Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Sinusitis is defined as an inflammation of the mucosal lining of the paranasal sinuses and can be caused by various factors including allergy, environmental irritants, and infection by viruses, bacteria, or fungi. It is also commonly referred to as rhinosinusitis because there is almost always coexisting inflammation in the nasal mucosa. Sinusitis can be classified as acute, subacute, and chronic. Acute sinusitis lasts up to 4 weeks and is usually caused by a viral or bacterial infection. Chronic sinusitis lasts more than 12 weeks and may result from a wide range of allergic and nonallergic causes. Subacute sinusitis lasts 4 to 12 weeks and usually represents a transition between acute and chronic sinusitis. Other patterns include recurrent acute sinusitis, defined as the occurrence of four or more episodes of acute sinusitis within 1 year, each lasting at least 7 days; and acute exacerbation of chronic sinusitis, defined as the presence of signs and symptoms of chronic sinusitis that worsen but return to baseline after treatment.
Sinusitis can also be categorized according to the mode of infection and underlying conditions, such as nosocomial sinusitis associated with nasotracheal intubation, odontogenic sinusitis, and sinusitis in severely immunocompromised hosts. From a clinical and management standpoint, the most important goal is to distinguish a bacterial infection from viral or allergic causes in acute sinusitis and to identify structural or fungal causes in chronic sinusitis. Distinguishing bacterial infection is critical for appropriate antimicrobial therapy, whereas structural or fungal causes may necessitate surgical intervention for diagnosis and treatment.
A 27-year old woman presented to the Emergency Room with a history of an acute onset of nasal discharge, a frontal headache, and a temperature of 39.5°C. Her temperature normalized within 2 days, but after 12 days she developed bothersome nasal congestion and purulent postnasal drip that did not improve. Physical examination revealed facial tenderness over the right maxillary sinus, and purulent secretion in the nasal passages and posterior pharynx. How should this patient be managed? Does she require antimicrobial therapy?
COMMENT: Several features in this patient suggest a bacterial etiology of acute sinusitis. Firstly, worsening of symptoms after initial improvement (double-sickening) is consistent with a bacterial superinfection following initial acute viral sinusitis. Secondly, purulent discharge in the nasal passages and posterior nasopharynx is highly predictive of a bacterial sinusitis. In light of her persistent symptoms, “watchful waiting” with symptomatic management is not warranted. A computed tomography (CT) of the paranasal sinusitis is recommended to confirm the diagnosis and exclude the possibility of complications. If fluid level or opacification in the sinuses is demonstrated, empirical antibiotic therapy with standard dose amoxicillin-clavulanate for 5 days is recommended. If there is no clinical improvement after 5 days, endoscopically directed middle meatal culture should be obtained for semi-quantitative culture and antibiotic susceptibility testing to confirm the diagnosis and guide further antimicrobial therapy.
The paranasal sinuses (maxillary, ethmoid, frontal, and sphenoid) are air-filled cavities lined by pseudostratified, ciliated columnar epithelium. They are interconnected through small tubular openings, the sinus ostia, which drain into different regions of the nasal cavity ( Fig. 31.1 ). The frontal, anterior ethmoid, and maxillary sinuses open into the middle meatus, whereas the posterior ethmoid and sphenoid sinuses open into the superior meatus. The osteomeatal complex, an area between the middle and inferior nasal turbinates representing the confluence of drainage from the paranasal sinuses, is a particularly important anatomic site because of its potential for mucosal thickening and impaired drainage leading to sinus infection even without mechanical obstruction of the ostia.
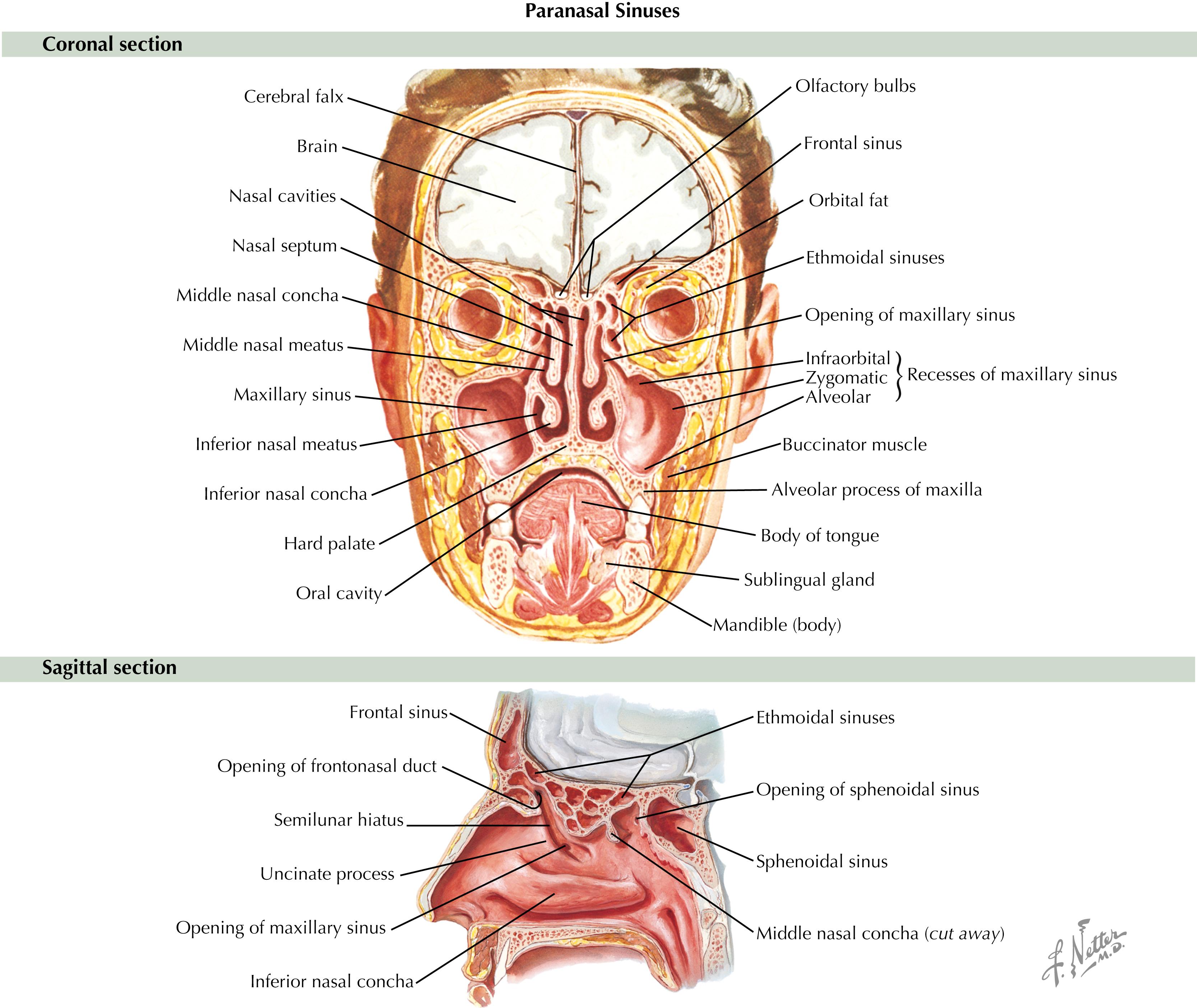
The maxillary sinuses, either alone or in combination with the ethmoid or frontal sinuses, are the most frequent site of infection. The ostium of the maxillary sinus lies at an obtuse angle toward the roof (see Fig. 31.1 ), so the maxillary sinus does not empty well in the erect posture but drains best when the patient is lying on the side opposite the affected sinus. The floor of the maxillary sinus directly adjoins the maxillary bone in which the apices of the first, second, and third molar teeth reside; hence, extraction or root infection of these teeth is a frequent cause of maxillary (odontogenic) sinusitis. Furthermore, because the superior alveolar nerves (branches of the maxillary nerve) supply both the molar teeth and the mucous membranes of the sinus, maxillary sinusitis may frequently manifest as a toothache.
The frontal sinus is not a frequent site of infection but may be a focus for spread of infection into the orbit or the brain ( Fig. 31.2 ). The frontal sinus is supplied by the supraorbital branch of the ophthalmic division of the trigeminal nerve. Thus headache is a prominent symptom of frontal sinusitis.
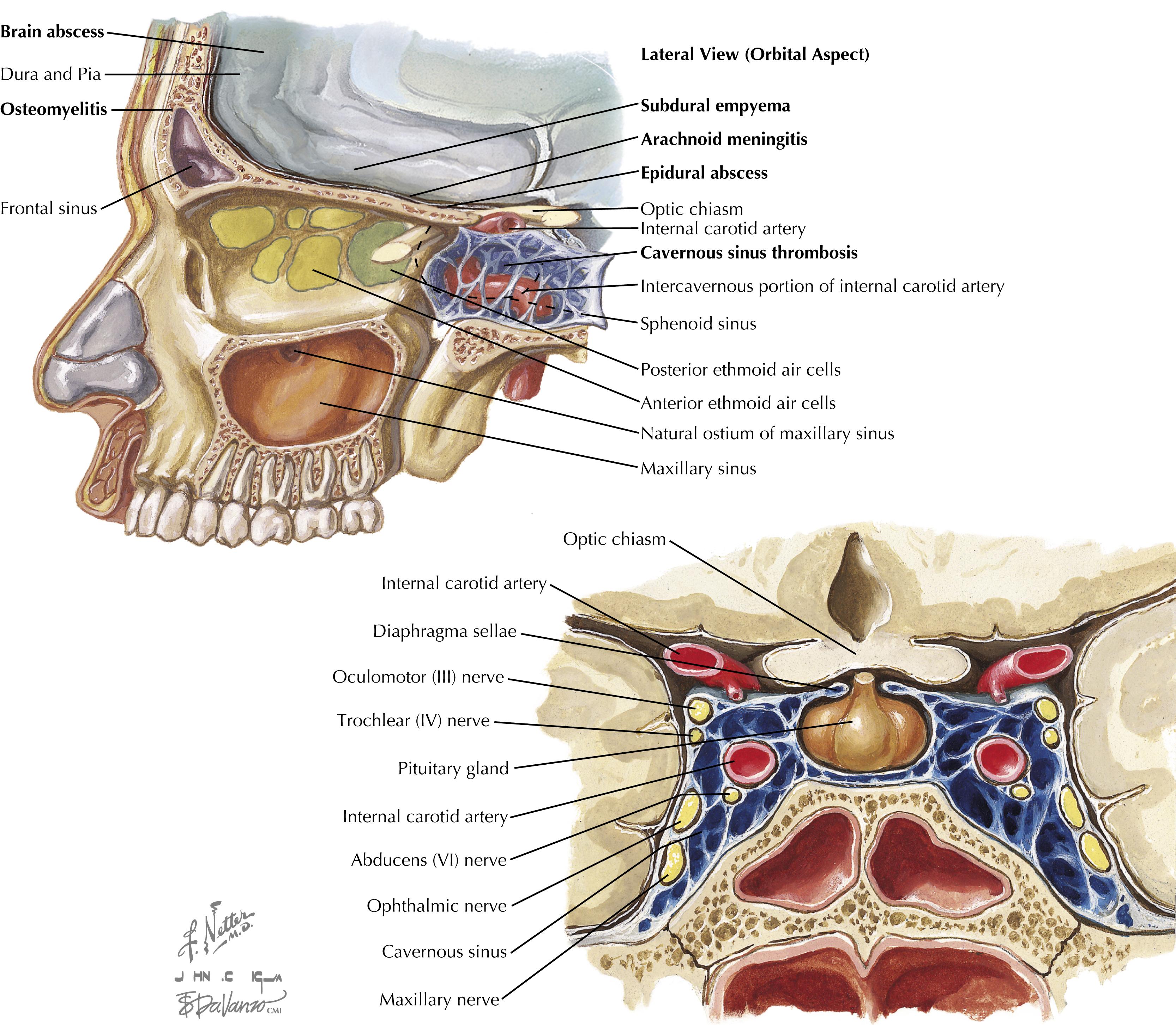
The ethmoid sinuses are composed of multiple air cells that are separated by thin bony partitions, and each air cell drains by an independent ostium. The ethmoid sinuses are separated from the orbit by a paper-thin orbital plate. Perforation of the plate allows direct spread of infection into the retro-orbital space. Ethmoid sinusitis can also spread to the superior sagittal vein or the cavernous venous sinus (see Fig. 31.2 ).
The sphenoid sinus occupies the body of the sphenoid bone in proximity to the pituitary gland above; the optic nerve and optic chiasm in front; and the internal carotids, the cavernous sinuses, and the temporal lobes of the brain on each side (see Fig. 31.2 ). Therefore sphenoid sinusitis can spread locally to cause cavernous sinus thrombosis, meningitis, temporal lobe abscess, and orbital fissure syndromes. The superior orbital fissure syndrome, characterized by orbital pain, exophthalmos, and ophthalmoplegia, is caused by involvement of the abducens, oculomotor, and trochlear nerves and the ophthalmic division of the trigeminal nerve as they pass through the orbital fissure.
A patent osteomeatal complex and normal mucociliary clearance function are the key defense mechanisms of the paranasal sinuses.
According to the 2017 National Health Interview Survey, approximately 30 million cases of sinusitis are diagnosed each year, representing 12% of all adults 18 years of age or older. Children younger than age 15 and adults 25 to 64 years old are the most frequently affected. It is the fifth leading cause for antimicrobial prescriptions in office practice. Total direct costs for treating sinusitis are estimated at $6 billion per year, not to mention significant indirect costs such as days lost from work, decreased productivity, and impaired quality of life.
Several risk factors predispose to acute or chronic sinusitis ( Box 31.1 ). The most common cause of acute sinusitis is a viral upper respiratory infection or the common cold. Adults typically develop two to three colds per year, and children have six to eight episodes per year. However, only up to 2% of adults and 6% to 13% of children with viral upper respiratory infections develop a secondary bacterial infection of the sinuses. Nose blowing that generates excessive positive intranasal pressures and propels contaminated fluid from the nasal cavity into the paranasal sinuses may be an important predisposing mechanism.
Viral upper respiratory tract infection
Allergic rhinitis
Irritants from cold or dry air
Chemicals or drugs (rhinitis medicamentosa)
Human immunodeficiency virus infection
Cystic fibrosis
Ciliary dysmotility syndrome
Viral upper respiratory tract infection
Allergic rhinitis
Anatomic abnormalities (e.g., nasal polyps, deviated nasal septum, choanal atresia, foreign body, tumors)
Common variable immunodeficiency
Selective immunoglobulin deficiency (immunoglobulin A [IgA], IgG subclasses)
Acquired immunodeficiency syndrome
Wegener granulomatosis
Diabetes mellitus
Odontogenic infection
Nasotracheal or nasogastric intubation
Head trauma
Swimming or diving
Cocaine sniffing
A strong association exists among allergic rhinitis, asthma, and recurrent sinusitis in both children and adults. It has been suggested that allergic rhinitis may be a predisposing factor for acute maxillary sinusitis in 25% to 30% of patients, and as many as 60% to 80% of patients with chronic sinusitis. The observation that asthma, allergic rhinitis, and rhinosinusitis frequently coexist raises the possibility that these conditions are manifestations of an inflammatory process within an integrated and contiguous upper and lower airway (the integrated airway hypothesis).
Mild and selective immune deficiencies have been frequently demonstrated in children and adults with recurrent or persistent symptoms of sinus disease. One study found that 52% of patients had selective immunoglobulin (Ig) deficiencies (IgG2, IgG4 subclass, or IgA) or poor responsiveness to some polysaccharide antigens. In addition, chronic or recurrent sinusitis is an important source of morbidity in patients with cystic fibrosis and patients infected with human immunodeficiency virus (HIV).
Certain actions, such as sustaining head trauma, swimming, diving, cocaine sniffing, and nasotracheal or nasogastric intubation, may repeatedly traumatize the nasal mucosa and facilitate microbial invasion of the paranasal sinuses. Dental extraction and periapical infections of the maxillary molar teeth are particularly important causes of odontogenic sinusitis.
Sinus puncture and aspiration is the gold standard for establishing the microbial cause of sinusitis. Although acute sinusitis is primarily caused by respiratory viruses such as rhinoviruses, influenza A, parainfluenza, respiratory syncytial virus, and adenoviruses, direct isolation of these viruses from antral aspirates has been relatively uncommon. In acute bacterial sinusitis, Streptococcus pneumoniae and nonencapsulated Haemophilus influenzae are the causative agents in 70% of adults, whereas the addition of Moraxella catarrhalis accounts for 80% of cases in children ( Table 31.1 ). Staphylococcus aureus together with viridans streptococci and S. pneumoniae are the predominant isolates in acute sphenoid sinusitis. Anaerobes are uncommonly isolated in acute sinusitis but are the predominant flora in chronic sinusitis. The isolation of anaerobes during acute sinusitis suggests an odontogenic source. Nosocomial sinusitis secondary to prolonged nasotracheal intubation is commonly a polymicrobial infection caused by gram-negative bacteria, S. aureus, and anaerobes.
| Microbial Agent | Prevalence Mean (Range) | |
|---|---|---|
| Adults (%) | Children (%) | |
| Acute Sinusitis | ||
| Streptococcus pneumoniae | 20–43 | 36–37 |
| Haemophilus influenzae | 6–35 | 23–25 |
| Moraxella catarrhalis | 2–10 | 19–25 |
| Streptococcus pyogenes | 1–7 | 2 |
| Staphylococcus aureus | 0–8 | 8–10 |
| Gram-negative bacilli (includes Enterobacteriaceae species, Pseudomonas aeruginosa ) | 0–24 | 2 |
| Anaerobes (Bacteroides, Fusobacterium, Peptostreptococcus, Veillonella) | 0–12 | 0–4 |
| Respiratory viruses (rhinovirus, influenza, parainfluenza, adenovirus) | 3–15 | 0–2 |
| Chronic Sinusitis | ||
| Aerobes | 29–43 | 20 |
| Streptococcus species | 9–14 | 6 |
| Staphylococcus species | 5–14 | 6 |
| Haemophilus influenzae | 1–6 | 3–5 |
| Anaerobes | 57–88 | 80 |
| Peptostreptococcus species | 25–38 | 23–73 |
| Bacteroides species | 14–27 | 27–29 |
| Fusobacterium species | 3–4 | 5–16 |
Up to 40% of H. influenzae , 80% of M. catarrhalis , and 30% of respiratory tract anaerobes produce β-lactamase. Over 25% of S. pneumoniae is now resistant to trimethoprim-sulfamethoxazole (TMP-SMX). Macrolide-resistant H. influenzae and S. pneumoniae are also isolated with increasing frequency.
The microbiology of chronic sinusitis is more closely linked to underlying comorbid diseases and differs considerably from that of acute sinusitis. In patients with cystic fibrosis, Pseudomonas aeruginosa and nontypable H. influenzae are the most frequent pathogens. Sinusitis in patients with HIV infection is often caused by gram-negative bacilli and unusual pathogens such as Aspergillus species and cytomegalovirus. In debilitated and severely immunocompromised hosts, such as those with uncontrolled diabetes mellitus, advanced HIV infection, or chemotherapy-induced neutropenia, invasive fungal infection with Aspergillus, Mucor, Pseudallescheria boydii, Fusarium, and other saprophytic fungi may occur. In chronic sinusitis associated with nasal polyposis or allergic fungal rhinosinusitis, hypersensitivity to and colonization by Aspergillus and other saprophytic fungi in the paranasal sinuses can often be demonstrated. In addition, there is an increased prevalence of nasal colonization by enterotoxin-producing S. aureus in patients with chronic sinusitis associated with nasal polyposis. Such patients typically demonstrate local production of enterotoxin-specific IgE antibodies and coexisting aspirin sensitivity or asthma.
Acute sinusitis is often difficult to distinguish from the common cold or allergic (vasomotor) rhinitis. The presence of at least two major symptoms or one major and two or more minor symptoms may distinguish acute sinusitis (whether viral or bacterial) from rhinitis ( Table 31.2 ). Three hallmarks that suggest a bacterial sinusitis rather than a viral infection are: (1) persistence (i.e., more than 10 days); (2) severity; and (3) worsening of respiratory symptoms after initial improvement (double-sickening). The probability of identifying a bacterial infection by sinus aspiration is approximately 60% for patients with symptoms persisting beyond 10 days. The presence of purulent postnasal discharge, maxillary toothache, facial pain, or unilateral maxillary sinus tenderness further increases the likelihood of a bacterial infection. Hyposmia, jaw pain with mastication, nasal congestion, and a recent history of upper respiratory tract infection are other manifestations. The combination of these clinical findings greatly enhances the diagnostic probability. In children, the most common manifestations of bacterial sinusitis are cough (80%), nasal discharge (76%), and fever (63%). Parents of preschoolers often report malodorous breath. Headache, facial pain, and swelling are rare.
| Major Symptoms | Minor Symptoms |
|---|---|
| Purulent anterior nasal discharge Purulent or discolored posterior nasal discharge Nasal congestion or obstruction Facial congestion or fullness Facial pain or pressure Hyposmia or anosmia Fever (for acute sinusitis only) |
Headache Ear pain, pressure, or fullness Halitosis Dental pain Cough Fever (for subacute or chronic sinusitis) Fatigue |
a A diagnosis of sinusitis is probable in the presence of at least two major symptoms or one major and two or more minor symptoms.
In ethmoid sinusitis, edema of the eyelids and excessive tearing may be a prominent feature. Retro-orbital pain and proptosis indicate extension of infection into the orbit. Severe intractable headache is dominant in sphenoid sinusitis and can mimic ophthalmic migraine or trigeminal neuralgia. Neurologic deficit with hypoesthesia or hyperesthesia of the ophthalmic or maxillary dermatomes of the trigeminal nerve may be detected in one third of the patients.
In nosocomial sinusitis secondary to prolonged nasotracheal or nasogastric intubation, the clinical features may be relatively silent apart from unexplained fever. The presence of purulent rhinorrhea or a middle ear effusion may be the only physical finding. A high index of suspicion is required for early diagnosis.
Chronic sinusitis may mimic asthma, allergic rhinitis, or chronic bronchitis. Pain or tenderness on palpation may be present over the affected sinuses. Fever is uncommon. Physical findings may be subtle. Fatigue, general malaise, and an ill-defined feeling of unwellness and irritability can be more prominent than local symptoms of nasal congestion, facial pain, or postnasal drip. Four cardinal findings in chronic sinusitis include: (1) anterior and/or posterior mucopurulent drainage; (2) nasal obstruction; (3) facial pain, pressure, or fullness; and (4) decreased sense of smell (hyposmia or anosmia). The presence of at least two of these signs or symptoms together with objective signs of mucosal inflammation is required to make a firm diagnosis. In addition, chronic sinusitis may manifest in three distinctive clinical syndromes: (1) chronic sinusitis with nasal polyposis (20% to 33% of cases); (2) allergic fungal rhinosinusitis (6% to 12%); and (3) chronic sinusitis without nasal polyposis (60% to 65%).
Chronic sinusitis without nasal polyposis typically shows abundant eosinophils and neutrophils but lacks evidence of fungal hyphae. Chronic sinusitis with polyposis is clinically more distinctive because of the presence of bilateral nasal polyps with eosinophilic infiltration in the middle meatus or the sinus cavities. There is a high association with aspirin sensitivity and asthma, and colonization with enterotoxin-producing S. aureus with evidence of IgE-mediated hypersensitivity to these superantigens. Allergic fungal sinusitis is characterized by abundant “allergic mucin” associated with sinus opacification, the presence of degranulating eosinophils, and fungal hyphae. IgE-mediated hypersensitivity to one or more colonizing fungi can usually be demonstrated.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here