Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
How is pain defined?
In 1994, thought leaders in the International Association for the Study of Pain defined pain as follows: “An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms as such.”
Can pain occur without tissue injury or impending tissue damage?
Yes. While pain most commonly starts with a noxious or injuring stimulus, it may be initiated de novo in the central nervous system (CNS) without any stimulus. A noxious stimulus may occur at any tissue that triggers a cascade of physiologic events that should cause pain, but pain may not always be perceived.
How can you have a painful stimulus or tissue injury yet not perceive pain?
The brain can evoke an inhibitory influence on ascending neural transmission. Emotional shock, decreased level of consciousness, and cerebral dysfunction are some examples of a disconnection between painful stimulus and pain perception.
What are the emotional and cognitive aspects of pain perception?
If an individual recognizes a stimulus as painful but is emotionally indifferent to pain, then there is no sense of suffering—no distress, no anguish. The impact of the pain is largely nullified by a lack of an emotional, interpretive context.
Describe the physiologic events from the time of painful stimulus to the actual perception of pain.
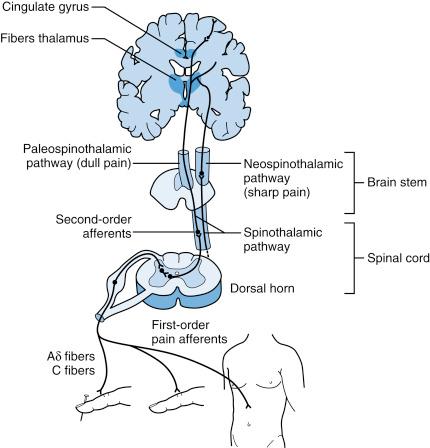
Using Fig. 27-1 one can track pain processing from the stimulus delivered at a finger to nerves ascending the somatosensory pathway from the peripheral nervous system to the brain. The depiction of a nail going through the fingertip is the pain stimulus. This painful stimulus first encounters the afferent nociceptors. Most nociceptors are bare nerve endings. Pain-conveying fibers are either C-fibers or A-delta nerve fibers.
How does the noxious stimulus evoke a response at the nociceptor?
The noxious stimulus interacts with transduction channels at the nerve ending. Some channels respond to thermal stimuli (TRPV1), cold (TRPM1, TRPM8), and chemical/mechanical stimuli (TRPA1). Nociceptive stimuli activate these transduction channels and initiate the influx of a sodium and calcium current, thus causing depolarization and the propagation of current down the axon. This conversion of heat, cold, chemical, or mechanical energy to an electrical impulse at the nerve terminal is called transduction .
What is a primary afferent?
The primary afferent is the peripheral nerve from the tissue where the stimulus is encountered. This afferent conveys a train of impulses toward the spinal cord. The afferent is essentially a sensory nerve transmitting impulses toward the CNS.
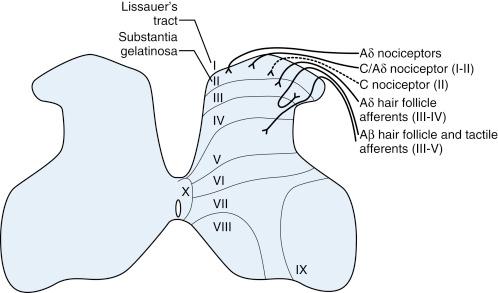
What happens at the nerve terminal in the spinal cord?
The peripheral sensory nerve has its cell body at the dorsal ganglion. Its dendrites, which function as a nerve terminal, project into the spinal cord at lamina I and II. Neurotransmitters such as substance P, neurokinin-1 (NK-1), calcitonin gene-related peptide (CGRP), and glutamate are released at the terminal in the dorsal horn. All of these transmitters are excitatory. They provoke the influx of sodium and calcium into the cell of the second-order neuron. The second-order neuron is in lamina I (Lissauer’s tract) or lamina II (substantia gelatinosa).
Binshtok AM: Mechanisms of nociceptive transduction and transmission: a machinery for pain sensation and tools for selective analgesia. Rev Neurobiol 97:143-147, 2011.
Woolf CJ, Ma Q: Nociceptors—noxious stimulus detectors. Neuron 55(3):353-364, 2007.
How does the primary afferent synapse or interact with dorsal horn neurons?
There are interneurons that have intervening synapses between some of the primary afferents and neurons at deeper layers in the dorsal horn such as lamina V. Some of these lamina V neurons have long dendrites extending into lamina II and synapse directly with primary afferents. The dorsal horn is a very fertile territory for modulatory influences from descending nerves arising from higher centers as well as local interneurons. The interneurons are typically inhibitory. The preponderant influence from descending neural input is also inhibitory. See Table 27-1 for a summary of dorsal horn neurotransmitters or ligands.
| Receptor | Drug or Neurotransmitter | Channel and Direction | Effect |
|---|---|---|---|
| GABA-A | GABA | Chloride influx | Inhibitory |
| GABA-B | GABA | Potassium influx | Inhibitory |
| Glycine | Glycine | Chloride influx | Inhibitory |
| Opioid | Opioids | Potassium influx | Inhibitory |
| μ, κ, σ | Opioids | Potassium influx | Inhibitory |
| α1, α2 | Norepinephrine | Potassium influx | Inhibitory |
| SHT | Serotonin | Potassium influx | Inhibitory |
| AMPA | Glutamate | Sodium influx | Excitatory |
| NMDA | Glutamate | Sodium and calcium influx | Excitatory |
| NK-1 | Substance-P | Sodium and calcium influx | Excitatory |
| NK-1,2 | NK-1 | Sodium and calcium influx | Excitatory |
| CCGP | CGRP | Sodium and calcium influx | Excitatory |
| GABA-B | Baclofen | Potassium influx | Inhibitory |
| GABA-A | Benzodiazepine | Chloride influx | Inhibitory |
| Gabapentinoid receptor | Gabapentin/Pregabalin | Blocks calcium, L-type | Inhibitory |
| α1, α2 | SNRI | Potassium influx | Inhibitory |
| 5-HT | SNRI | Potassium influx | Inhibitory |
| NMDA | Ketamine | Sodium and calcium influx | Excitatory |
| Conopeptide receptor | ω-Conopeptide | Blocks calcium, N-type | Inhibitory |
Once the primary afferent synapses with the second-order neuron, where does the second-order neuron project?
The axon of the second-order neuron projects as the spinothalamic tract. It descends to ventromedial gray and crosses the midline through the anterior commissure and then ascends in the ventrolateral white matter of the cord as the spinothalamic tract (neospinothalamic). There is also a multisynaptic spinothalamic tract that ascends in the dorsomedial white matter of the spinal cord near the midline. This is called the paleospinothalamic tract . These tracts ascend to the brain stem, thalamus, somatosensory cortex, and limbic system ( Fig. 27-2 ).
How do the functions of the neospinothalamic and paleospinothalamic tracts differ?
The lateral spinothalamic tract (neospinothalamic tract) ascends to the thalamus and cortex with few synaptic connections. Therefore, sharp pain and the avoidance response can be evoked due to the rapid transmission and perception of pain. In contrast, the dorsomedial thalamic tract (paleothalamic tract) synapses at multiple locations, including the recticular activating system, before reaching the thalamus and limbic system. Transmission along the paleothalamic system is slow and associated with more indolent visceral-autonomic and emotional/behavioral responses.
Yalsh TL, Wiese AJ: Survey of systems involved in nociceptive processing. In Deer TR, Leong MS, Buvanendran A, et al. (eds): Comprehensive treatment of chronic pain by medical, interventional, and integrative approaches. New York: Springer, 2013, pp 3-21.
Describe the descending pain inhibitory system.
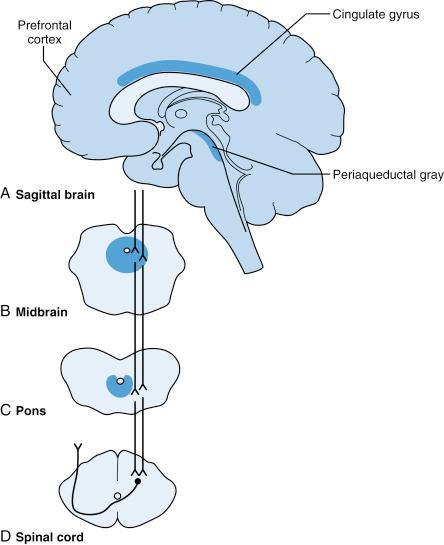
From the prefrontal cortex, cingulate gyrus, and other limbic structures, inhibitory outflow descends to the thalamus and periaqueductal gray to the reticular region of the pons and medulla. From the brain stem nuclei, projections head to the spinal cord. There are serotonergic, noradrenergic, and opioidergic neurons that provide inhibitory pain input at the dorsal horn ( Fig. 27-3 ).
Name some treatments that block pain transmission at the primary afferent level.
Injection of anesthetic drugs like lidocaine blocks sodium channels at the nerve terminal and axon. This blockade prevents depolarization and transmission of impulses. Another approach is to deplete substance P from the cutaneous nerve terminal with capsaicin. This depletion does not completely prevent pain transmission but reduces pain sensitivity at the cutaneous field supplied by the primary afferent.
Fishman SM, Ballantyne JC, Rathmell JP (eds): Bonica’s management of pain, 4th ed. New York: Lippincott Williams & Wilkins, 2009.
Describe pharmacologic interventions at the spinal cord and higher centers that inhibit pain.
Any drug or anesthetic approach that reduces excitatory input from primary afferents and second-order neurons results in analgesia. These drugs include opioids, serotonin–norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants, N -methyl d -aspartate (NMDA) antagonists, calcium channel blocking drugs such as gabapentin for L-type channels, and Ziconitide ® (omega-conopeptide) for N-type channels. Examples of these drugs are listed in Table 27-2 .
| Drug | Oral Route | IV Route | Duration | Half-Life |
|---|---|---|---|---|
| Morphine | 30 mg | 10 mg | 3-4 hr | 2 hr |
| Oxycodone | 20 mg | — | 4-6 hr | 4.5 hr |
| Hydromorphone | 7.5 mg | 1.5-2 mg | 4-5 hr | 2-3 hr |
| Hydrocodone | 30 mg | — | 4-6 hr | 3-4.5 hr |
| Codeine | 200 mg | 120 mg | 4-6 hr | 3 hr |
| Tapentadol | 75-100 mg | — | 4-6 hr | 4-5 hr |
| Fentanyl | — | 100 mcg | 1-2 hr | 1-2 hr |
| Buprenorphine | — | 0.4 mg | 6-12 hr | 2.2 hr IV; 37 hr SL |
How do antidepressants that inhibit norepinephrine and serotonin reuptake reduce pain?
These drugs work on the descending inhibitory pathways. They increase K + influx and block Ca ++ influx at the second-order neuron in the dorsal horn. It should be noted, however, that this mechanism of action depends on the type of 5-HT receptor since some subtypes are excitatory rather than inhibitory.
How are nociceptors sensitized?
After a burn of the skin, for example, inflammatory mediators are released at the injured tissue site. These include prostaglandins, bradykinin, protons, and cytokines. The local inflammatory milieu also triggers nociceptors to release substance P and calcitonin gene-related peptide (CGRP). These substances promote further vasodilation and facilitate the migration of inflammatory cells such as neutrophils and macrophages. Phosphorylation of the ionic channels makes these ionic channels more permeable to depolarizing ions like sodium and calcium, resulting in nerve hyperexcitability and nociceptor sensitization.
How can this sensitizing process be blocked at the tissue level?
Some examples of peripheral desensitizing methods are antiinflammatory medications such as nonsteroidal antiinflammatory drugs and corticosteroids as well as direct neural blockade with anesthetics.
What happens centrally in the spinal cord after tissue injury?
Tissue injury and inflammation result in locally released ligands that stimulate nociceptors and cause a barrage of electrical impulses from the primary afferent. Substance P, CGRP, and glutamate are released at the central nerve terminal of the primary afferent. These excitatory neurotransmitters trigger depolarization of the second-order neuron. Repeated depolarization activates G-protein-related second messengers, inducing a phosphorylation cascade and activation of transcription factors. The nerve may then upregulate its permeability to sodium and calcium and incorporate more ion channels in its membrane. Thus, the neuron becomes more sensitized to the incoming traffic of impulses.
Why is it that a blister burn becomes sensitive to light touch and stroking—stimuli that are not ordinarily painful?
This phenomenon occurs secondary to sensitization at the level of the dorsal horn. There, the C-fiber and A-delta nerve fibers conveying painful stimuli converge on second-order neurons that also receive input from A-beta fibers conveying light touch and stroking. Due to upregulation, the second-order neuron is now likely to depolarize in response to input from neurons conveying nonnoxious stimuli.
What is a wide-dynamic-range neuron?
A wide-dynamic-range neuron is the second-order neuron that receives input from primary afferents conveying impulses triggered by more than one type of stimulus modality—chemical, thermal, pressure, light touch, etc.
Are all second-order afferents wide-dynamic-range neurons?
Not necessarily. Some second-order neurons in lamina II (substantia gelatinosa) respond to only a specific type of noxious stimulus, and some may respond to multiple types of stimuli.
What is central facilitation?
Mendell and Wall determined that high-frequency C-fiber stimulation, not A-fiber stimulation, results in facilitating discharges from wide-dynamic range neurons. This phenomenon is called wind-up .
Define sensitization.
Sensitization is a left shift in the stimulus response curve such that a stimulus of lesser intensity is now able to evoke a painful response.
Define nociceptive pain.
Pain caused by stimulation of nociceptors by physical or chemical modalities such as pinch, crush, pressure, surgical incision, heat or extreme cold, or chemical irritation (such as exposure to acid or pepper).
What is neuropathic pain?
Pain caused by neuronal dysfunction, nerve injury, or disease.
What are the common features of neuropathic pain?
There may be hyperalgesia, allodynia, hyperpathia, dysesthesia, or lancinating jolts of pain. Nociceptive pain in the setting of sensitization may share some of these features. However, nociceptive pain is unlikely to be lancinating or associated with an electric jolt-like nature.
What is hyperalgesia?
Hyperalgesia is a painful reaction to a noxious stimulus that is perceived when the pain threshold is exceeded, at which point the painful response becomes exaggerated.
What is allodynia?
Allodynia is an exaggerated painful response to a nonnoxious stimulation such as light touch or stroking.
What is hyperpathia?
Hyperpathia is a general exaggerated response to painful stimuli, with no mention of threshold.
What is dysesthesia?
Dysesthesia refers to a painful, disagreeable sensation such as burning, icy-hot, prickly, itchy-prickly, intensely creepy-crawly, etc.
What is paresthesia?
Paresthesia is typically a nonpainful, tingling sensation.
What is deafferentation pain?
Deafferentation pain occurs in the setting of disruption of an afferent connection to the peripheral tissue. For example, this type of pain can occur in the setting of amputation, where nerves are transected and a limb or body part is missing, as well as brachial plexus avulsion injury and postherpetic neuralgia wherein the varicella zoster virus has destroyed the afferent input to second-order neurons.
Mendell LM, Wall PD: Responses to single dorsal horn cells to peripheral cutaneous unmyelinated fibers. Nature 206:97-99, 1965.
What is central pain?
Central pain arises from neuronal dysfunction within the CNS. The pain generator is not a peripheral nociceptor but a central population of neurons that spontaneously fire—delivering afferent traffic that is perceived as pain. Examples of central pain include spinal cord injury (which is both deafferentation and central), poststroke pain, and pain from a multiple sclerosis plaque.
How could central pain occur in the absence of peripheral tissue injury?
As discussed above, neurons can become more readily depolarized and hence more sensitive because of a number of cellular changes. These include sustained exposure to excitatory transmitters like glutamate and substance P. Such activity may recruit cytokines, prostaglandins, and other inflammatory mediators. Activation of kinases promotes phosphorylation that may change the susceptibility of ion channels to depolarizing current and trigger a cascade to intracellular changes including the production of more sodium or calcium channels.
Nociception without emotional or cognitive/interpretative correlation is not perceived as harmful, disagreeable, or unpleasant, so protective behavior is often nullified.
C-fiber input drives the sensitization process and “wind-up” in the dorsal horn.
Preemptive blockade of nerve impulses quells the neuronal processes that result in sensitization.
Which of the common peripheral neuropathies are often painful?
Examples include the following: diabetic polyneuropathy, diabetic mononeuritis multiplex, diabetic thoracoabdominal polyradiculitis, and the early phase of diabetic amyotrophy. Additionally, uremic neuropathy, ischemic neuropathy, toxic neuropathies such as arsenic poisoning, autoimmune deficiency syndrome (AIDS)-related polyneuropathy, nutritional deficiencies such as thiamine, pyridoxine, and folic acid deficiency.
How would you treat a painful diabetic neuropathy?
Food and Drug Administration-approved drugs such as pregabalin and duloxetine are often employed. There are a large number of off-label anticonvulsants used including gabapentin, oxcarbazepine, valproate, or lacosamine. Tramadol is also effective in some cases. Tricyclic antidepressants can be employed, but the side effect profile is less favorable than that of duloxetine. In more severe cases, an opioid may have to be added to the pharmacologic cocktail.
How would you treat human immunodeficiency virus (HIV) neuropathy?
Make sure the reverse transcriptase inhibitor used to treat the disease is not a provoking cause. Adding B vitamins, duloxetine, or pregabalin are often helpful.
Is there an advantage to using methylated folate and B12 products?
Some individuals have a deficiency in methylene folate reductase activity in the CNS. The use of methylated folate is required to circumvent this problem. Pharmacogenetic testing is available to determine if an individual has this polymorphism (see the pharmacogenetic section of this chapter).
List entrapment neuropathies likely to present with pain.
Carpal tunnel syndrome and ulnar nerve entrapment more commonly result in paresthesia and numbness, but painful symptoms are also quite common. Other entrapments include tarsal tunnel syndrome, lateral femoral cutaneous syndrome, suprascapular nerve entrapment, superior gluteal nerve entrapment, anterior interosseous syndrome, pronator teres syndrome, and radial tunnel syndrome.
How is carpal tunnel syndrome treated?
Mild cases of carpal tunnel syndrome can be treated with a cock-up splint. Some orthopedists inject steroids into the carpal tunnel compartment under ultrasound guidance. More severe entrapment typically requires carpal tunnel release.
How is ulnar entrapment treated?
The ulnar nerve may be entrapped at either the cubital tunnel in the elbow or Guyon’s canal at the wrist. Avoiding pressure on the nerve at the level of the elbow is achieved by keeping the forearm on the volar side and avoiding rubbing the elbow on hard surfaces. Repetitive ulnar deviation and flexion at the wrist aggravates the ulnar nerve at Guyon’s canal. Avoidance of such activities and use of nonsteroidal antiinflammatory drugs (NSAIDs) may help. Sometimes decompressive surgery is necessary.
How is the diagnosis of tarsal tunnel syndrome made?
Clinically, there is pain, dysesthesia, and/or numbness in the medial foot and base of the foot including the big toe and adjacent three toes. The tendon sheath covering the nerve wraps over the medial malleolus down to the calcaneus. The nerve splits into three components, the calcaneal, medial, and lateral plantar nerves. Depending on the location of compression along this tunnel, the heel may be painful along with medial and lateral plantar nerve distribution.
What intervention can be employed to reduce the discomfort of tarsal tunnel syndrome?
Conservative treatment includes steroid injection, physical therapy to mobilize the tibial nerve, and in recalcitrant cases surgery to decompress the tarsal tunnel is necessary.
How do you determine if someone has lateral femoral cutaneous nerve entrapment (a.k.a. meralgia paresthetica)?
Typically, the patient presents with dysesthesia in the anteriolateral aspect of the thigh. There is often exquisite point tenderness at the region where the nerve traverses under the inguinal ligament. This area is at the lateral corner of the ligament near its attachment to the anterior superior iliac spine. Obesity, seatbelt trauma, and diabetes are relatively common causes for this syndrome.
Discuss treatment options for lateral femoral cutaneous entrapment.
Corticosteroid injection near the vicinity of the nerve is often helpful. Weight reduction, if obesity is the source, is helpful. Avoiding recurrent trauma such as compression from a low-lying seatbelt buckle is advised. Surgery is not particularly helpful.
How does a patient with suprascapular nerve entrapment present?
Typically, the patient has deep pain in the posterior shoulder along the muscles of the scapula—namely, supra-and infraspinatus muscles. Weakness in these muscles may occur, and in chronic cases, there may be atrophy. A relatively rare condition, this is increasing in prevalence from the use of backpacks.
How is the above treated?
Steroid injections at the suprascapular notch, where the nerve passes under a ligament, can provide relief, but it may be temporary. Surgical decompression may be necessary.
What is the anterior interosseous syndrome?
This syndrome is caused by entrapment of the anterior interosseous branch of the median nerve. It can be provoked by blunt trauma or repetitive flexion at elbow and wrist such as using an ice pick. The site of entrapment is between the tendinous origins of the pronator teres and the flexor digitorum superficialis. On occasion, it is caused by either a viral or inflammatory process. Symptoms include pain in the forearm and wrist. Easy fatigability and weakness in the distal flexors of the thumb and index finger are often noted. Creating a tight O-ring sign with the thumb and index finger is not possible; instead a flattened, weak pinch is made.
What is the treatment?
Antiinflammatory medications, local steroid/anesthetic injection, pregabalin, gabapentin, duloxetine, or tricyclic antidepressants (TCAs) such as nortriptyline can be tried. If these fail, surgical decompression may be necessary.
What is pronator teres syndrome?
The median nerve is entrapped in the proximal forearm by either the pronator muscle or its fibrous band, the lateral edge of the flexor digitorum superficialis, or the lacertus fibrosus. Symptoms include pain on forced pronation, chronic aching in the forearm, and weakness of the intrinsic muscles of the hand. A positive Tinel’s sign may be elicited at the level of the proximal region of the pronator teres.
What is the treatment?
Pronator teres syndrome is likewise treated conservatively with NSAIDs, TCAs, or pregabalin. If these fail, then steroid injections and surgical exploration if that fails.
What is radial tunnel syndrome?
Radial tunnel syndrome is an entrapment of the posterior interosseous branch of the radial nerve at the proximal forearm. This may be due to an aberrant fibrous band, sharp tendinous margin, or a blood vessel. Symptoms include pain in the proximal and lateral forearm similar to tennis elbow. In fact, it is often mistaken for tennis elbow. It is a rare syndrome, and although tennis elbow is so common, radial tunnel syndrome should still be added to the differential diagnosis. Treatment is similar to the other entrapment syndromes.
Note : Some of the pain syndromes in the above text are not uncommon.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here