Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The Conformable TAG (CTAG) endoprosthesis (WL Gore and Associates, Flagstaff, Arizona) is the third-generation thoracic endograft approved for treatment of aneurysm, traumatic transection, and Type B dissection in the descending thoracic aorta. The second-generation TAG endoprosthesis was the first stent graft approved for thoracic endovascular aortic repair (TEVAR) of descending aortic aneurysm by the US Food and Drug Administration (FDA) in 2005. More than 40,000 TAG devices were distributed worldwide prior to its discontinuation in 2013. These devices have been studied extensively in various clinical trials and real-world use clinical series and are associated with significantly lower short-term mortality and morbidity than open surgery for thoracic aortic aneurysm. The efficacy of the newer CTAG device has been further studied for the treatment of Type B aortic dissection and traumatic aortic transection.
The expansion of the use of the TAG and CTAG devices in treating thoracic pathologies have led to a unique set of device-related complications, which will be summarized in this chapter. The complications can be divided into intraoperative (maldeployment, retrograde dissection, branch occlusion), early events, and late events (stent graft collapse, stent fracture).
The TAG thoracic endoprosthesis is a self-expanding device comprising of an expanded polytetrafluoroethylene (ePTFE) and fluoroethylpropylene (FEP) tube graft, which is supported externally by a nitinol stent. There are flared covered scallops and a radiopaque gold marker at each end of the device ( Fig. 20.1 ). An ePTFE sleeve is used to constrain the stent graft on the delivery catheter and remains in place between the external surface of the device and the aorta after deployment. The TAG endoprosthesis was available in sizes ranging from 26 to 45 mm for use in intended aortic inner diameters of 23–42 mm, with the recommended oversizing window of 8%–17%.

The phase II pivotal study was a prospective, nonrandomized, multicenter study, which enrolled 142 patients who underwent TEVAR of descending thoracic aortic aneurysms with the first generation TAG device. The enrollment was between 1999 and 2001 and a total of 139 patients (98%) underwent successful implantation of the device. Three patients had procedural failure (2%) resulting from access issues secondary to iliac artery size and tortuosity. Two patients had misplacement of the device, resulting in unplanned coverage of subclavian and/or visceral arteries. The patient with coverage of visceral vessels underwent open removal of the displaced device. Major adverse events (MAE) within 30-days occurred in 32% of patients, including bleeding (9%), cardiac event (3%), pulmonary event (10%), and vascular complications (14%). The overall operative mortality was 2% and five patients (3.5%) suffered a perioperative stroke. Four patients developed spinal cord ischemia and the subsequent placement of spinal drain was beneficial in three out of those four patients. Five patients developed early endoleak, including one Type I and four Type II endoleaks. The patient who had early Type I endoleak was treated with placement of an additional proximal endograft.
The all-cause mortality and aneurysm-related mortality for the pivotal trial was 75% and 79% respectively at 2 years. There were three proximal migrations and four component migrations during 2-year follow-up. Three patients underwent endovascular interventions and one had conversion to open surgery. No aneurysm rupture was reported during the follow-up. The cumulative rate of endoleak was 15% (21 patients) during the first 2 years after surgery. There were 20 stent fractures, which were identified in 19 patients. Up to 90% of the stent fractures occurred in the longitudinal spine and two in the apical nitinol support ring. The majority of patients with stent fracture in this cohort were asymptomatic (18 patients) and only one patient developed a Type III endoleak, which was treated successfully with extension of the pre-existing stent graft.
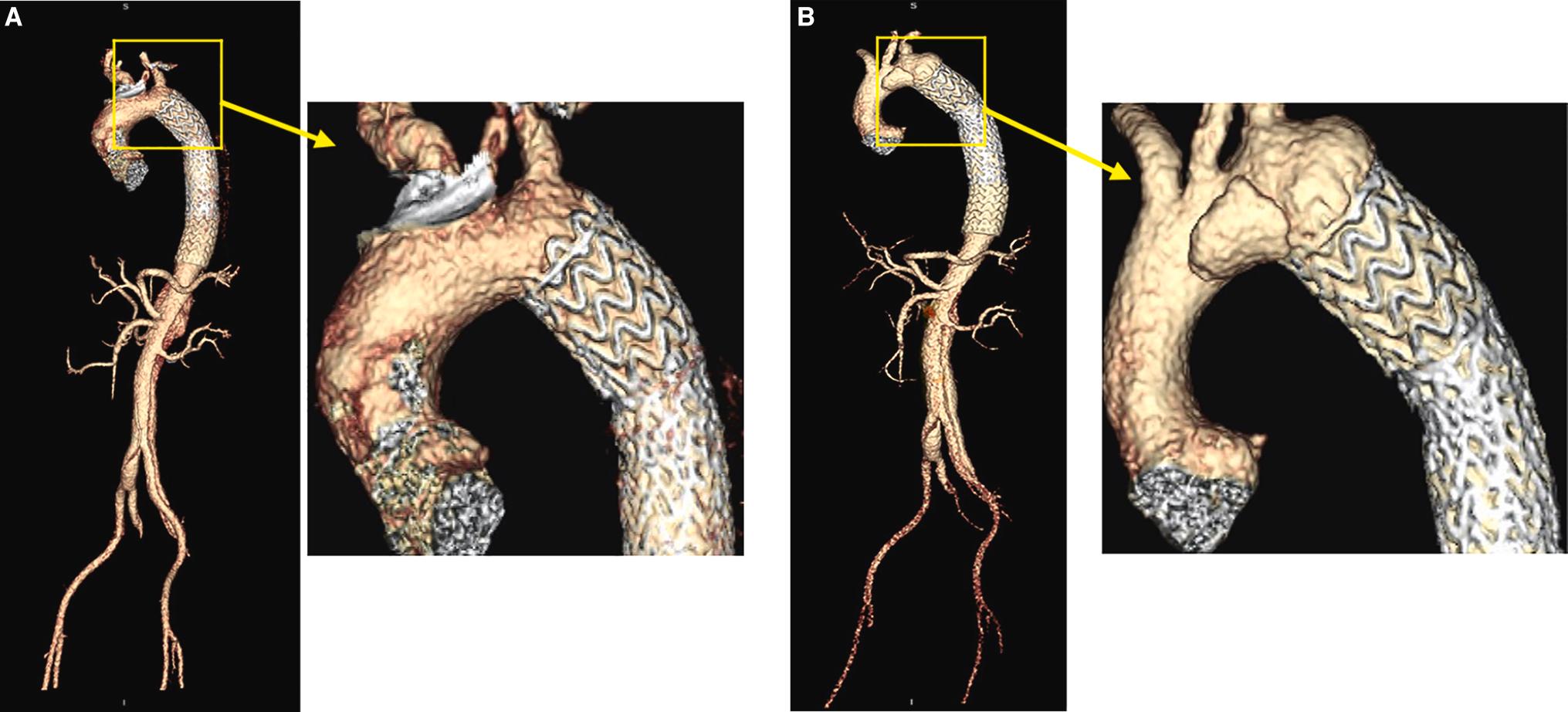
The complication of stent fractures in the initial pivotal trial led to voluntary withdrawal of the device in May 2001 and the development of the second generation TAG device. The first generation TAG device was constructed with two ePTFE layers and was supported by two longitudinal columnar spines ( Fig. 20.1A ). The modified second generation TAG device was constructed with three ePTFE layers and the longitudinal wires, which were susceptible to fracture, were removed ( Fig. 20.1B ). The modified device was evaluated in the confirmatory trial, which enrolled 51 patients from 11 clinical sites. The MAE was 12% at 30-day follow-up and there was no device-related MAE reported.
The intermediate and long-term results for the TAG pivotal trial were published in 2007 and 2008. The rate of aneurysm-related mortality was significantly lower in the TAG group when compared with the open surgical group (2.8% versus 11.7%, P =0.008). Endoleaks developed in 10.6% of TAG patients and the majority were Type Ia endoleak at the attachment site. Five TAG patients required aneurysm-related endovascular and open reinterventions (3.6%): one arch aneurysm repair for Type I endoleak and migration, five endovascular interventions in three patients for endoleaks, and one open conversion for aortoesophageal fistula. There were no additional spine fractures other than the previously reported 20 fractures (19 patients) after 24 months.
Structurally the TAG device was not as flexible as the newer generation CTAG device (described later). In patients with deep arch curves or so-called gothic arches, suboptimal placement resulted in a “bird-beak” appearance as a result of incomplete inner aortic curve apposition to the aortic arch ( Fig. 20.2 ). This theoretically increased the risk of Type Ia endoleak and/or endograft collapse. The less flexible TAG endograft was also found in other off-label use to cause new antegrade intimal tears when it was used to treat aortic dissection ( Fig. 20.3 ). In our practice we recommend the placement of an extension endograft to correct the “bird beak” to eliminate the pressure onto the membrane of dissection. This type of graft-related complications have fortunately been minimized with the more flexible new generation CTAG endoprosthesis ( Fig. 20.4 ).


Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here