorders may result from possible autosomal recessive inheritance versus an abnormality of chromosome 13. Aprosencephaly/atelencephaly has also been reported in a family with pathogenic variants in the SIX3 gene, which has also been associated with HPE. Typically, these are diagnosed prenatally by ultrasound and fetal magnetic resonance imaging (MRI). Although considered “lethal” malformations, it is important for the neonatologist to be prepared for infants with severe malformations to live longer than expected and even go home from the hospital.
HPE represents a spectrum of defects in forebrain development and is the most common brain malformation, although most affected fetuses are miscarried early in gestation. HPE represents a variable degree of incomplete separation of the prosencephalon along one or more of its three major planes during the third and fourth weeks of gestation (discussed earlier). The DeMyer classification scheme groups the degree of separation as “alobar,” “semilobar,” and “lobar” as well as a milder middle interhemispheric variant subtype, also referred to as syntelencephaly ; however, HPE can be difficult to classify in a given patient. In alobar HPE ( Fig. 53.2 ), a single anterior ventricle is contained within a holosphere with complete lack of separation of the prosencephalon. Alobar defects may be classified by fetal imaging findings. Depending on the severity of the defect, other midline structures such as olfactory bulbs/tracts, the corpus callosum, the anterior commissure, and the optic nerves may be affected. In addition, midline deep structures such as the basal ganglia, hypothalamus, and thalamic structures are fused, and vascular malformations may also be present. The milder semilobar and lobar forms have distinct hemispheres and the presence of at least a portion of the corpus callosum. In “semilobar” HPE, the frontal lobes are more than 50% fused, and the thalami and hypothalamus may also be fused. “Lobar” HPE is associated with the fissure along almost the entire midline, separation, or near separation, of the thalami and absence of the CSP. A middle hemispheric variant has been described in which the posterior, frontal, and parietal lobes fail to separate, with an absence of the body of the corpus callosum. Typically, patients with the middle interhemispheric variant are not identified in the neonatal period unless the variant was diagnosed prenatally. Finally, a septo-preoptic type has been suggested, where the nonseparation is restricted to the septal and preoptic areas.
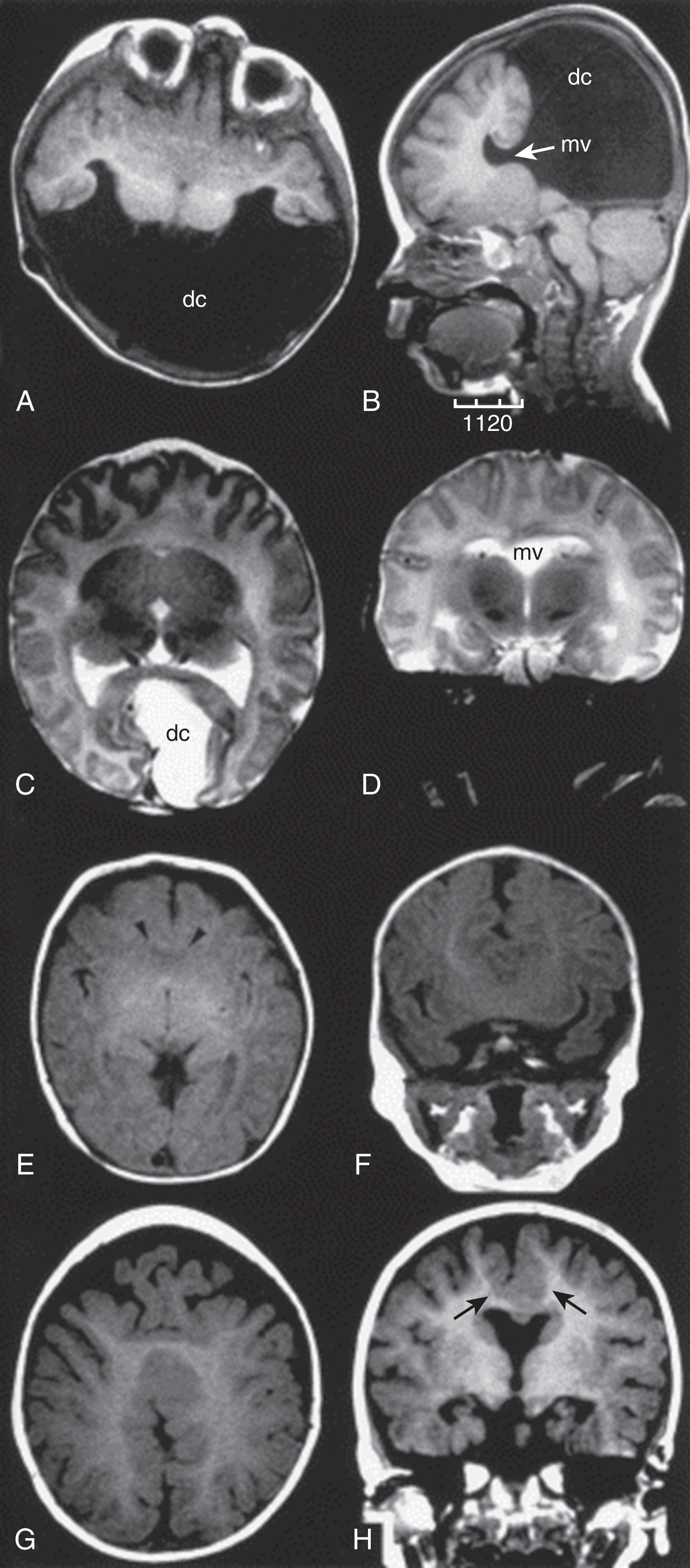
With the advent of prenatal ultrasonography, patients with HPE are usually identified before birth. Alobar HPE may be identified as early as 10 weeks’ gestation and can be reliably identified by 14 weeks. False-positive findings by ultrasonography are common, so fetal MRI can be very useful for clarifying the diagnosis and severity of the malformation, particularly if pregnancy termination is being considered. Subtle findings such as the absence of CSP may suggest the milder forms of HPE, although absent CSP can be isolated or associated with ACC. Given the high rate of chromosome abnormalities seen in HPE (25% to 50%), amniocentesis for chromosome array and possibly DNA sequencing is indicated.
Up to 80% of children with HPE have a craniofacial anomaly. The findings may range from cyclopia (a single central eye) with a nose-like structure (proboscis) above the eye, to cebocephaly (a flattened single nostril situated centrally between the eyes), to median cleft lip. Mild cases may have a single central incisor or hypotelorism. The concept of “the face predicts the brain,” refers to the fact that more severe facial malformations are often associated with more severe brain malformations; for example, patients with alobar HPE can have normal facies, while those with lobar or semilobar HPE can have severe facial malformations.
Newborns with HPE present with low tone and microcephaly. However, the microcephaly may be obscured by a co-occurring hydrocephalus due to the blockage of cerebrospinal fluid (CSF) flow through the fused thalami ; these cases are often associated with a large dorsal cyst. Ventriculoperitoneal shunts can relieve symptoms of increased intracranial pressure. Over time, patients may develop spasticity and dystonia. Oromotor dysfunction is frequent, and many children with HPE require tube feedings.
As with other midline brain defects, endocrinologic abnormalities are very common. Diabetes insipidus occurs in up to 70% of patients, with hypothyroidism, hypoadrenocorticism, and growth hormone deficiency being less common. These endocrine abnormalities can develop over time, requiring periodic monitoring. Hypothalamic dysfunction may also cause irregularities of sleep, temperature regulation, appetite, and thirst.
Approximately 40% of children with HPE have epilepsy, but one-third of these will have intractable epilepsy. Seizures may also be provoked by endocrinologic abnormalities such as hypernatremia or hypoglycemia. Given the range of possible medical issues, a multidisciplinary approach to the care of these children is necessary, including continued surveillance for future complications such as hydrocephalus, seizures, and pituitary insufficiency.
Prognosis is related to the severity of the defect, the involvement of other organ systems, and the genetic cause. Fetal or neonatal death is typical for most individuals with chromosome abnormalities. In contrast, more than 50% of cytogenetically normal patients with all types of HPE are alive at 12 months. Survival into late adolescence and adulthood has been reported.
The live birth prevalence of HPE is 1 in 10,000 to 1 in 20,000. The prevalence is higher in miscarried embryos and fetuses, representing as many as 1 per 250 pregnancies.
The cause of HPE is multifactorial, with both genetic and environmental factors appearing to contribute to the variable spectrum of presentations. Up to 45% of HPE is caused by chromosomal abnormalities detectable by standard karyotyping. The most common chromosome abnormalities are trisomies 13 and 18. Chromosome microarrays can identify smaller copy number variants in 10% to 20% of individuals with HPE with normal karyotypes. Pathogenic variants in at least 14 genes have been associated with HPE, accounting for up to 25% of syndromic forms (e.g., Smith–Lemli–Opitz, Meckel, Rubenstein–Taybi, Kallman, and Pallister–Hall syndromes). Six genes have been well established to cause nonsyndromic HPE: SHH, ZIC2, SIX3, TGIF, GLI2 , and PTCH1 . SHH accounts for up to 40% of familial cases of HPE.
HPE is characterized by extreme intrafamilial variability. The same loss-of-function pathogenic variant can be found in asymptomatic or mildly affected family members as in family members who are severely affected. Incomplete penetrance can result in “microforms,” including hypotelorism, midface hypoplasia, or a single central incisor. One explanation for these observations comes from studies suggesting that the mode of inheritance for HPE may be multigenic, though examples of digenic, “double hit,” cases are quite rare. This suggests a certain complexity to genetic modifiers of known pathogenic variants. Furthermore, the severity of expression of the HPE phenotype throughout a given family may be influenced by the additive contributions from multiple genetic factors as well as environmental or teratogenic effects.
Still, some genotype-phenotype correlations have emerged. Patients with ZIC2 pathogenic variants can have a characteristic facial appearance (bitemporal narrowing, upslanting palpebral fissures, large ears, and a short nose with anteverted nares). ZIC2 pathogenic variants also appear to be the most common de novo pathogenic variant and have a high penetrance.
Environmental factors (e.g., ethanol, vitamin A toxicity) can produce cyclopia during the early phase of gastrulation. Maternal diabetes mellitus increases the risk of HPE to approximately 1% to 2% of all pregnancies. Cholesterol-lowering agents have been associated with HPE, presumably because of their effects on SHH signaling. Smith–Lemli–Opitz syndrome is caused by a defect in the terminal step of cholesterol biosynthesis, and HPE manifests itself in approximately 5% of affected individuals. Additionally, ingested plant alkaloids have caused epidemics of cyclopia in sheep by processes that inhibit cholesterol biosynthesis. Other environmental associations (cytomegalovirus [CMV] infection, medications, assisted reproductive technologies) have been suggested by case reports or animal studies.
The corpus callosum consists of approximately 190 million axons and is formed by a complex, multistep process that involves midline patterning, cellular proliferation, migration, and axonal growth. Initial formation of the corpus callosum proceeds over 11 weeks or so and is mediated by multiple gene networks. Development continues through adolescence as these connections are refined. Genetic as well as environmental factors affect callosal formation.
ACC results in abnormal gyration of the medial portion of each hemisphere, eversion of the cingulate gyri, and sulcation perpendicular to the long axis of the hemisphere. The external angles of the lateral ventricle are oriented parallel and upward, and the fornices are widely separated. If present, a useful distinguishing feature is Probst bundles ( Fig. 53.3 ), which are fiber bundles that run parallel to the ventricle in an anterior-to-posterior direction. ACC can be partial, more often involving loss of posterior segments.
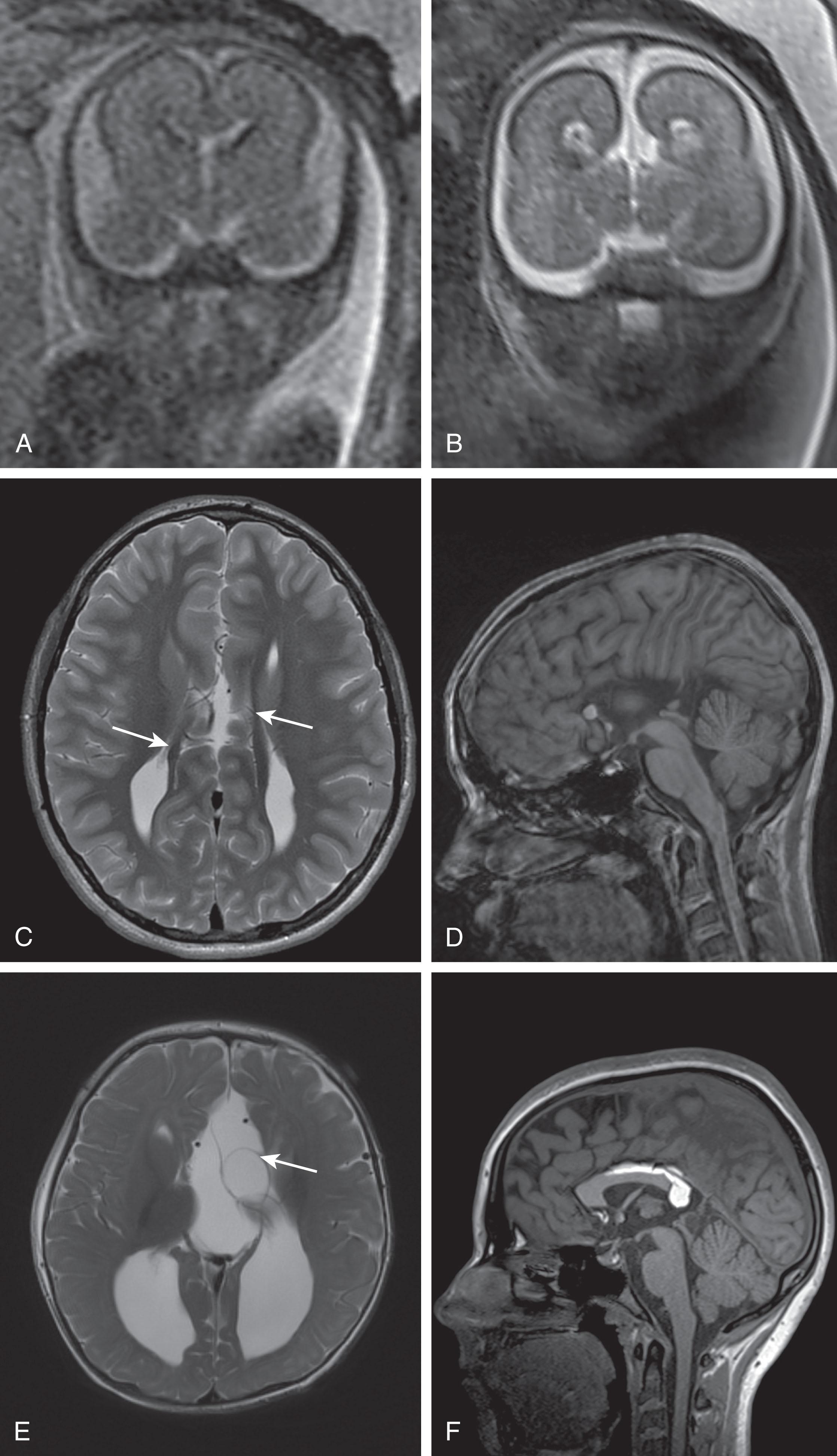
ACC often occurs in association with other structural abnormalities. These may be minor, such as cysts or lipomas (see Fig. 53.3 ), or more severe, such as heterotopia, polymicrogyria (PMG), microcephaly, abnormal sulcation, commissural and white matter abnormalities, and malformations of the posterior fossa.
The prevalence of ACC ranges from 0.5 in 10,000 in the general population to 600 in 10,000 in children with neurodevelopmental disabilities. ACC can also be associated with prenatal infections, vascular accidents, and teratogen effects. Infection results in a thinner corpus callosum with a typical rostral-to-caudal extent and is a rare cause of isolated ACC. Ethanol exposure has the strongest association with ACC, which was reported in 7% of children with fetal alcohol syndrome in one series.
ACC is a feature of hundreds of different disorders, and all modes of inheritance have been observed. Glass et al. (2008) found that callosal anomalies were associated with a chromosomal abnormality 17% of the time, commonly aneuploidy (chromosomes 13, 18, and 21). ACC may be associated with either inherited or de novo copy number variants, some overlapping with those found in patients with autism. ACC is also a primary feature of several important disorders, such as Mowat–Wilson, Aicardi, acrocallosal syndromes, L1CAM -related spastic paraplegia, and X-linked lissencephaly with ACC and ambiguous genitalia. Given the number of genetic syndromes associated with ACC, some authors have suggested a subdivision of groups based on the associated conditions (craniofacial, metabolic, ocular, ciliopathies), which aids in the diagnostic evaluation of these patients.
Prenatally, fetal MRI at 20 to 22 weeks’ gestation maximizes the identification of additional cerebral findings when pregnancy decision-making is still an option. Earlier MRI scans yield more false-negative results and miss structural changes. Additional diagnostic options include genetic (chromosomal microarray, cell-free fetal DNA) and infectious (serologic tests, polymerase chain reaction testing on amniotic fluid) disease testing. Given the challenges with accurate prenatal diagnosis, newborns should be evaluated by brain MRI shortly after birth and by subspecialty consultations (neurology, ophthalmology, genetics, developmental pediatrics, audiology). Laboratory testing (chromosome microarray, DNA sequencing, metabolic testing) should be considered, depending on the examination and MRI findings. Surveillance for neurodevelopmental issues, visual impairment, and pituitary insufficiency is recommended.
The outcomes of ACC are variable. A systematic literature review revealed that up to 75% of patients with MRI-confirmed isolated ACC were developing typically at early school age, while 11% had severe disability. Associated microcephaly, epilepsy, cerebral palsy, and cerebral dysgenesis are correlated with a higher risk of the abnormal neurodevelopmental outcome. Neuropsychological studies have shown specific impairment in abstract reasoning, problem-solving, and category fluency. Difficulty with higher-level language such as comprehension of syntax and linguistic pragmatics is also evident. These findings underscore the need for continued evaluation for learning and language difficulties in these patients.
Classic SOD is the triad of the absence of the septum pellucidum, optic nerve hypoplasia, and pituitary dysfunction. The diagnosis of SOD is made when two or more features of the triad are present ; 30% of patients have all three features. SOD is a clinically and etiologically diverse group of disorders and overlaps with isolated optic nerve hypoplasia. This diversity makes it difficult to provide counseling about prognosis and associated medical issues.
Prenatally, SOD may be suspected in fetuses with absent CSP or ACC, although most fetuses with isolated absent CSP do not have SOD, posing a challenge for counseling. Postnatally, SOD may be suspected in a patient with growth failure, visual abnormalities, or genital abnormalities secondary to pituitary dysfunction. Early diagnosis is important to reduce the risk of adrenal crisis and hypoglycemia and requires brain MRI, ophthalmologic evaluation, and laboratory testing for pituitary insufficiency.
Children with SOD may be blind or have a visual impairment, presenting with roving gaze, nystagmus, or strabismus. Neurodevelopmental prognosis is controversial and may be correlated with the presence of other brain abnormalities. In early studies, cerebral palsy was found in 57% of children with SOD, intellectual disability was found in 71%, epilepsy was found in 37%, and behavioral problems were found in 20%. A later neurodevelopmental study of seven children with unilateral or bilateral optic nerve hypoplasia with the absence of CSP found normal cognitive development, intact neurologic status, normal language development, and age-appropriate behavior in six of the seven children. Conversely, a descriptive series of three children with SOD plus cortical dysplasia showed that all three had abnormal development and neurologic examination findings. Specialists in development, neurology, endocrinology, and ophthalmology should follow these children. Hypopituitarism is seen in up to 80% of patients, with growth hormone deficiency being the most common. Lifelong monitoring is needed as pituitary insufficiency can become clinically apparent over time.
The prevalence of SOD is 1 in 10,000 births, with increased risk in younger mothers. Pathogenic variants in several genes are associated with SOD (e.g., HESX1, SOX2, SOX1, OTX2 ) ; however, a genetic origin is not identified in most patients, suggesting environmental or complex genetic causes. The disease is sporadic in most patients, and SOD can exhibit dominant and recessive modes of inheritance. Some instances of SOD have been associated with prenatal drug and alcohol exposure or a vascular pathogenesis ; however, causation remains unproven. The recurrence risk is less than 1% in the absence of consanguinity.
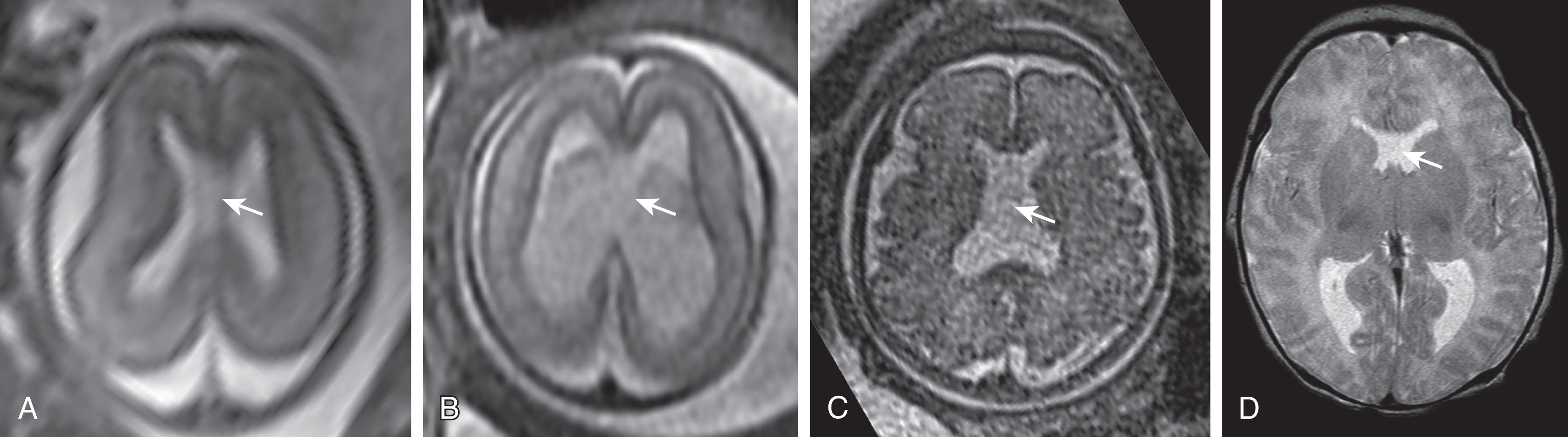
The presence of the CSP is a normal finding on ultrasonography and MRI of fetuses and premature infants. This normal finding represents a fluid-filled space between the lamellae of the septi pellucidi, which typically fuse as the fetal brain matures. The absence of the CSP in fetuses and premature infants may be associated with neuroanatomic anomalies. It may be an isolated finding ( Fig. 53.4 ), but MRI is recommended for further evaluation. In addition, a larger than expected CSP width should prompt a detailed ultrasound evaluation as this anomaly can be seen in fetuses with aneuploidy.
Defects in proliferation and neuronal survival include microcephaly and macrocephaly as well as cortical dysplasia. Migration defects result in disruption of the layered cortical structure, which can be seen grossly (as with lissencephaly) or microscopically (focal dysplasia). We will also discuss cortical defects such as heterotopia, PMG, cobblestone cortex, schizencephaly, and other destructive lesions. We will not discuss disorders of neuronal crest migration (e.g., neuroblastoma, Hirschsprung disease).
Projection neurons originate from neural progenitor cells that reside in the periventricular zone and subventricular zones. These progenitors undergo symmetric and asymmetric cell divisions to generate more progenitors as well as post-mitotic neurons, which subsequently differentiate into projection neurons. The cerebral cortex develops in an inside-out pattern, with early-born neurons forming the deepest layers and later-born neurons populating the superficial layers. This process occurs during weeks 7 to 11 of gestation. Intrinsic and extrinsic signals direct appropriate arrest of migration, positioning of the final cell layers, and terminal differentiation of projection neurons into a variety of subtypes. Disruption of any of these processes can result in the malformations we discuss. Most interneurons are born in the median ganglionic eminences and migrate long distances to populate the brain, a process termed tangential migration. Non-neuronal cells (astrocytes and oligodendrocytes) arise from the same neural progenitors that generate projection neurons, but form later.
Disorders of cortical development may be genetic or caused by in utero insults (hypoxia, ischemia, metabolic derangements, toxins, and infection). Diagnosis is based on clinical presentation, imaging, pathology, and genetic testing. Malformations can manifest clinically as epilepsy or intellectual disability and may be part of syndromic disorders with other organ involvement. Management includes both medical and surgical interventions for seizure control, therapy support for motor and cognitive disabilities, and appropriate surveillance and involvement of specialists if needed. The framework of cerebral cortex development has been used to classify cortical malformations and is being updated on the basis of expanding genetic knowledge.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here