Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A valuable characteristic of the vascular system is that all blood vessels are distensible. The distensible nature of the arteries allows them to accommodate the pulsatile output of the heart and to average out the pressure pulsations. This capability provides smooth continuous flow of blood through the very small blood vessels of the tissues.
The most distensible of all the vessels are the veins. Even slight increases in venous pressure cause the veins to store 0.5 to 1.0 liter of extra blood. Therefore, the veins provide a reservoir for storing large quantities of extra blood that can be called into use whenever blood is required elsewhere in the circulation.
Vascular distensibility normally is expressed as the fractional increase in volume for each millimeter of mercury rise in pressure, in accordance with the following formula:
That is, if 1 mm Hg causes a vessel that originally contained 10 ml of blood to increase its volume by 1 ml, the distensibility would be 0.1 per mm Hg, or 10% per mm Hg.
The walls of the arteries are thicker and far stronger than those of the veins. Consequently, the veins, on average, are about eight times more distensible than the arteries. That is, a given increase in pressure causes about eight times as much increase in blood in a vein as in an artery of comparable size.
In the pulmonary circulation, the pulmonary vein distensibilities are similar to those of the systemic circulation. However, the pulmonary arteries normally operate under pressures about one sixth of those in the systemic arterial system, and their distensibilities are correspondingly greater—about six times the distensibility of systemic arteries.
In hemodynamic studies, it usually is much more important to know the total quantity of blood that can be stored in a given portion of the circulation for each mm Hg pressure rise than to know the distensibilities of the individual vessels. This value is called the compliance or capacitance of the respective vascular bed; that is:
Compliance and distensibility are quite different. A highly distensible vessel that has a small volume may have far less compliance than a much less distensible vessel that has a large volume because compliance is equal to distensibility times volume.
The compliance of a systemic vein is about 24 times that of its corresponding artery because it is about 8 times as distensible and has a volume about 3 times as great (8 × 3 = 24).
A convenient method for expressing the relationship of pressure to volume in a vessel or in any portion of the circulation is to use a volume-pressure curve. The red and blue solid curves in Figure 15-1 represent, respectively, the volume-pressure curves of the normal systemic arterial system and venous system, showing that when the arterial system of the average adult person (including all the large arteries, small arteries, and arterioles) is filled with about 700 ml of blood, the mean arterial pressure is 100 mm Hg but, when it is filled with only 400 ml of blood, the pressure falls to zero.
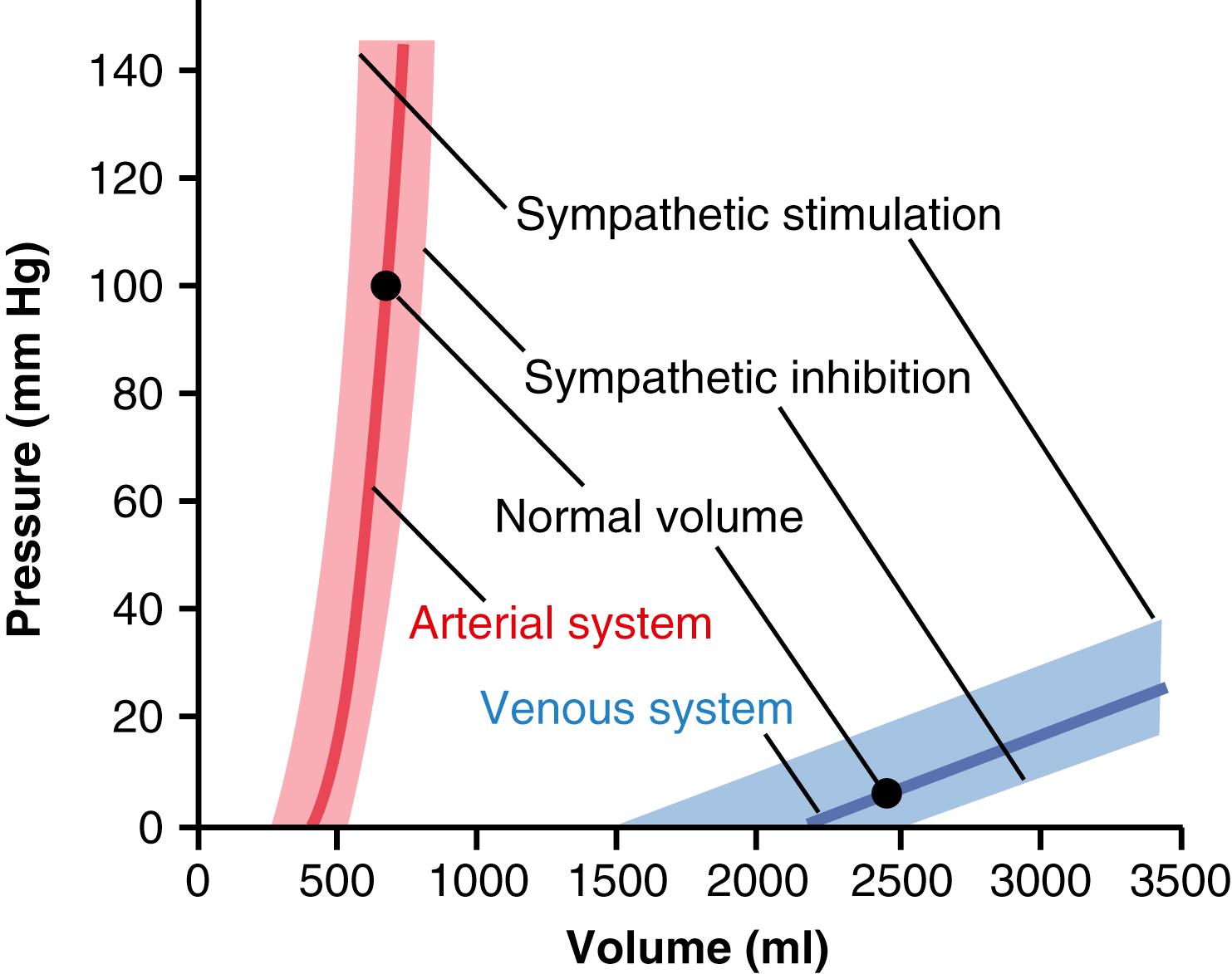
In the entire systemic venous system, the volume normally ranges from 2000 to 3500 ml, and a change of several hundred ml in this volume is required to change the venous pressure by only 3 to 5 mm Hg. This requirement mainly explains why as much as one-half liter of blood can be transfused into a healthy person in only a few minutes without greatly altering the function of the circulation.
Also shown in Figure 15-1 are the effects on the volume-pressure curves when the vascular sympathetic nerves are excited or inhibited. It is evident that an increase in vascular smooth muscle tone caused by sympathetic stimulation increases the pressure at each volume of the arteries or veins, whereas sympathetic inhibition decreases the pressure at each volume. Control of the vessels by the sympathetics in this manner is a valuable means for diminishing the dimensions of one segment of the circulation, thus transferring blood to other segments. For example, an increase in vascular tone throughout the systemic circulation can cause large volumes of blood to shift into the heart, which is one of the principal methods that the body uses to rapidly increase heart pumping.
Sympathetic control of vascular capacitance is also highly important during hemorrhage. Enhancement of sympathetic tone, especially to the veins, reduces the vessel sizes enough that the circulation continues to operate almost normally, even when as much as 25% of the total blood volume has been lost.
The term delayed compliance means that a vessel exposed to increased volume at first exhibits a large increase in pressure, but progressive delayed stretching of smooth muscle in the vessel wall allows the pressure to return toward normal over a period of minutes to hours. This effect is shown in Figure 15-2 . In this figure, the pressure is recorded in a small segment of a vein that is occluded at both ends. An extra volume of blood is suddenly injected until the pressure rises from 5 to 12 mm Hg. Even though none of the blood is removed after it is injected, the pressure begins to decrease immediately and approaches about 9 mm Hg after several minutes. Thus, the volume of blood injected causes immediate elastic distention of the vein, but then the smooth muscle fibers of the vein begin to creep to longer lengths, and their tensions correspondingly decrease. This effect is a characteristic of all smooth muscle and is called stress-relaxation, as explained in Chapter 8 .
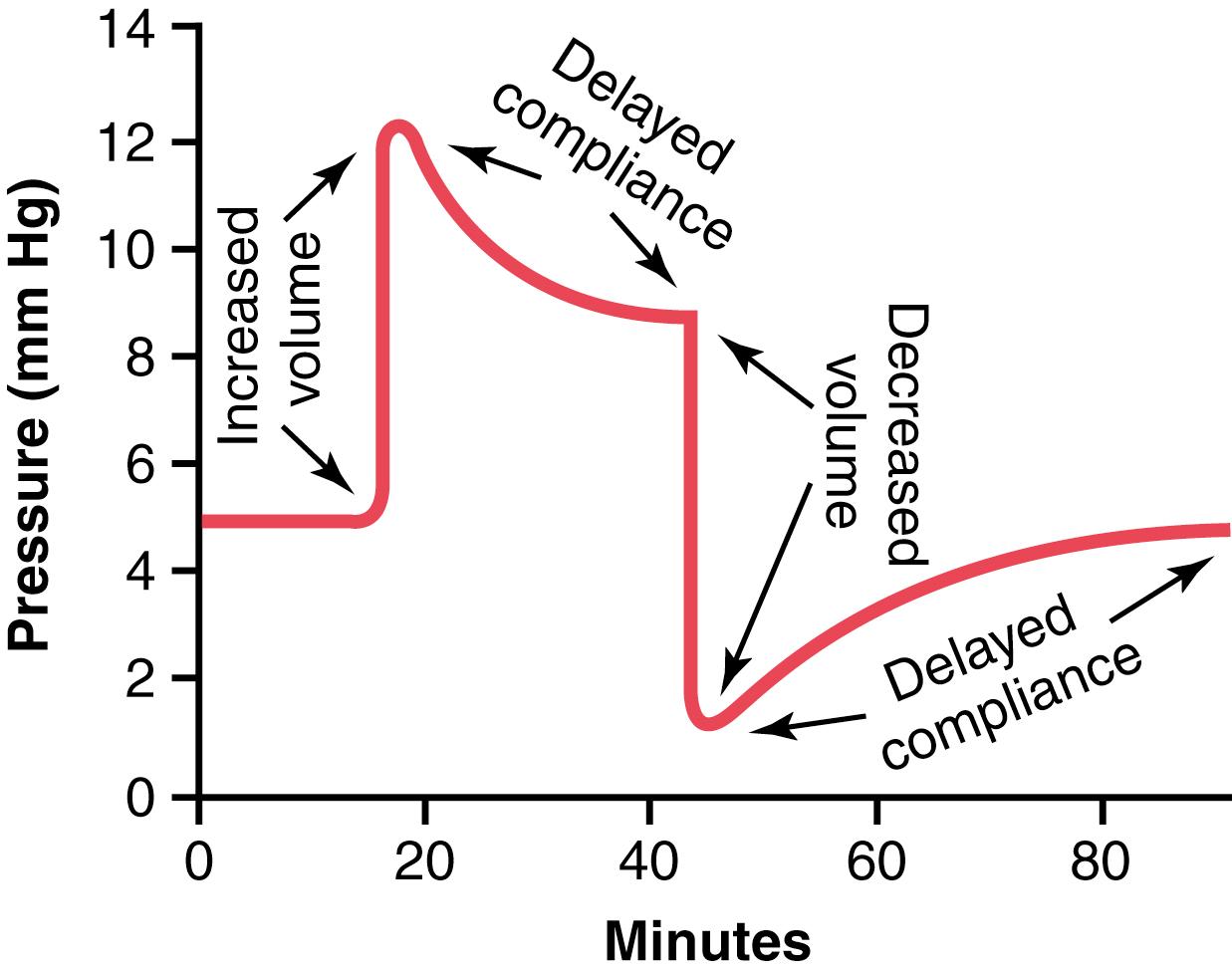
Delayed compliance is a valuable mechanism whereby the circulation can accommodate extra blood when necessary, such as after a large transfusion. Delayed compliance in the reverse direction is one way in which the circulation automatically adjusts itself over a period of minutes or hours to diminished blood volume after serious hemorrhage.
With each beat of the heart, a new surge of blood fills the arteries. Were it not for distensibility of the arterial system, all this new blood would have to flow through the peripheral blood vessels almost instantaneously, only during cardiac systole, and no flow would occur during diastole. However, the compliance of the arterial tree normally reduces the pressure pulsations to almost no pulsations by the time the blood reaches the capillaries; therefore, tissue blood flow is mainly continuous with very little pulsation.
The pressure pulsations at the root of the aorta are illustrated in Figure 15-3 . In a healthy young adult, the pressure at the top of each pulse, called the systolic pressure, is about 120 mm Hg. At the lowest point of each pulse, called the diastolic pressure, it is about 80 mm Hg. The difference between these two pressures, about 40 mm Hg, is called the pulse pressure.
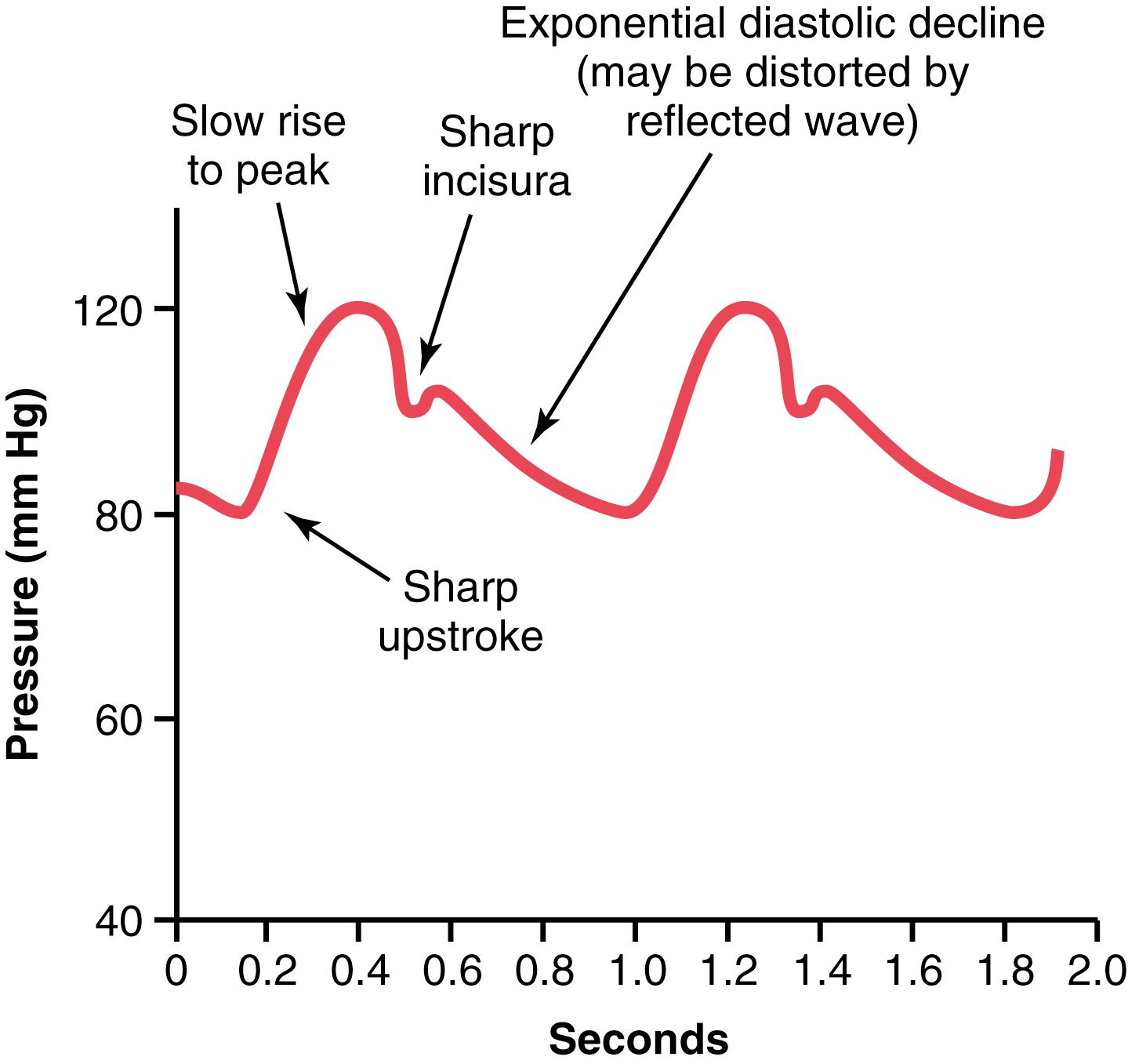
Two major factors affect the pulse pressure: (1) the stroke volume output of the heart; and (2) the compliance (total distensibility) of the arterial tree. A third less important factor is the character of ejection from the heart during systole.
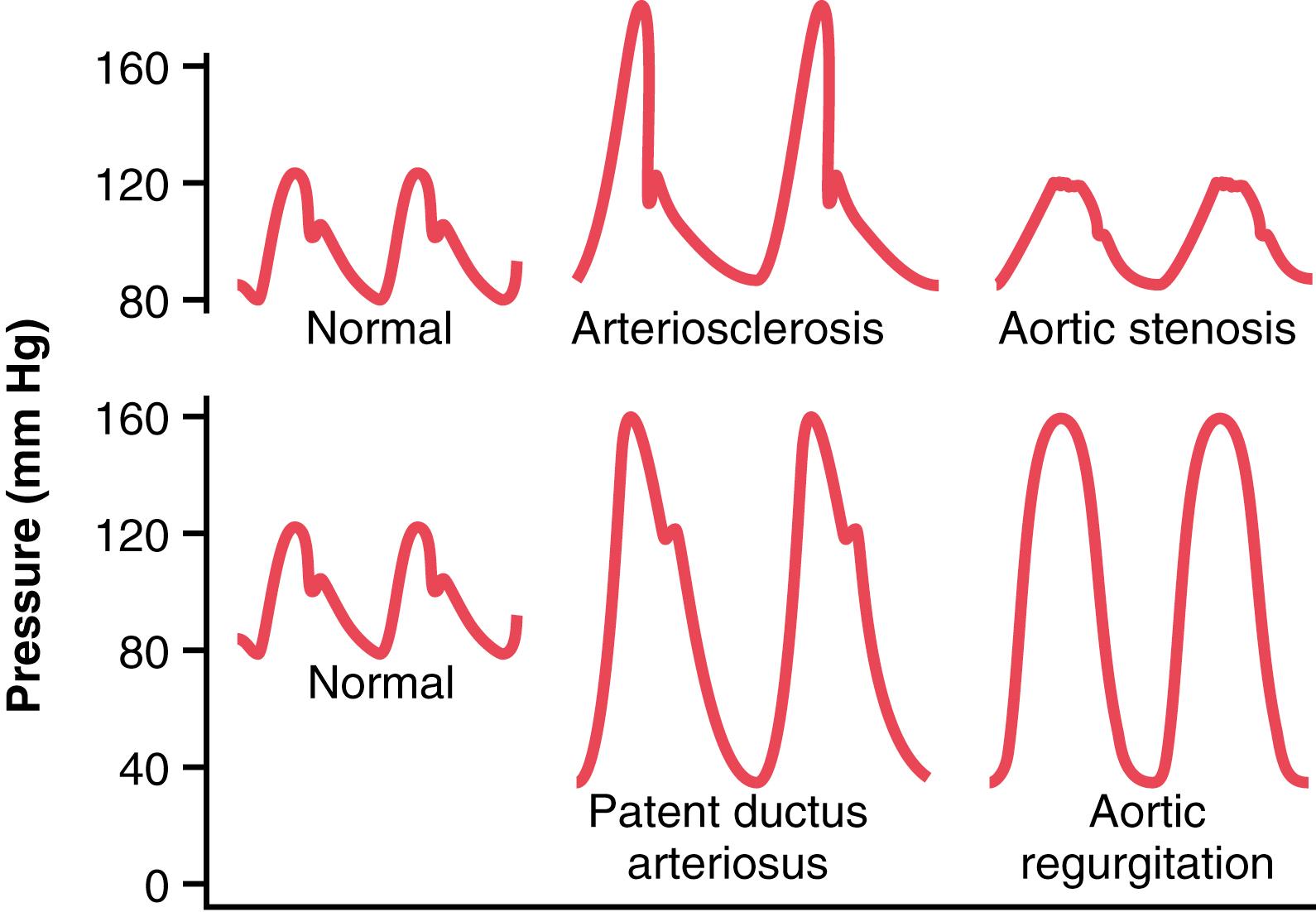
In general, the greater the stroke volume output, the greater the amount of blood that must be accommodated in the arterial tree with each heartbeat and, therefore, the greater the pressure rise and fall during systole and diastole, thus causing a greater pulse pressure. Conversely, the less the compliance of the arterial system, the greater the rise in pressure for a given stroke volume of blood pumped into the arteries. For example, as demonstrated by the middle top curves in Figure 15-4 , the pulse pressure in old age sometimes rises to twice normal because the arteries have stiffened with arteriosclerosis and therefore are relatively noncompliant.
In effect, pulse pressure is determined approximately by the ratio of stroke volume output to compliance of the arterial tree . Any condition of the circulation that affects either of these two factors also affects the pulse pressure:

Some pathophysiological conditions of the circulation cause abnormal contours of the pressure pulse wave in addition to altering the pulse pressure. Especially distinctive among these conditions are aortic stenosis, patent ductus arteriosus, and aortic regurgitation, each of which is shown in Figure 15-4 .
In persons with aortic valve stenosis , the diameter of the aortic valve opening is reduced significantly, and the aortic pressure pulse is decreased significantly because of diminished blood flow outward through the stenotic valve.
In persons with patent ductus arteriosus, 50% or more of the blood pumped into the aorta by the left ventricle flows immediately backward through the wide open ductus into the pulmonary artery and lung blood vessels, thus allowing the diastolic pressure to fall very low before the next heartbeat and increasing the pulse pressure.
In persons with aortic regurgitation, the aortic valve is absent or does not close completely. Therefore, after each heartbeat, the blood that has just been pumped into the aorta flows immediately backward into the left ventricle. As a result, the aortic pressure can fall all the way to zero between heartbeats. Also, there is no incisura in the aortic pulse contour because there is no aortic valve to close.
When the heart ejects blood into the aorta during systole, only the proximal portion of the aorta initially becomes distended because the inertia of the blood prevents sudden blood movement all the way to the periphery. However, the rising pressure in the proximal aorta rapidly overcomes this inertia, and the wavefront of distention spreads farther and farther along the aorta, as shown in Figure 15-5 . This phenomenon is called transmission of the pressure pulse in the arteries.
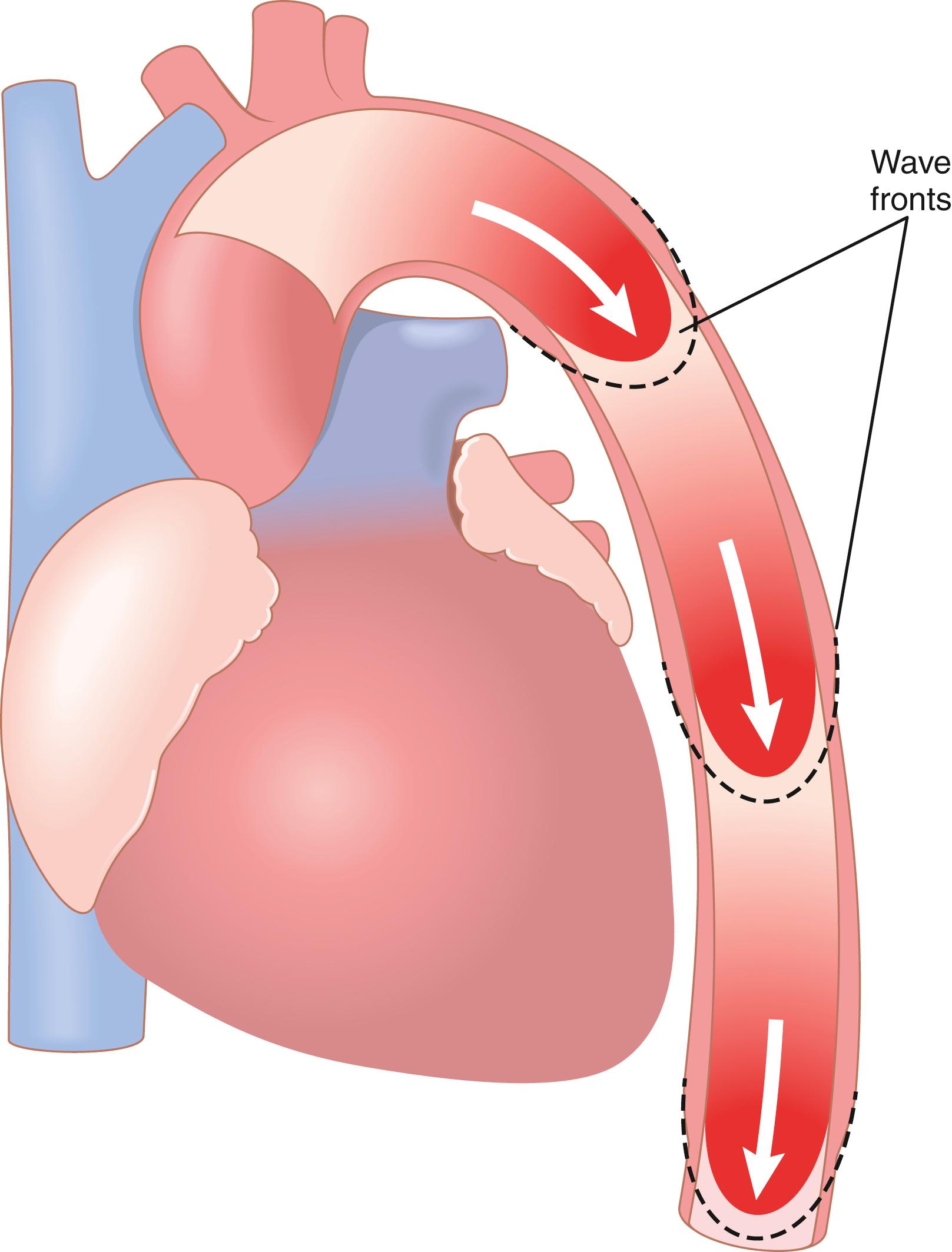
The velocity of pressure pulse transmission is 3 to 5 m/sec in the normal aorta, 7 to 10 m/sec in the large arterial branches, and 15 to 35 m/sec in the small arteries. In general, the greater the compliance of each vascular segment, the slower the velocity, which explains the slow transmission in the aorta and the much faster transmission in the much less compliant small distal arteries. In the aorta, the velocity of transmission of the pressure pulse is 15 or more times the velocity of blood flow because the pressure pulse is simply a moving wave of pressure that involves little forward total movement of blood volume.
Figure 15-6 shows typical changes in the pressure pulse contours as the pulse travels into the peripheral vessels. Note especially in the three lower curves that the intensity of pulsation becomes progressively less in the smaller arteries, arterioles and, especially, capillaries. In fact, only when the aortic pulsations are extremely large or the arterioles are greatly dilated can pulsations be observed in the capillaries.
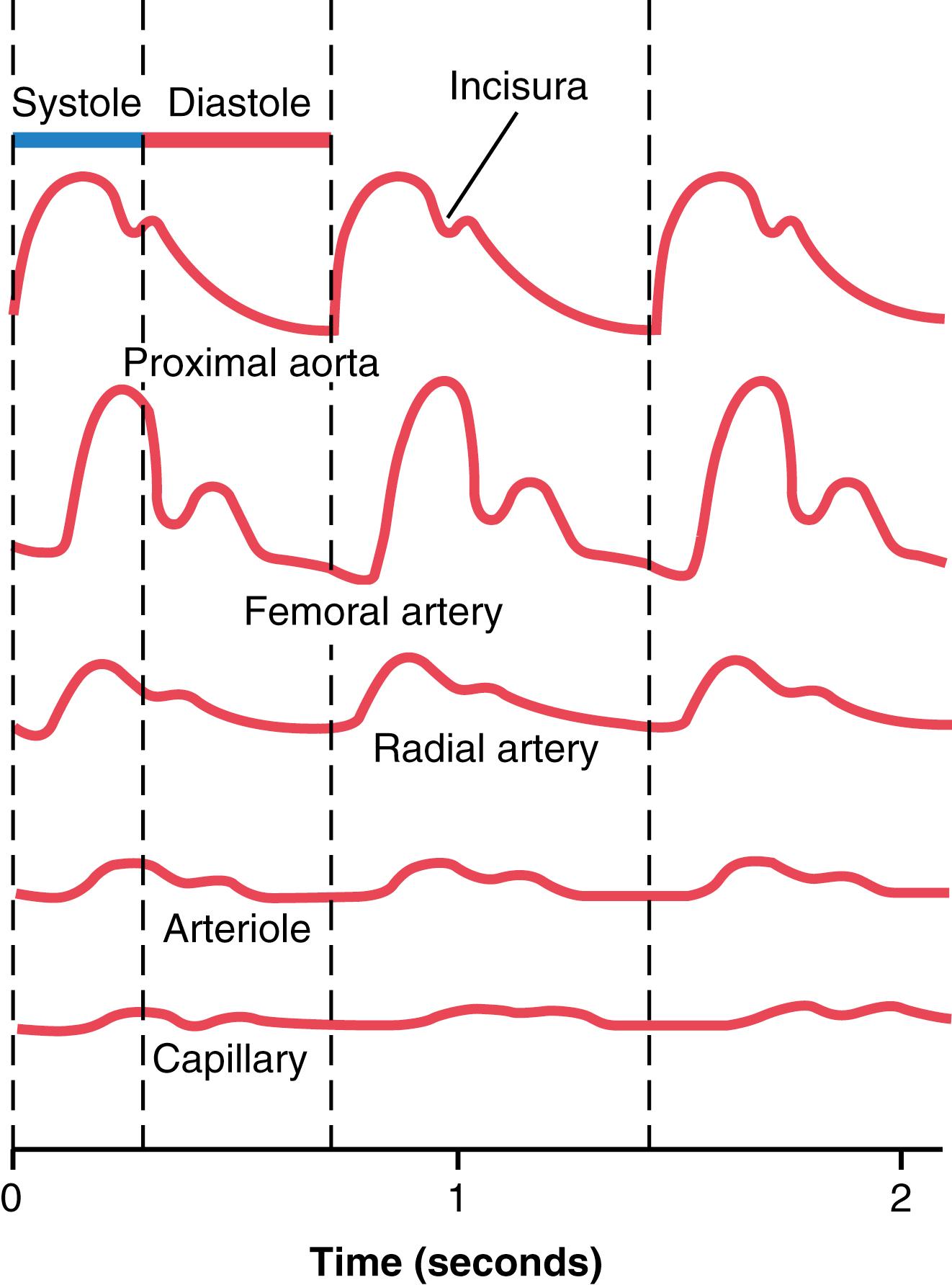
This progressive diminution of the pulsations in the periphery is called damping of the pressure pulses. The cause of this damping is twofold: (1) resistance to blood movement in the vessels; and (2) compliance of the vessels. The resistance damps the pulsations because a small amount of blood must flow forward at the pulse wave front to distend the next segment of the vessel; the greater the resistance, the more difficult it is for this to occur. The compliance damps the pulsations because the more compliant a vessel, the greater the quantity of blood required at the pulse wave front to cause an increase in pressure. Therefore, the degree of damping is almost directly proportional to the product of resistance times compliance .
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here