Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The study of anatomy requires a clinical vocabulary that defines position, movements, relationships, and planes of reference, as well as the systems of the human body. The study of anatomy can be by body region or by body organ systems . Generally, courses of anatomy in the United States approach anatomical study by regions, integrating all applicable body systems into the study of a particular region. This textbook therefore is arranged regionally, and for those studying anatomy for the first time, this initial chapter introduces you to the major body systems that you will encounter in your study of anatomy. You will find it extremely helpful to refer back to this introduction as you encounter various body systems in your study of regional anatomy.
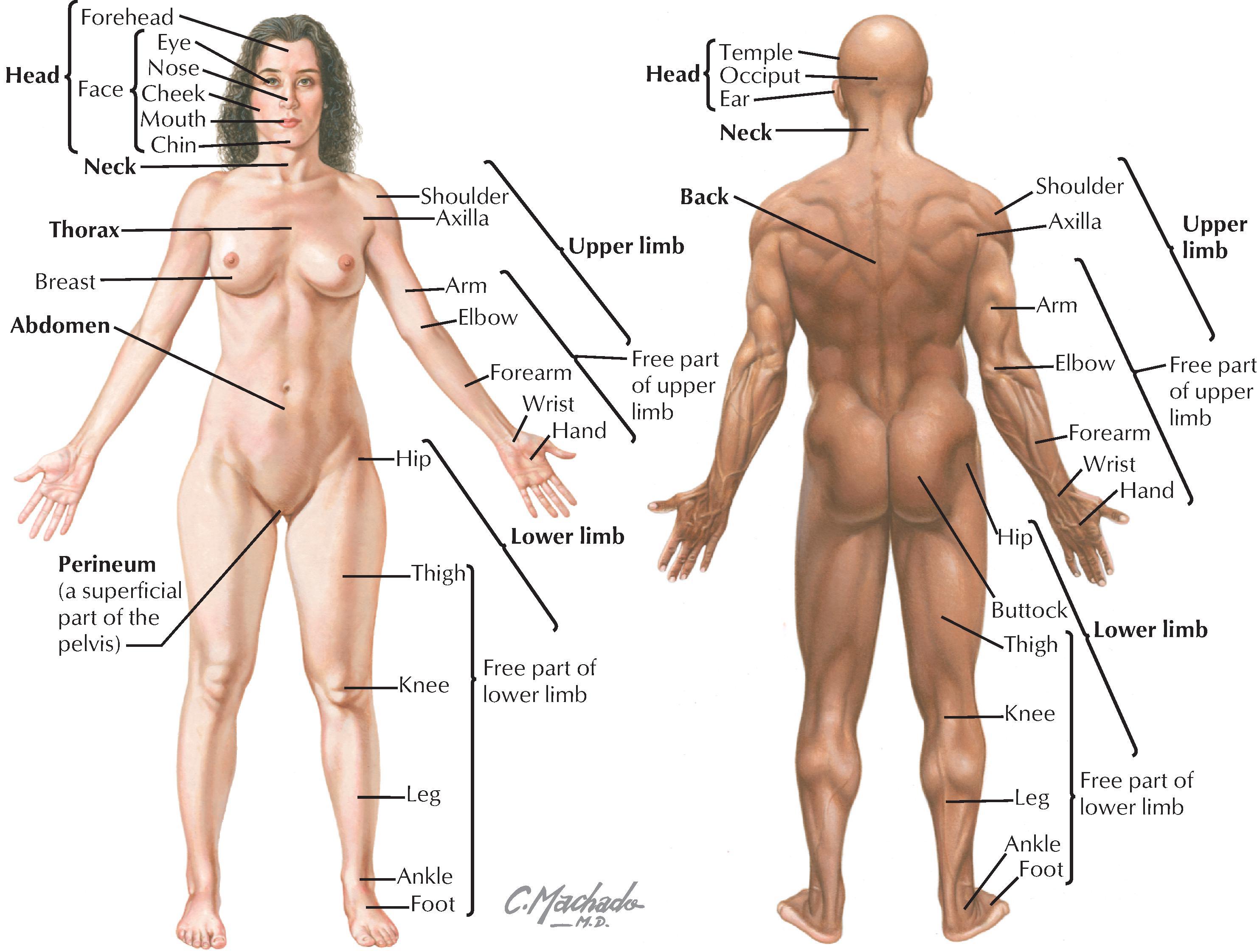
By convention, anatomical descriptions of the human body are based on a person in the anatomical position ( Fig. 1.1 ), as follows:
Standing erect and facing forward
Arms hanging at the sides with palms facing forward
Legs placed together with feet facing forward
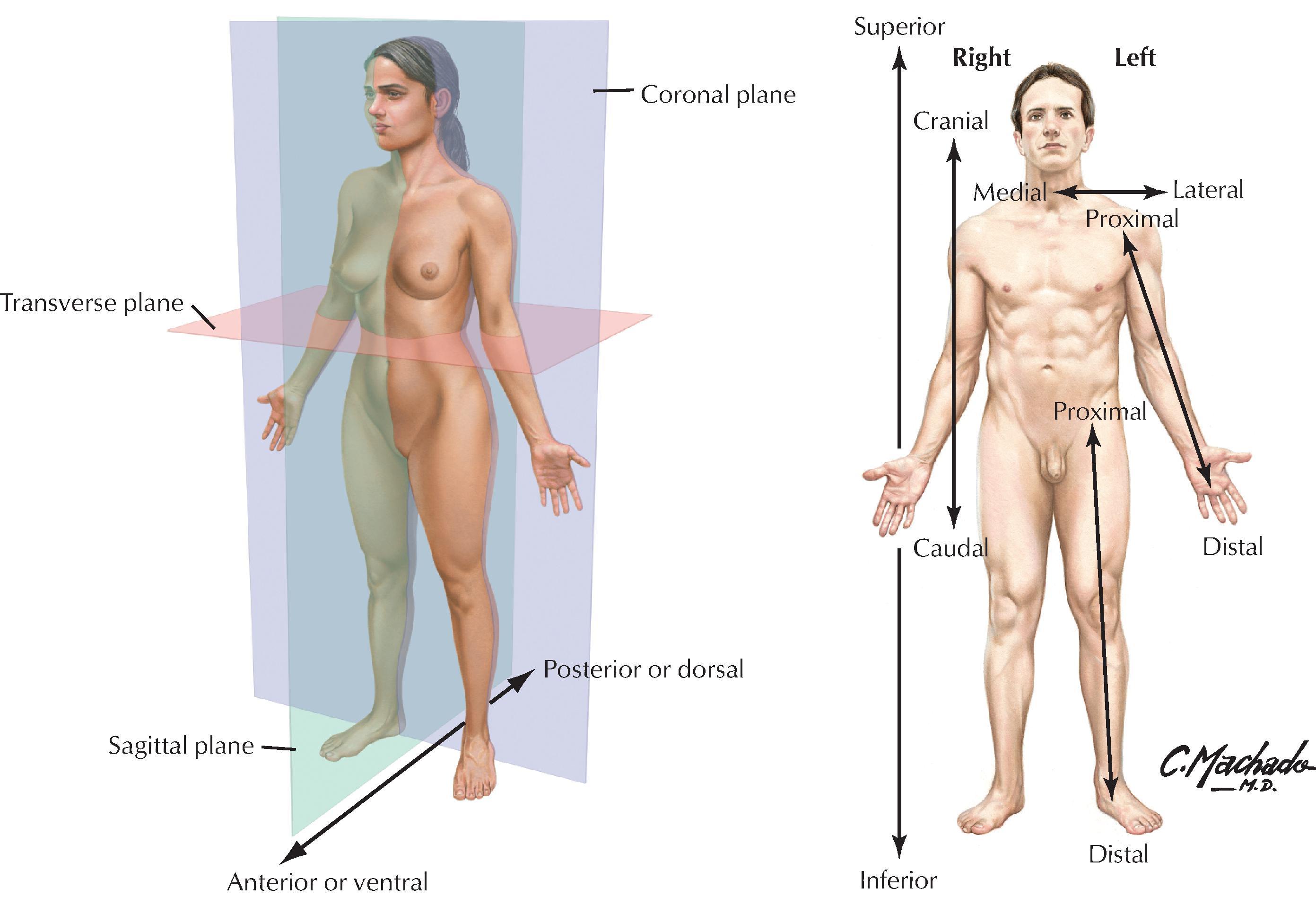
Anatomical descriptions often are referenced to one or more of three distinct body planes ( Fig. 1.2 and Table 1.1 ), as follows:
Sagittal plane: a vertical plane that divides the body into equal right and left halves (median or midsagittal plane) or a plane parallel to the median sagittal plane (parasagittal) that divides the body into unequal right and left portions.
Frontal (coronal) plane: a vertical plane that divides the body into anterior and posterior portions (equal or unequal); this plane is at right angles to the median sagittal plane.
Transverse (axial) plane: a horizontal plane that divides the body into superior and inferior portions (equal or unequal) and is at right angles to both the median sagittal and the frontal planes (sometimes called cross sections ).
| TERM | DEFINITION |
|---|---|
| Anterior (ventral) | Near the front |
| Posterior (dorsal) | Near the back |
| Superior (cranial) | Upward, or near the head |
| Inferior (caudal) | Downward, or near the feet |
| Medial | Toward the midline or median plane |
| Lateral | Farther from the midline or median plane |
| Proximal | Near a reference point |
| Distal | Away from a reference point |
| Superficial | Closer to the surface |
| Deep | Farther from the surface |
| Median plane | Divides body into equal right and left parts |
| Midsagittal plane | Median plane |
| Sagittal plane | Divides body into unequal right and left parts |
| Frontal (coronal) plane | Divides body into equal or unequal anterior and posterior parts |
| Transverse plane | Divides body into equal or unequal superior and inferior parts (cross sections) |
Key terms of relationship used in anatomy and the clinic are summarized in Table 1.1 . A structure or feature closer to the front of the body is considered anterior (ventral), and one closer to the back is termed posterior (dorsal). The terms medial and lateral are used to distinguish a structure or feature in relationship to the midline; the nose is medial to the ear, and in anatomical position, the nose also is anterior to the ear. Sometimes these terms of relationship are used in combination (e.g., superomedial, meaning closer to the head and nearer the median sagittal plane).
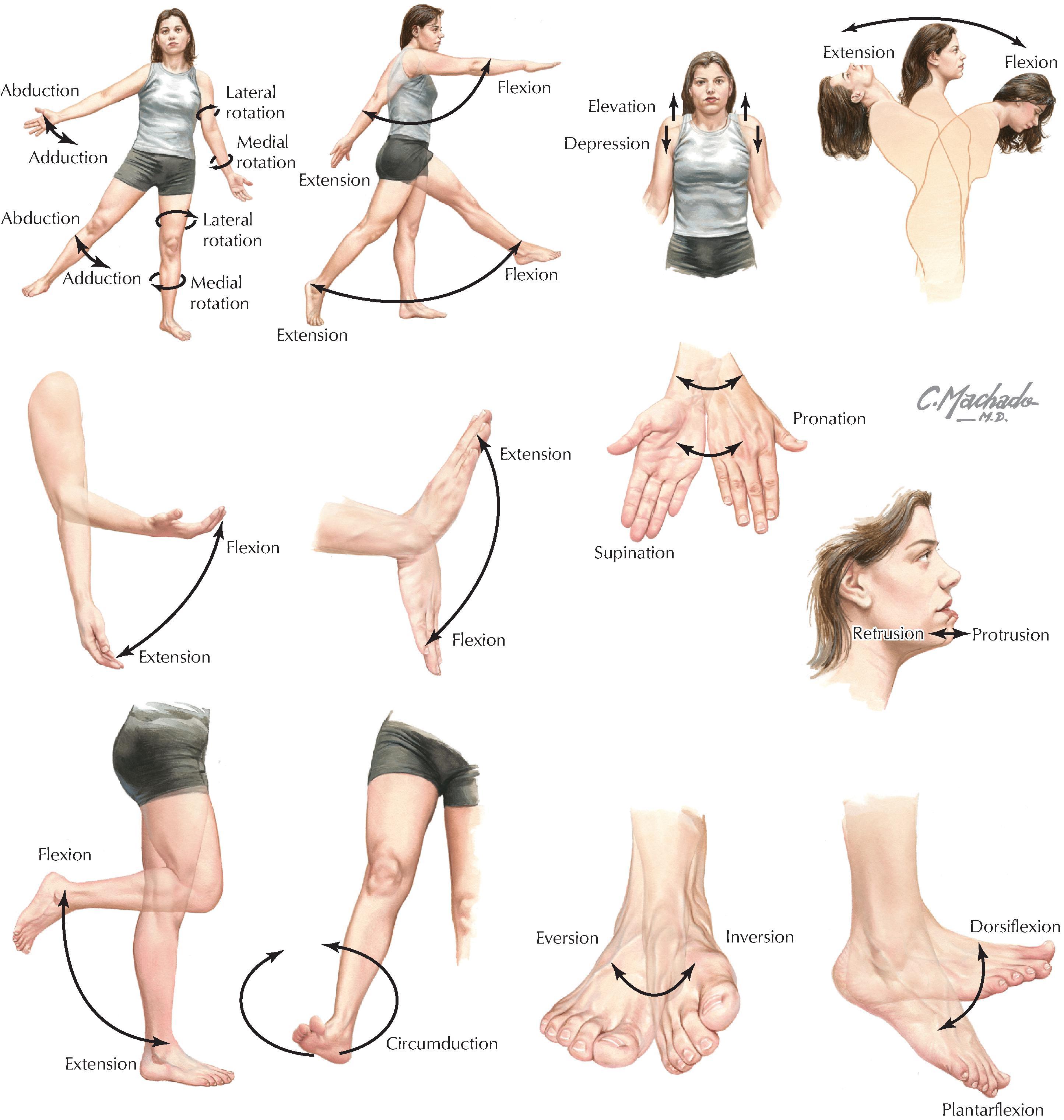
Body movements usually occur at the joints where two or more bones or cartilages articulate with one another. Muscles act on joints to accomplish these movements and may be described as follows: “The biceps muscle flexes the forearm at the elbow.” Fig. 1.3 summarizes the terms of movement.
The human body is remarkably complex and remarkably consistent anatomically, but normal variations do exist, often related to size, gender, age, number, shape, and attachment. Variations are particularly common in the following structures:
Bones: the fine features of bones (processes, spines, articular surfaces) may be variable depending on the forces working on a bone.
Muscles: they vary with size and fine details of their attachments (it is better to learn their actions and general attachments rather than focus on detailed exceptions).
Organs: the size and shape of some organs will vary depending on their normal physiology or pathophysiologic changes that have occurred previously.
Arteries: they are surprisingly consistent, although some variation is seen in the branching patterns, especially in the lower neck (subclavian branches) and in the pelvis (internal iliac branches).
Veins: they are consistent, although variations, especially in size and number of veins, can occur and often can be traced to their complex embryologic development; veins generally are more numerous than arteries, larger, and more variable.
The skin is the largest organ in the body, accounting for about 15% to 20% of the total body mass, and has the following functions:
Protection: against mechanical abrasion and in immune responses, as well as prevention of dehydration.
Temperature regulation: largely through vasodilation, vasoconstriction, fat storage, or activation of sweat glands.
Sensations: to touch by specialized mechanoreceptors such as pacinian and Meissner’s corpuscles; to pain by nociceptors; and to temperature by thermoreceptors.
Endocrine regulation: by secretion of hormones, cytokines, and growth factors, and by synthesis and storage of vitamin D.
Exocrine secretions: by secretion of sweat and oily sebum from sebaceous glands.
The skin consists of two layers ( Fig. 1.4 ):
Epidermis: is the outer protective layer consisting of a keratinized stratified squamous epithelium derived from the embryonic ectoderm.
Dermis: is the dense connective tissue layer that gives skin most of its thickness and support, and is derived from the embryonic mesoderm.
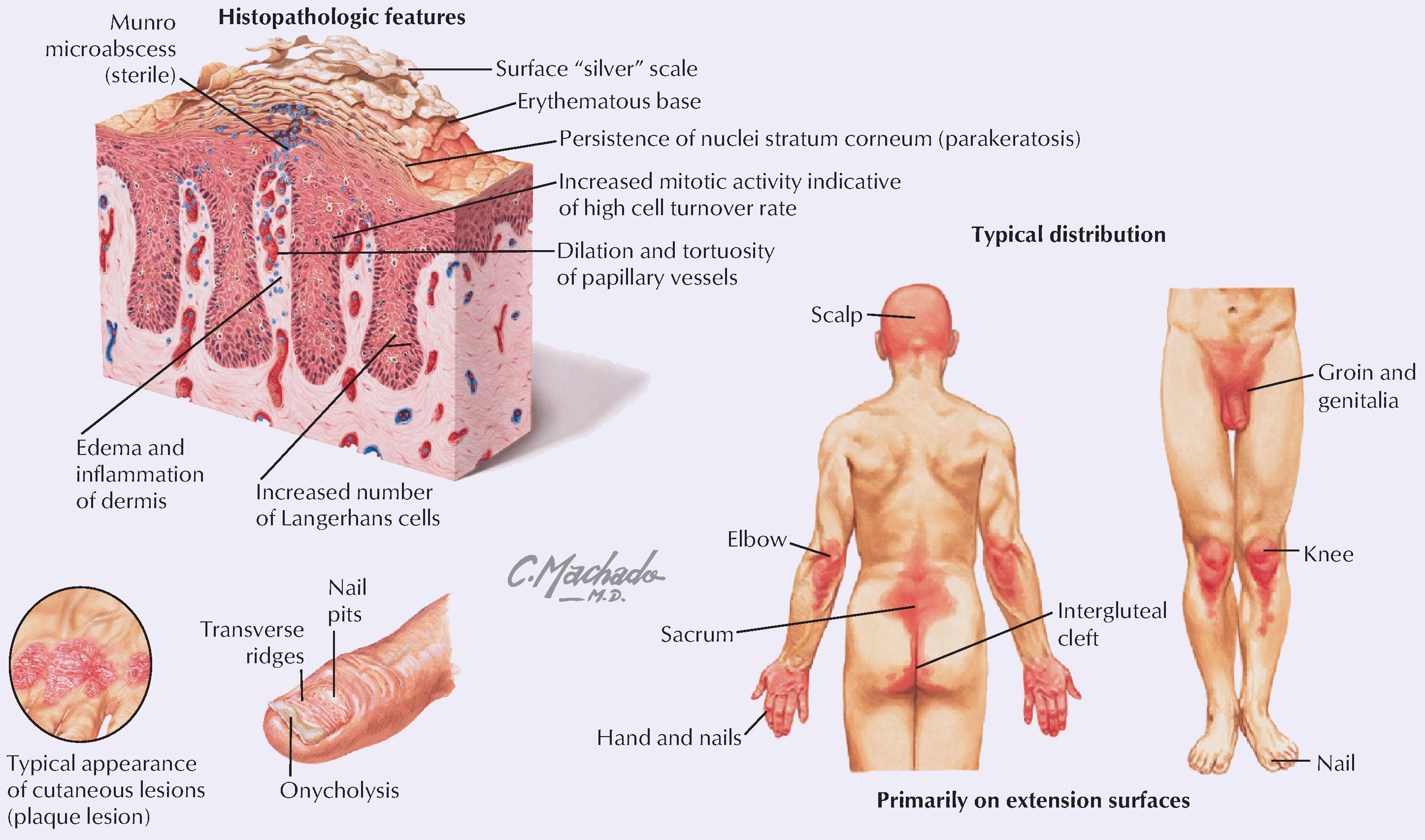
Psoriasis is a chronic inflammatory skin disorder that affects approximately 1% to 3% of the population (women and men equally). It is characterized by defined red plaques capped with a surface scale of desquamated epidermis. Although the pathogenesis is unknown, psoriasis seems to involve a genetic predisposition.
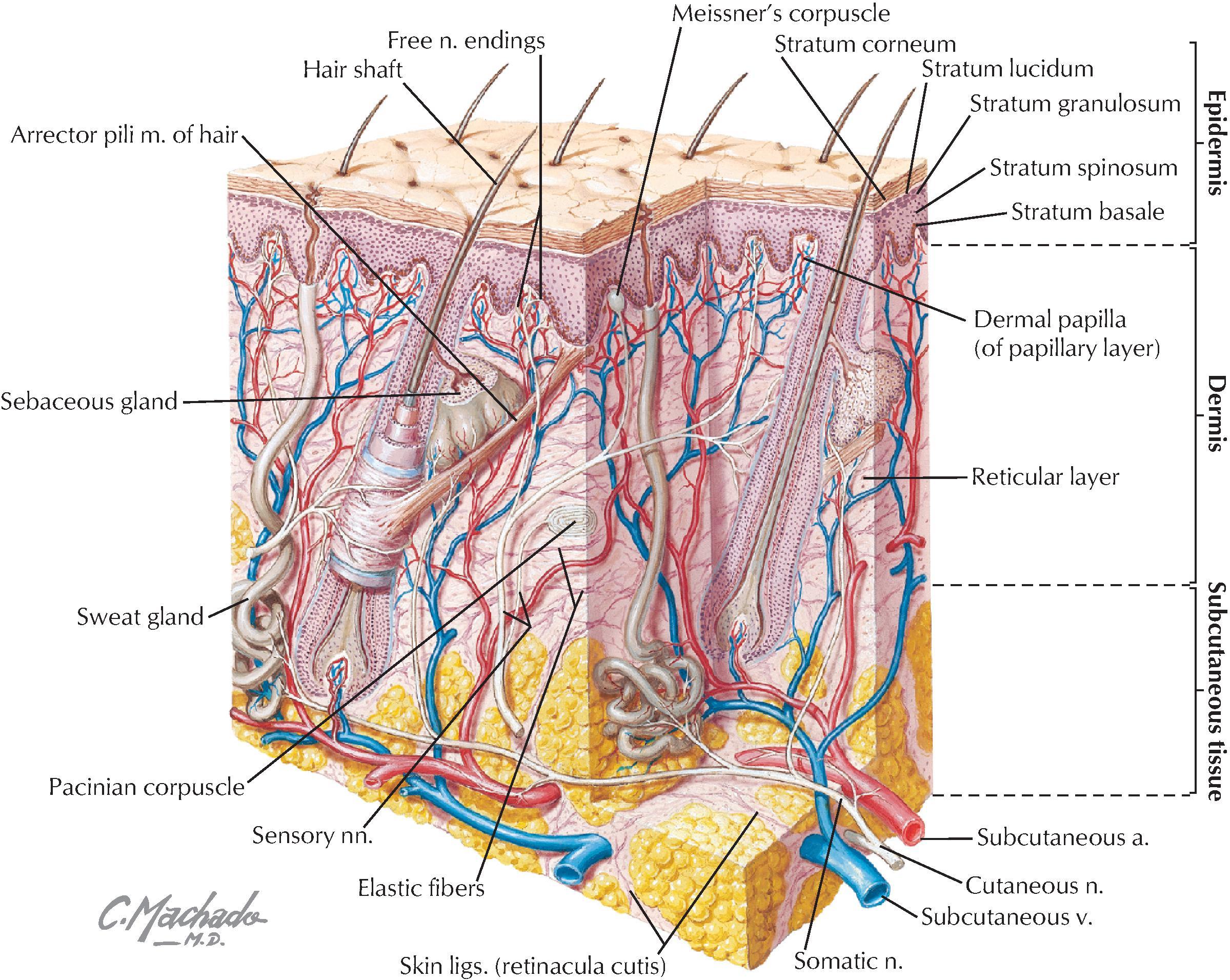
Fascia is a connective tissue sheet that may contain variable amounts of fat. It can interconnect structures, provide a conduit for vessels and nerves (termed neurovascular bundles ), and provide a sheath around structures (e.g., muscles) that permits them to slide over one another easily. Superficial fascia is attached to and lies just beneath the dermis of the skin and can vary in thickness and density; it acts as a cushion, contains variable amounts of fat, and allows the skin to glide over its surface. Deep fascia usually consists of a dense connective tissue, is attached to the deep surface of the superficial fascia, and often ensheathes muscles and divides them into functional groupings. Extensions of the deep fascia encasing muscles also may course inward and attach to the skeleton, dividing groups of muscles with intermuscular septa. Common injuries to the skin include abrasions, cuts (lacerations), and burns. Burns are classified as follows:
First-degree: burn damage that is limited to the superficial layers of the epidermis; termed a superficial burn, clinically it causes erythema (redness of the skin).
Second-degree: burn damage that includes all of the epidermis and extends into the superficial dermis; termed a partial-thickness burn, it causes blisters but spares the hair follicles and sweat glands.
Third-degree: burn damage that includes all the epidermis and dermis and may even involve the subcutaneous tissue and underlying deep fascia and muscle; termed a full-thickness burn, it causes charring.
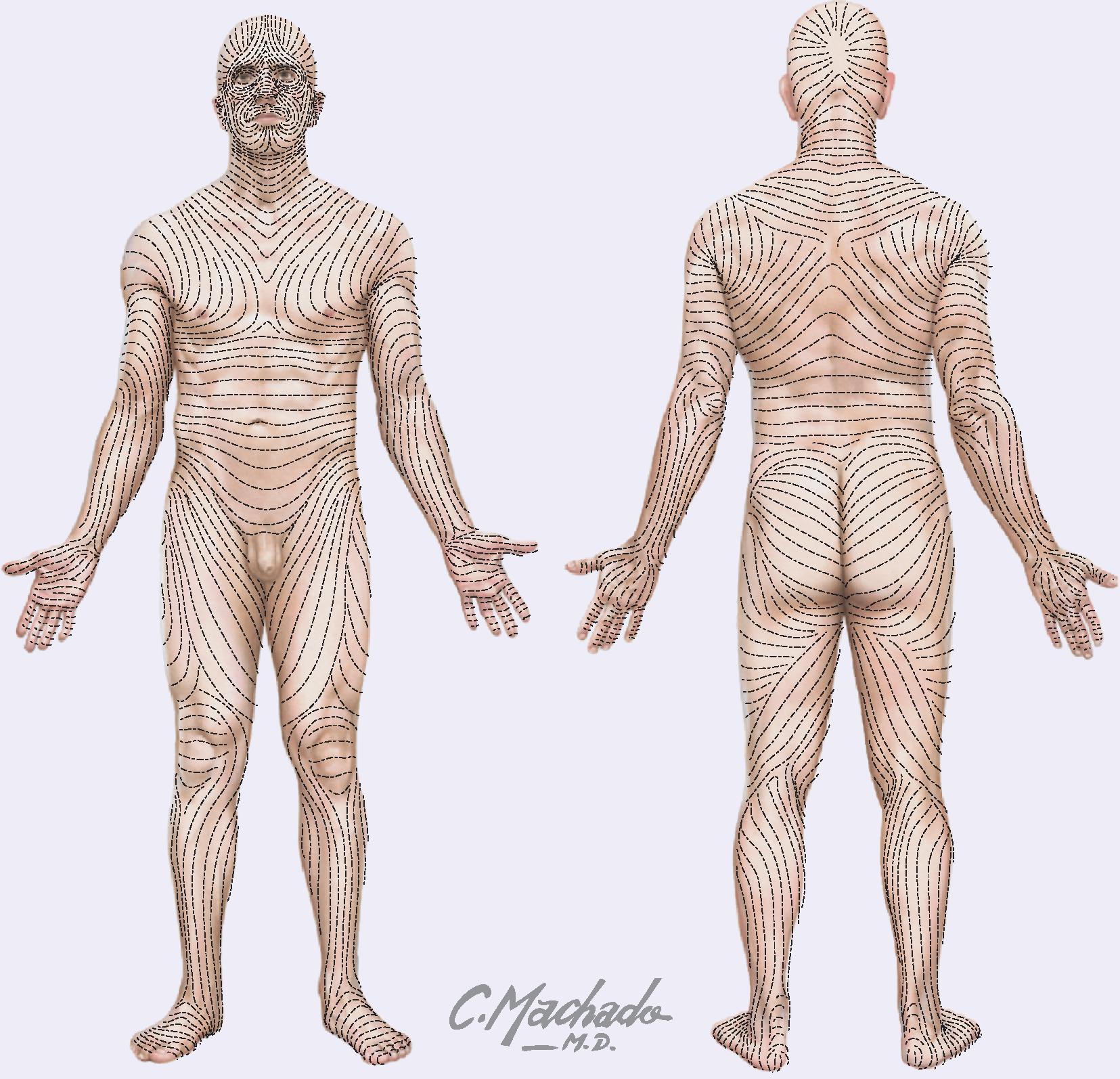
Collagen in the skin creates tension lines called Langer’s lines. Surgeons sometimes use these lines to make skin incisions; other times, they may use the natural skin folds. The resulting incision wounds tend to gape less when the incision is parallel to Langer’s lines, resulting in a smaller scar after healing. However, skin fold incisions also may conceal the scar following healing of the incision.
The human skeleton is divided into two descriptive regions ( Fig. 1.5 ):
Axial skeleton: includes the bones of the skull, vertebral column (spine), ribs, and sternum, which form the “axis” or central line of the body (80 bones).
Appendicular skeleton: includes the bones of the limbs, including the pectoral and pelvic girdles, which attach the limbs to the body’s axis (134 bones).
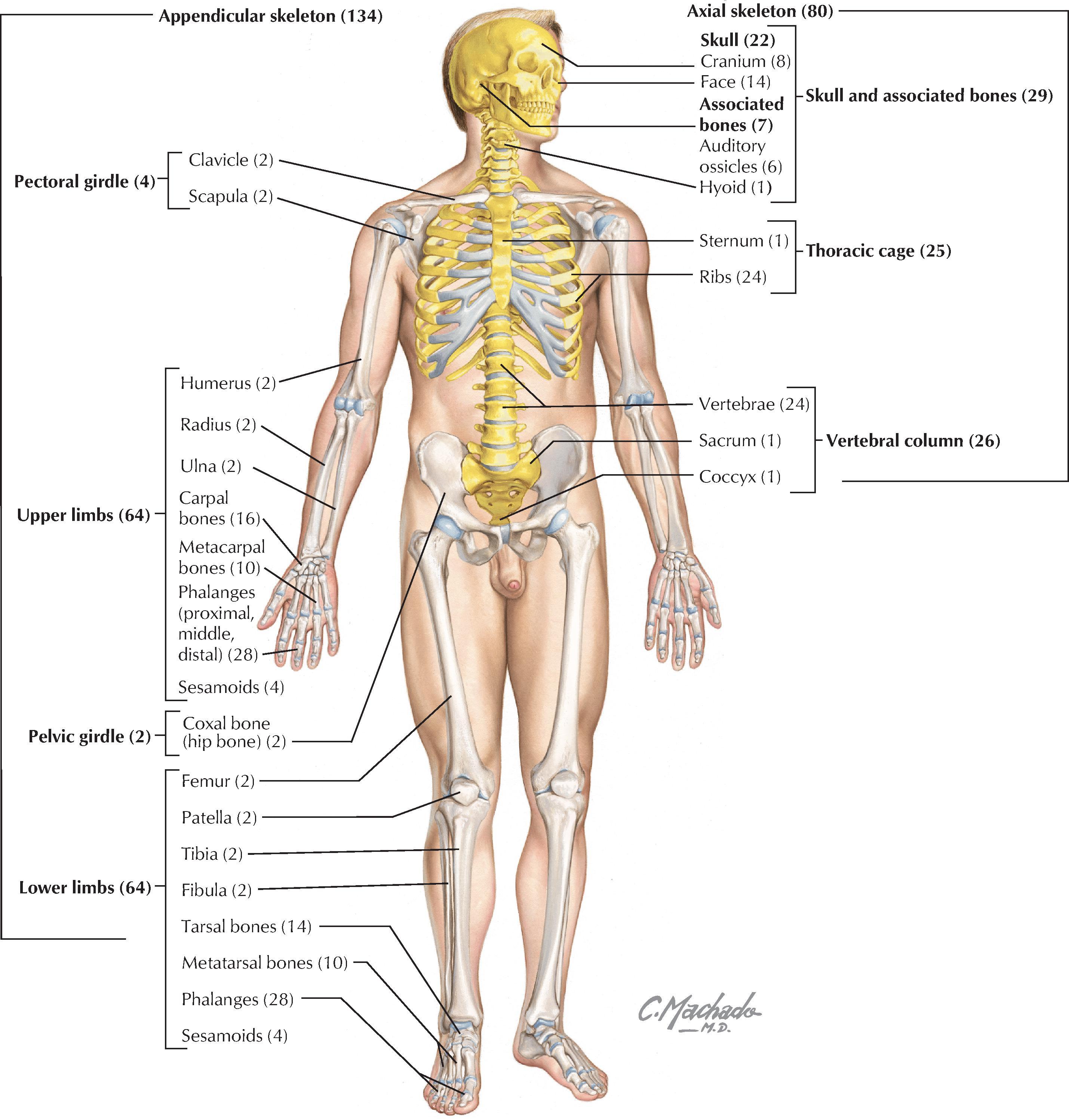
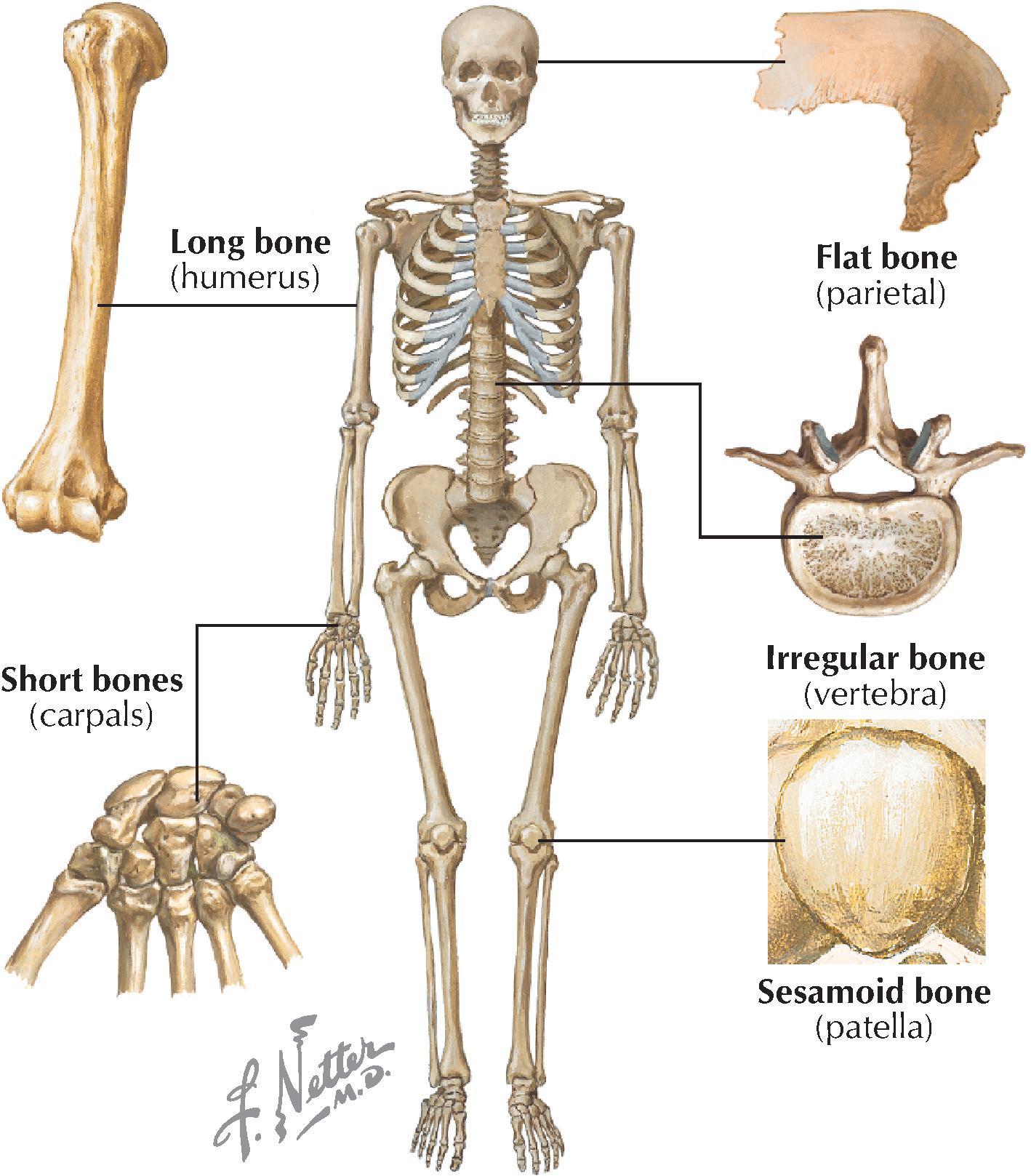
The skeleton is composed of a living, dynamic, rigid connective tissue that forms the bones and cartilages. Generally, humans have about 214 bones, although this number varies, particularly in the number of small sesamoid bones that may be present. (Typically, we have 8 sesamoid bones of the hands and feet.) Cartilage is attached to some bones, especially where flexibility is important, or covers the surfaces of bones at points of articulation. About 99% of the body’s calcium is stored in bone, and many bones possess a central cavity that contains bone marrow—a collection of hemopoietic (blood-forming) cells. Most of the bones can be classified into one of the following five shapes ( Fig. 1.6 ):
Long.
Short.
Flat.
Irregular.
Sesamoid.
The functions of the skeletal system include:
Support.
Protection of vital organs.
A mechanism, along with muscles, for movement.
Storage of calcium and other salts, growth factors, and cytokines.
A source of blood cells.
There are two types of bone:
Compact: is a relatively solid mass of bone, commonly seen as a superficial layer of bone, that provides strength.
Spongy (trabecular or cancellous): is a less dense trabeculated network of bone spicules making up the substance of most bones and surrounding an inner marrow cavity.
Long bones also are divided into the following descriptive regions ( Fig. 1.7 ):
Epiphysis: the ends of long bones, which develop from secondary ossification centers.
Epiphysial plate: the site of growth in length; it contains cartilage in actively growing bones.
Metaphysis: the site where the bone’s shaft joins the epiphysis and epiphysial plate.
Diaphysis: the shaft of a long bone, which represents the primary ossification center and the site where growth in width occurs.
As a living, dynamic tissue, bone receives a rich blood supply from:
Nutrient arteries: usually one or several larger arteries that pass through the diaphysis and supply the compact and spongy bone, as well as the bone marrow.
Metaphysial and epiphysial arteries: usually arise from articular branches supplying the joint.
Periosteal arteries: numerous small arteries from adjacent vessels that supply the compact bone.
Various surface features of bones (ridges, grooves, and bumps) result from the tension placed on them by the attachment of tendons, ligaments, and fascia, as well as by neurovascular bundles or other structures that pass along the bone. Descriptively, these features include the following:
Condyle: a rounded articular surface covered with articular (hyaline) cartilage.
Crest: a ridge (narrow or wide) of bone.
Epicondyle: a prominent ridge or eminence superior to a condyle.
Facet: a flat, smooth articular surface, usually covered with articular (hyaline) cartilage.
Fissure: a very narrow “slitlike” opening in a bone.
Foramen: a round or oval “hole” in the bone for passage of another structure (nerve or vessel).
Fossa: a “cuplike” depression in the bone, usually for articulation with another bone.
Groove: a furrow in the bone.
Line: a fine linear ridge of bone, but less prominent than a crest.
Malleolus: a rounded eminence.
Meatus: a passageway or canal in a bone.
Notch: an indentation along the edge of a bone.
Process: a bony prominence that may be sharp or blunt.
Protuberance: a protruding eminence on an otherwise smooth surface.
Ramus: a thin part of a bone that joins a thicker process of the same bone.
Spine: a sharp process projecting from a bone.
Trochanter: large, blunt process for muscle tendon or ligament attachment.
Tubercle: a small, elevated process.
Tuberosity: a large, rounded eminence that may be coarse or rough.
Bones develop in one of the following two ways:
Intramembranous formation: most flat bones develop in this way by direct calcium deposition into a mesenchymal (primitive mesoderm) precursor or model of the bone.
Endochondral formation: most long and irregularly shaped bones develop by calcium deposition into a cartilaginous model of the bone that provides a scaffold for the future bone.
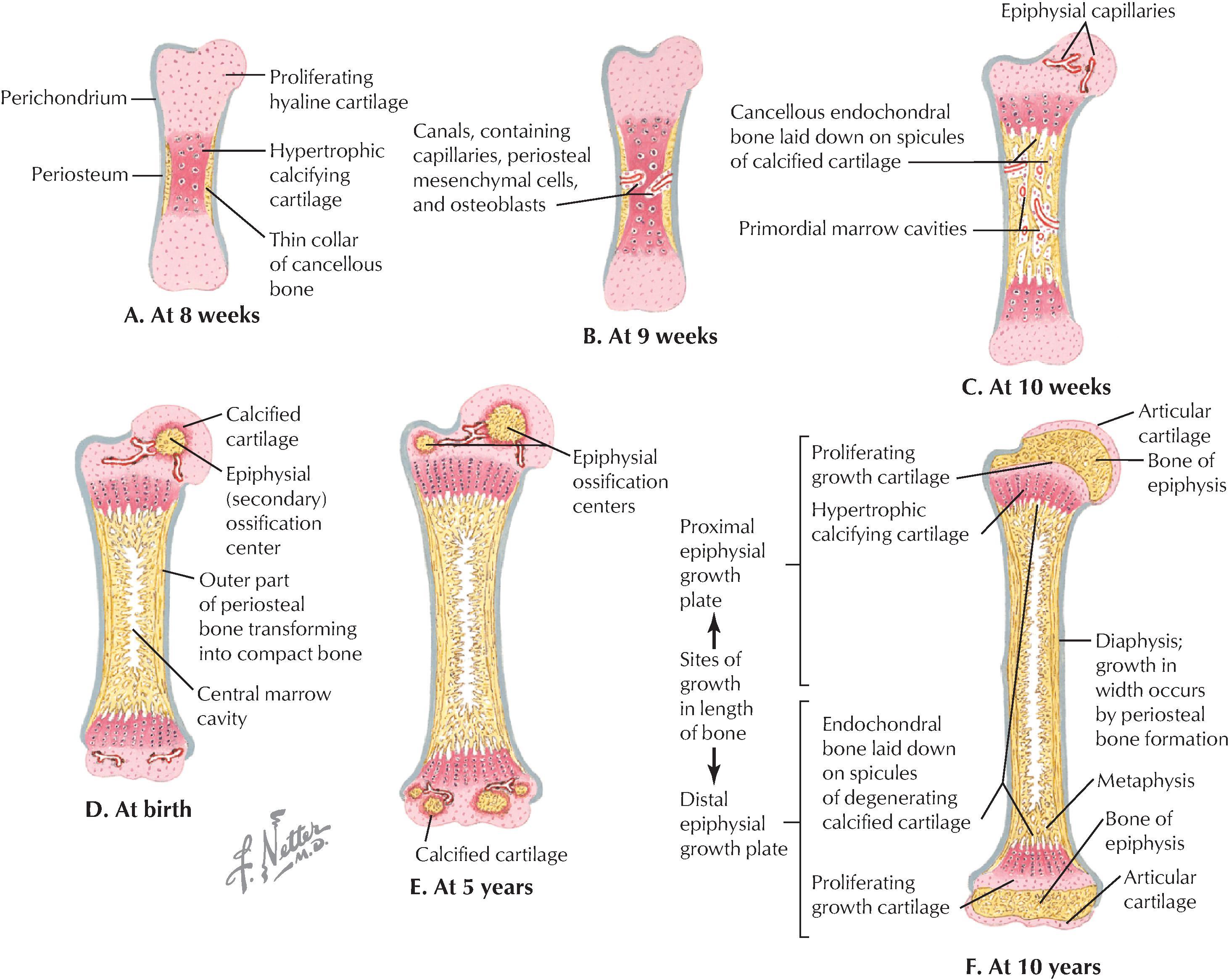
The following sequence of events defines endochondral bone formation ( Fig. 1.7, A-F ):
Formation of a thin collar of bone around a hyaline cartilage model.
Cavitation of the primary ossification center and invasion of vessels, nerves, lymphatics, red marrow elements, and osteoblasts.
Formation of spongy (cancellous) endochondral bone on calcified spicules.
Diaphysis elongation, formation of the central marrow cavity, and appearance of the secondary ossification centers in the epiphyses.
Long bone growth during childhood.
Epiphysial fusion occurring from puberty into maturity (early to mid-20s).
Joints are the sites of union or articulation of two or more bones or cartilages, and are classified into one of the following three types ( Fig. 1.8 ):
Fibrous (synarthroses): bones joined by fibrous connective tissue.
Cartilaginous (amphiarthroses): bones joined by cartilage, or by cartilage and fibrous tissue.
Synovial (diarthroses): in this most common type of joint, the bones are joined by a joint cavity filled with a small amount of synovial fluid and surrounded by a capsule; the bony articular surfaces are covered with hyaline cartilage.
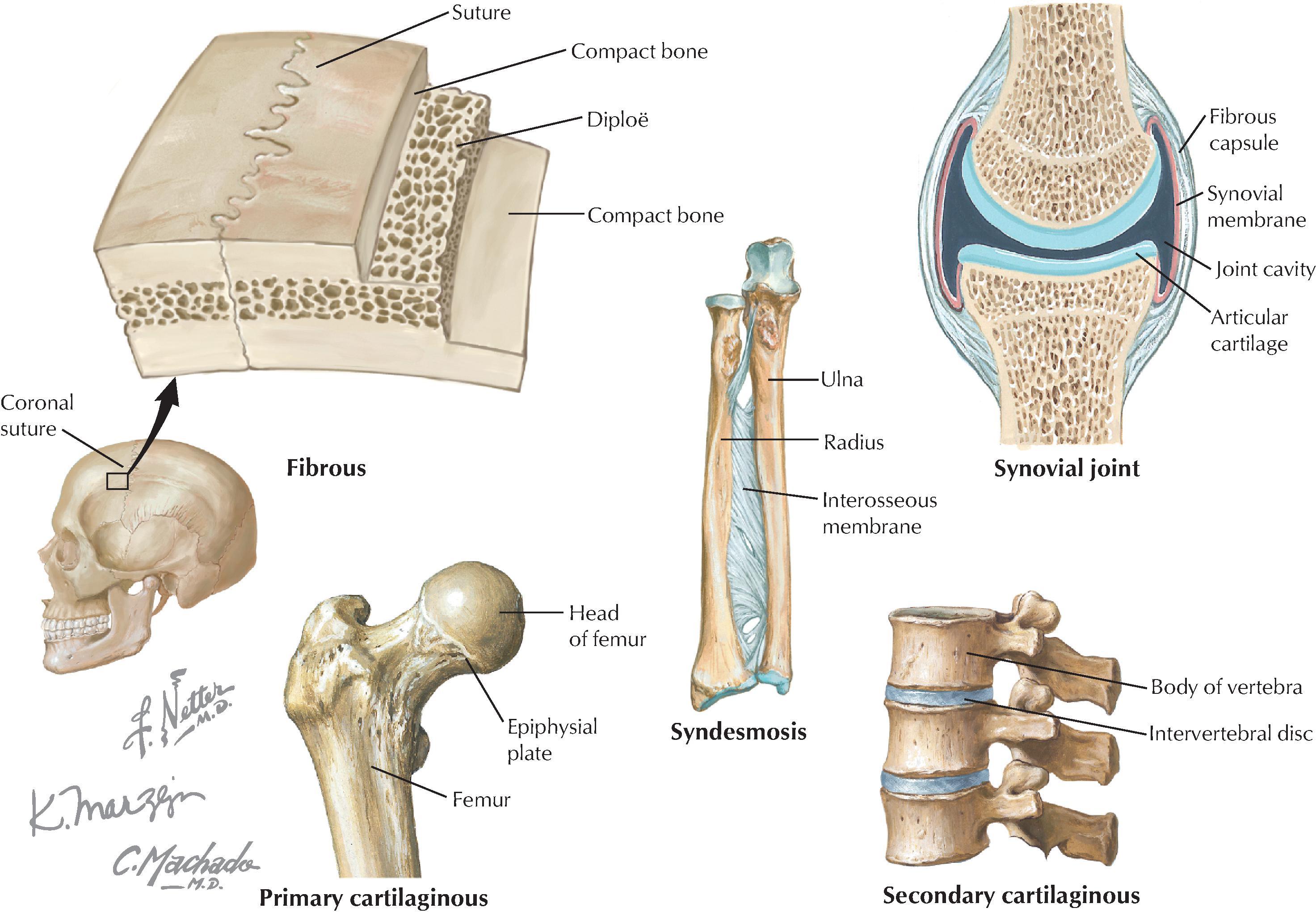
Fibrous joints include sutures (flat bones of the skull), syndesmoses (two bones connected by a fibrous membrane), and gomphoses (teeth fitting into fibrous tissue-lined sockets).
Cartilaginous joints include primary (synchondrosis) joints between surfaces lined by hyaline cartilage (epiphysial plate connecting the diaphysis with the epiphysis), and secondary (symphysis) joints between hyaline-lined articular surfaces and an intervening fibrocartilaginous disc. Primary joints allow for growth and some bending, whereas secondary joints allow for strength and some flexibility.
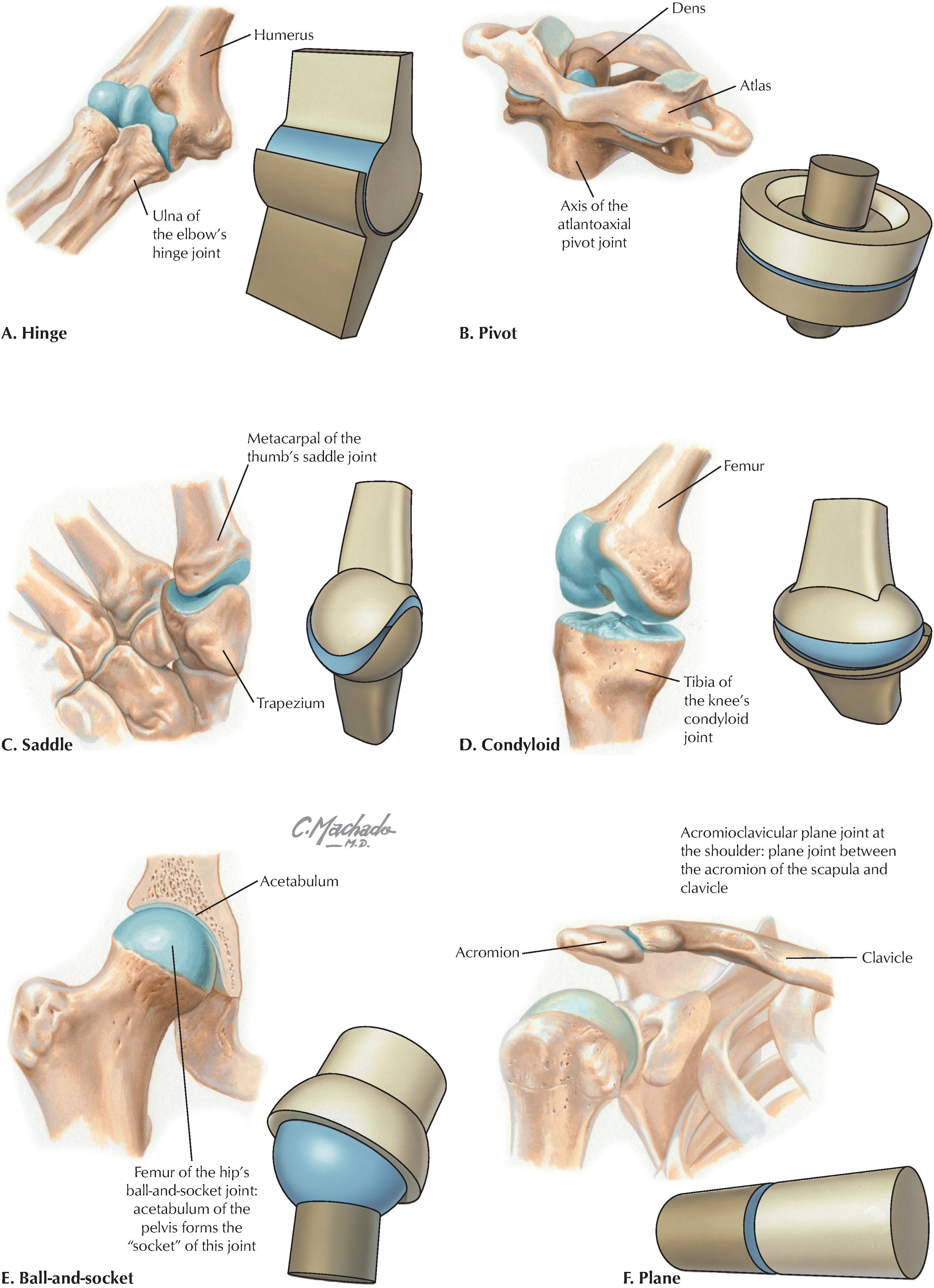
Synovial joints generally allow for considerable movement and are classified according to their shape and the type of movement that they permit (uniaxial, biaxial, or multiaxial movement) ( Fig. 1.9 ), as follows:
Hinge (ginglymus): are uniaxial joints for flexion and extension.
Pivot (trochoid): are uniaxial joints for rotation.
Saddle: are biaxial joints for flexion, extension, abduction, adduction, and circumduction.
Condyloid (ellipsoid; sometimes classified separately): are biaxial joints for flexion, extension, abduction, adduction, and circumduction.
Plane (gliding): are joints that only allow simple gliding movements.
Ball-and-socket (spheroid): are multiaxial joints for flexion, extension, abduction, adduction, mediolateral rotation, and circumduction.
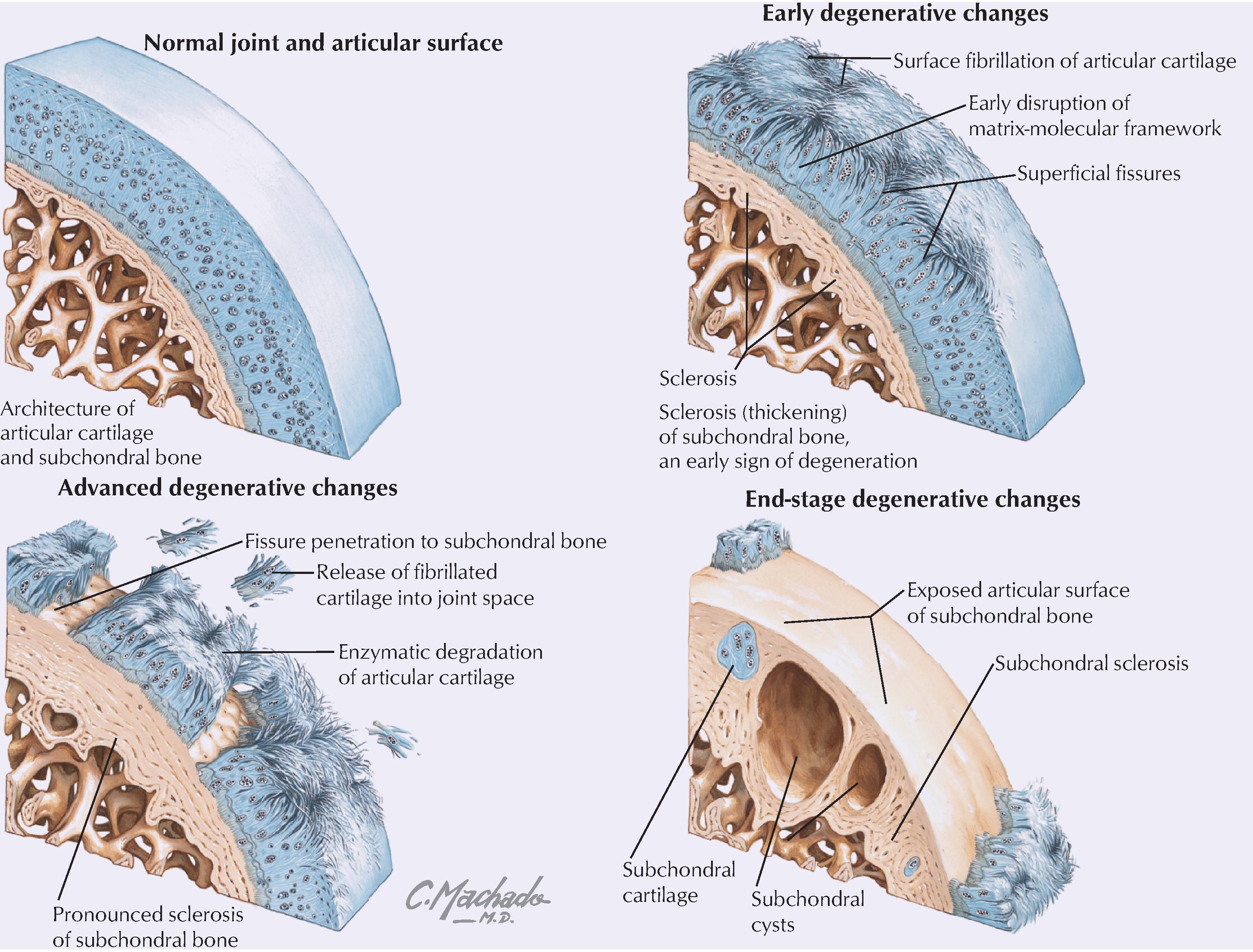
Degenerative joint disease is a catch-all term for osteoarthritis, degenerative arthritis, osteoarthrosis, or hypertrophic arthritis; it is characterized by progressive loss of articular cartilage and failure of repair. Osteoarthritis can affect any synovial joint but most often involves the foot, knee, hip, spine, and hand. As the articular cartilage is lost, the joint space (the space between the two articulating bones) becomes narrowed, and the exposed bony surfaces rub against each other, causing significant pain.
Muscle cells (fibers) produce contractions (shortenings in length) that result in movement, maintenance of posture, changes in shape, or the propulsion of fluids through hollow tissues or organs. There are three different types of muscle:
Skeletal: striated muscle fibers that are attached to bone and are responsible for movements of the skeleton (sometimes simplistically referred to as voluntary muscle ).
Cardiac: striated muscle fibers that make up the walls of the heart and proximal portions of the great veins where they enter the heart.
Smooth: nonstriated muscle fibers that line various organ systems (gastrointestinal, urogenital, respiratory), attach to hair follicles, and line the walls of most blood vessels (sometimes simplistically referred to as involuntary muscle ).
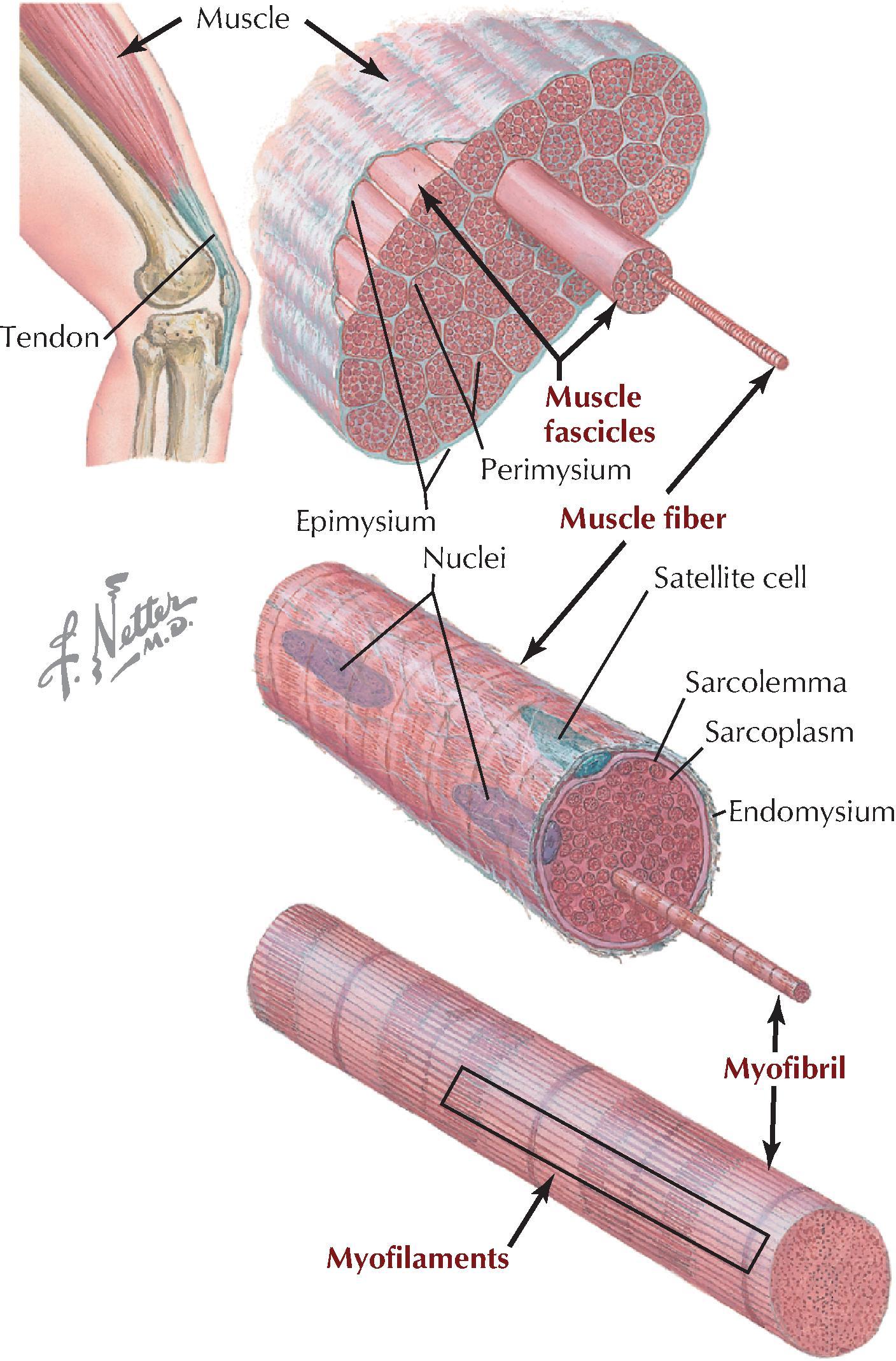
Skeletal muscle is divided into fascicles (bundles), which are composed of muscle fibers (muscle cells) ( Fig. 1.10 ). The muscle fiber cells contain longitudinally oriented myofibrils that run the full length of the cell. Each myofibril is composed of many myofilaments, which are composed of individual myosin (thick filaments) and actin (thin filaments) that slide over one another during muscle contraction.
Skeletal muscle moves bones at their joints and possesses an origin (the muscle’s fixed or proximal attachment) and an insertion (the muscle’s movable or distal attachment). In a few instances, the muscle’s origin moves more than its insertion. At the gross level, anatomists classify muscle on the basis of its shape:
Flat: muscle that has parallel fibers, usually in a broad flat sheet with a broad tendon of attachment called an aponeurosis.
Quadrate: muscle that has a four-sided appearance.
Circular: muscle that forms sphincters that close off tubes or openings.
Digastric: two muscles in series and connected by a common tendon.
Fusiform: muscle that has a wide center and tapered ends.
Pennate: muscle that has a feathered appearance (unipennate, bipennate, or multipennate forms).
Muscle contraction shortens the muscle. Generally, skeletal muscle contracts in one of three ways:
Reflexive: involuntary or through automatic contraction; seen in the diaphragm during respiration or in the reflex contraction elicited by tapping a muscle’s tendon with a reflex hammer.
Tonic: maintains “muscle tone,” a slight contraction that may not cause movement but allows the muscle to maintain firmness necessary for stability of a joint and important in maintaining posture.
Phasic: includes two types of contraction: isometric contraction , where no movement occurs but the muscle maintains tension to hold a position (stronger than tonic contraction); and isotonic contraction , where the muscle shortens to produce movement.
Muscle contraction that produces movements can act in several ways, depending on the conditions:
Agonist: the main muscle responsible for a specific movement (the “prime mover”).
Antagonist: the muscle that opposes the action of the agonist; as an agonist muscle contracts, the antagonistic muscle relaxes.
Fixator: one or more muscles that steady the proximal part of a limb when a more distal part is being moved.
Synergist: a muscle, or muscles, that complements (works synergistically with) the contraction of the agonist, either by assisting with the movement generated by the agonist or by reducing unnecessary movements that would occur as the agonist contracts.
The cardiovascular system consists of (1) the heart , which pumps blood into the pulmonary circulation for gas exchange and into the systemic circulation to supply the body tissues; and (2) the vessels that carry the blood, including the arteries, arterioles, capillaries, venules, and veins. The blood passing through the cardiovascular system consists of the following formed elements ( Fig. 1.11 ):
Platelets.
White blood cells (WBCs).
Red blood cells (RBCs).
Plasma.
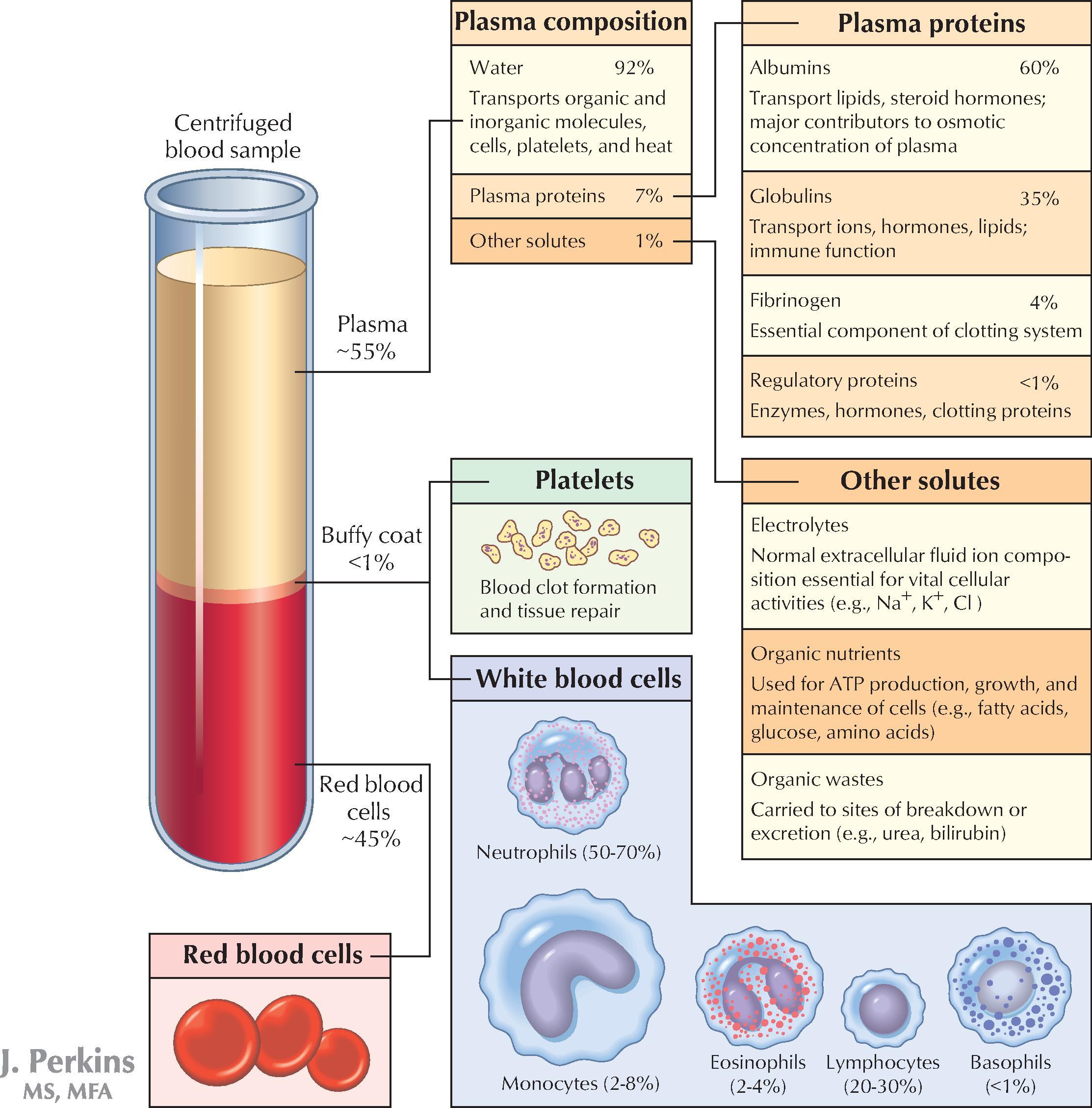
Blood is a fluid connective tissue that circulates through the arteries to reach the body’s tissues and then returns to the heart through the veins. When blood is “spun down” in a centrifuge tube, the RBCs precipitate to the bottom of the tube, where they account for about 45% of the blood volume. This is called the hematocrit and normally ranges from 40% to 50% in males and 35% to 45% in females. The next layer is a “buffy coat,” which makes up slightly less than 1% of the blood volume and includes WBCs (leukocytes) and platelets. The remaining 55% of the blood volume is the plasma and includes water, plasma proteins, clotting factors, and various solutes ( serum is plasma with the clotting factors removed). The functions of blood include:
Transport of dissolved gases, nutrients, metabolic waste products, and hormones to and from tissues.
Prevention of fluid loss via clotting mechanisms.
Immune defense.
Regulation of pH and electrolyte balance.
Thermoregulation through blood vessel constriction and dilation.
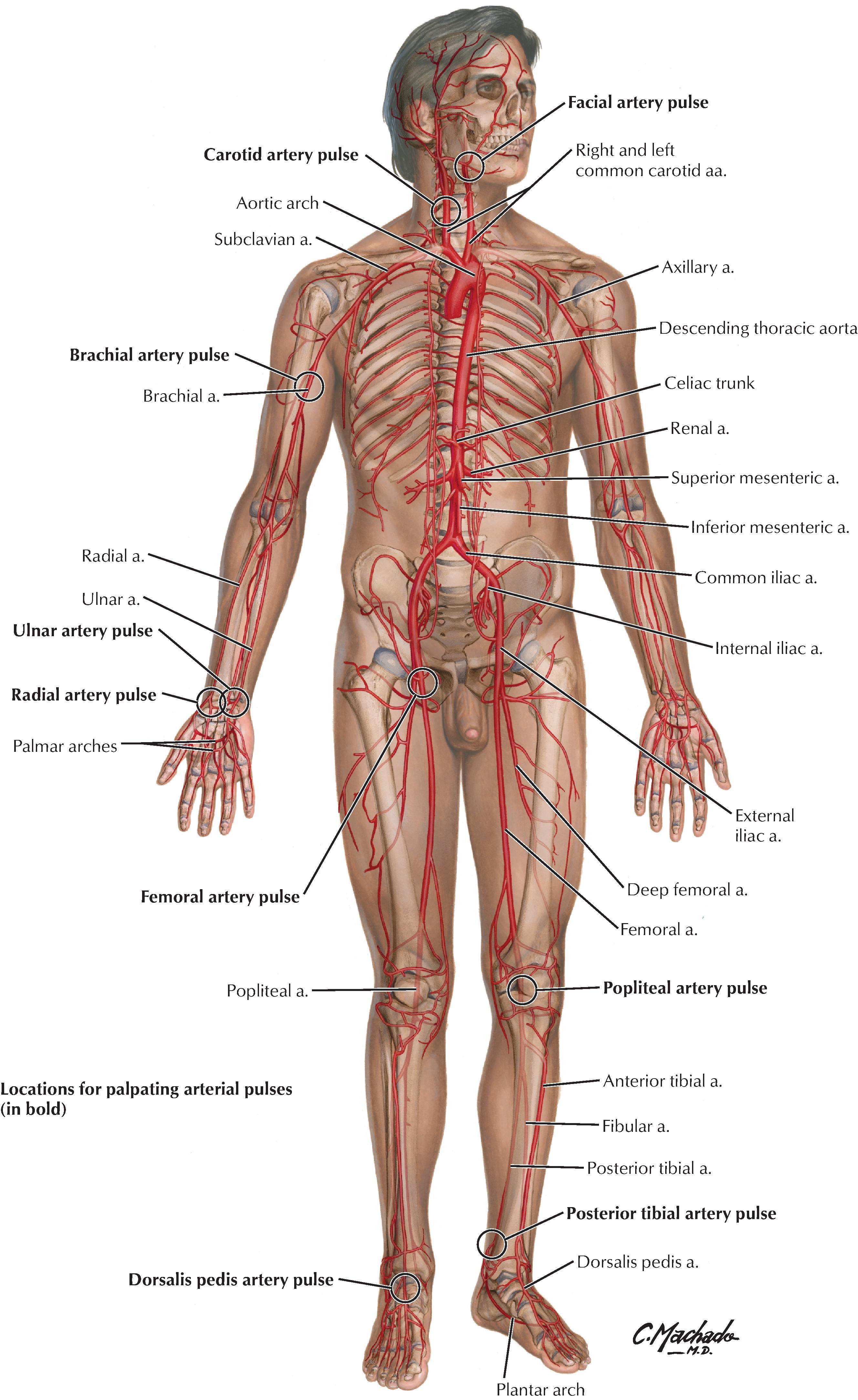
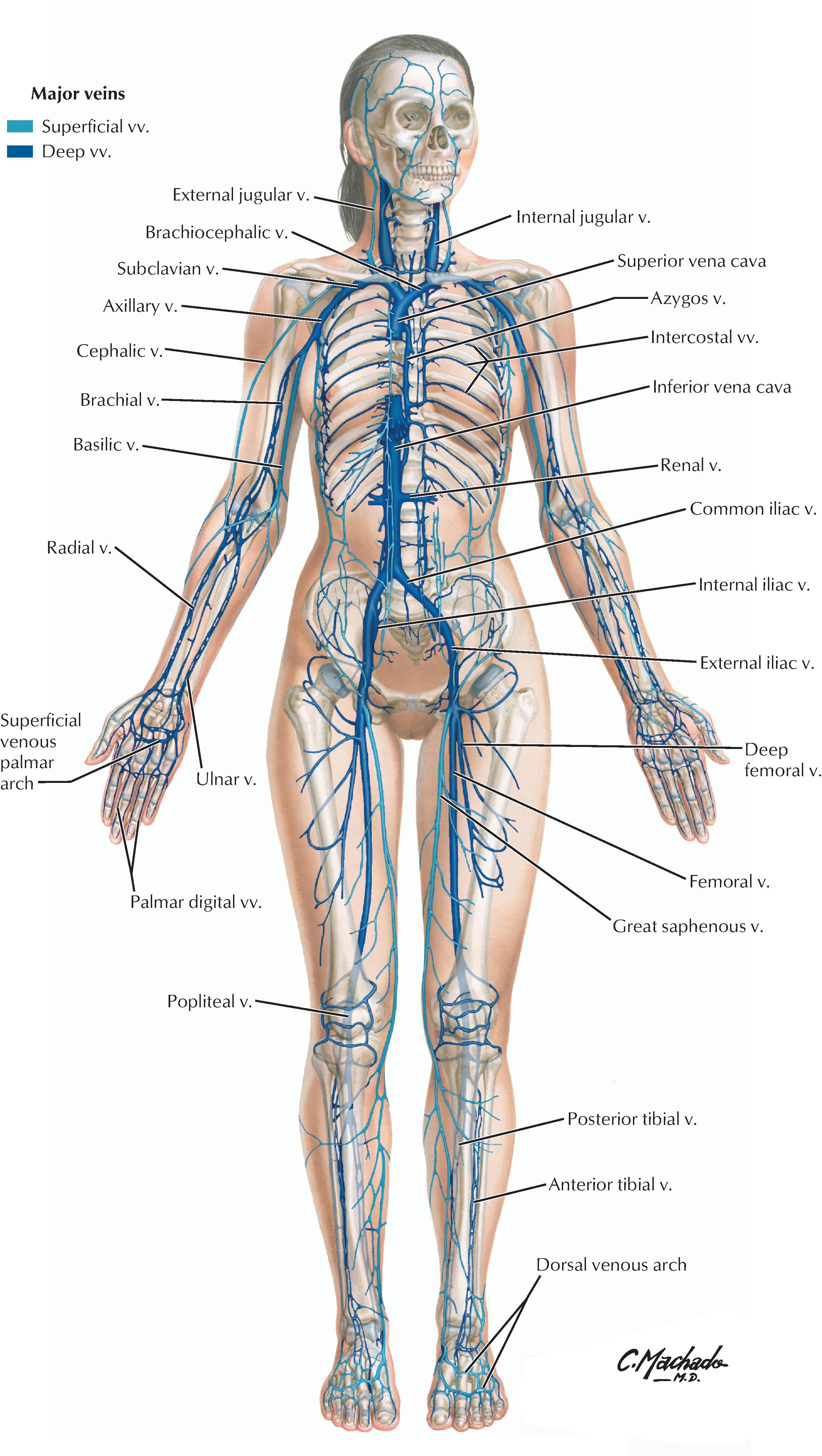
Blood circulates through the blood vessels ( Fig. 1.12 ). Arteries carry blood away from the heart, and veins carry blood back to the heart. Arteries generally have more smooth muscle in their walls than veins and are responsible for most of the vascular resistance, especially the small muscular arteries and arterioles. Capillaries are simple microscopic tubes with very thin walls connecting arteries to veins; they constitute more that 90% of all the blood vessels in the human body. At any point in time, most of the blood resides in the veins (about 64%) and is returned to the right side of the heart; thus veins are the capacitance vessels, capable of holding most of the blood, and are far more variable and numerous than their corresponding arteries.
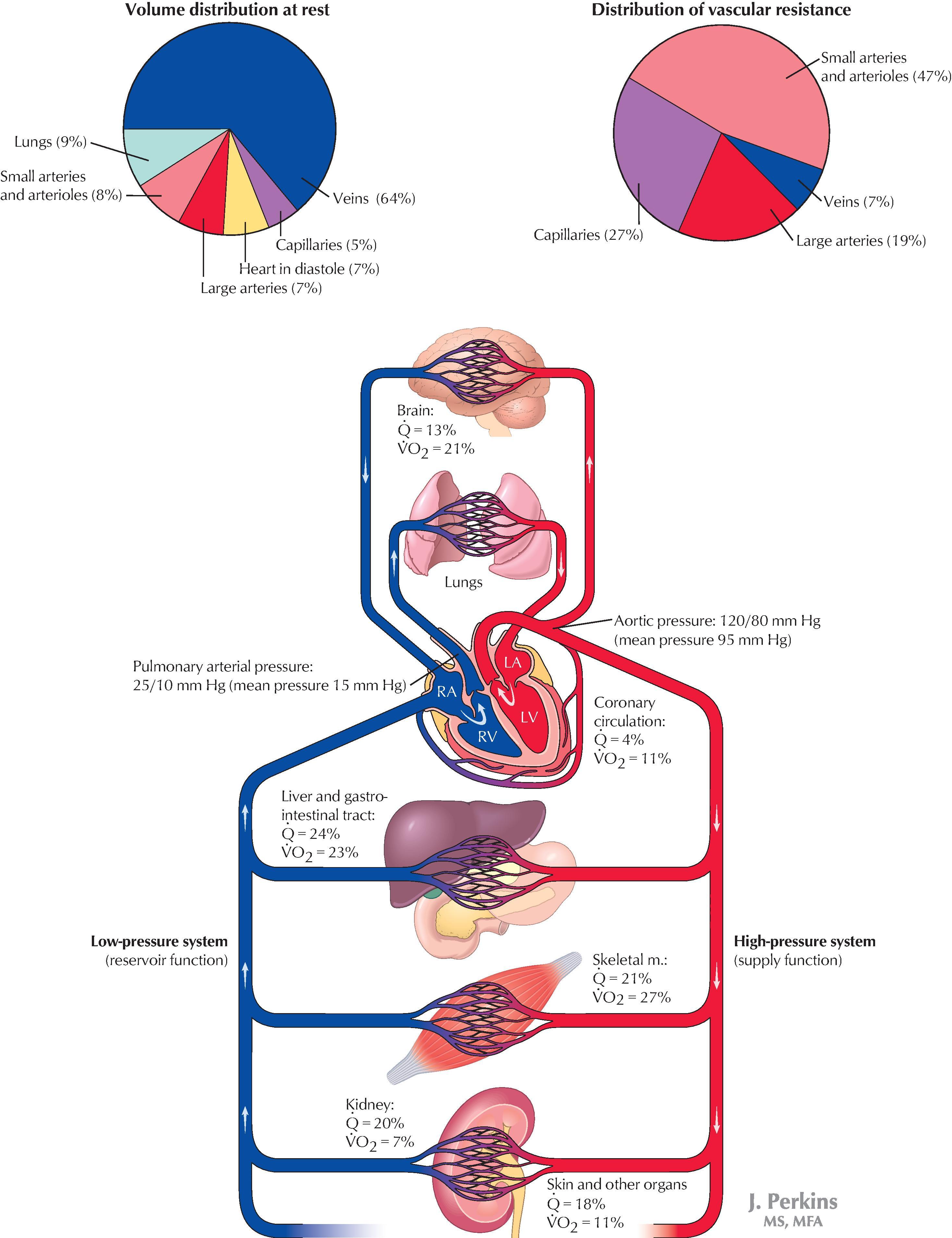
The major arteries are illustrated in Fig. 1.13 . At certain points along the pathway of the systemic arterial circulation, large and medium-sized arteries lie near the body’s surface and can be used to take a pulse by compressing the artery against a hard underlying structure (usually a bone). The most distal pulse from the heart is usually taken over the dorsalis pedis artery on the dorsum of the foot or by the posterior tibial artery pulse, at the medial aspect of the ankle.
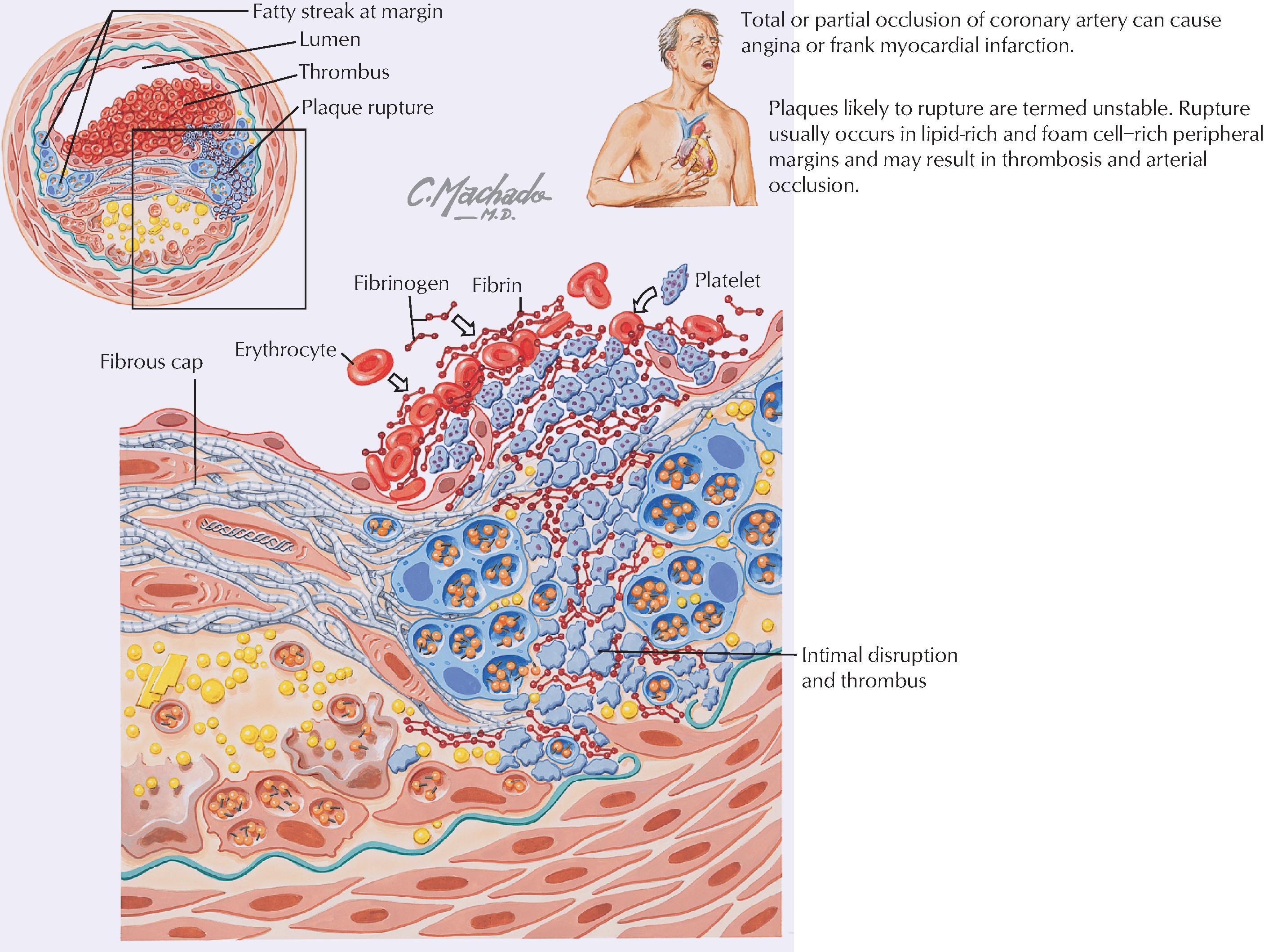
Thickening and narrowing of the arterial wall and eventual deposition of lipid into the wall can lead to one form of atherosclerosis. The narrowed artery may not be able to meet the metabolic needs of the adjacent tissues, which may become ischemic. Multiple factors, including focal inflammation of the arterial wall, may result in this condition. When development of a plaque is such that it is likely to rupture and lead to thrombosis and arterial occlusion, the atherogenic process is termed unstable plaque formation.
The major veins are illustrated in Fig. 1.14 . Veins are capacitance vessels because they are distensible and numerous and can serve as reservoirs for the blood. Because veins carry blood at low pressure and often against gravity, larger veins of the limbs and lower neck region have numerous valves that aid in venous return to the heart (several other veins throughout the body may also contain valves). Both the presence of valves and the contractions of adjacent skeletal muscles help to “pump” the venous blood against gravity and toward the heart. In most of the body, the veins occur as a superficial set of veins in the subcutaneous tissue that connects with a deeper set of veins that parallel the arteries. Types of veins include:
Venules: these are very small veins that collect blood from the capillary beds.
Veins: these are small, medium, and large veins that contain some smooth muscle in their walls, but not as much as their corresponding arteries.
Portal venous systems: these are veins that transport blood between two capillary beds (e.g., the hepatic portal system draining the GI tract).
The heart is a hollow muscular (cardiac muscle) organ that is divided into four chambers ( Figs. 1.12, 1.15 ):
Right atrium: receives the blood from the systemic circulation via the superior and inferior venae cavae.
Right ventricle: receives the blood from the right atrium and pumps it into the pulmonary circulation via the pulmonary trunk and pulmonary arteries.
Left atrium: receives the blood from the lungs via pulmonary veins.
Left ventricle: receives the blood from the left atrium and pumps it into the systemic circulation via the aorta.
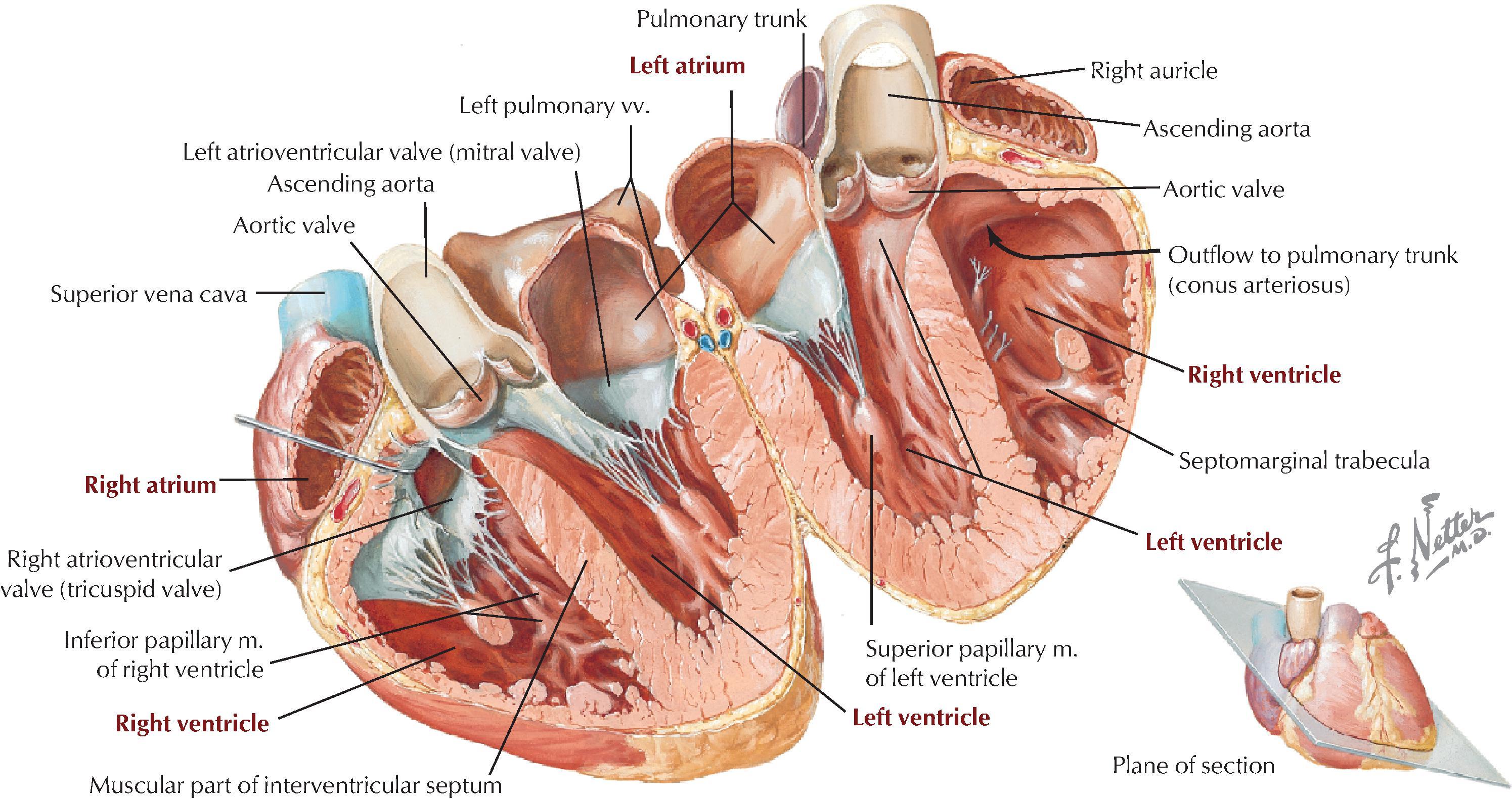
The atria and ventricles are separated by atrioventricular valves ( tricuspid on the right side and mitral on the left side) that prevent the blood from refluxing into the atria when the ventricles contract. Likewise, the two major outflow vessels, the pulmonary trunk from the right ventricle and the ascending aorta from the left ventricle, possess the pulmonary (pulmonic) valve and the aortic valve (both semilunar valves), respectively.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here