Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Neuroblastoma, a tumor of the sympathetic nervous system, is the most common extracranial solid tumor in children. There is broad heterogeneity in the disease course, which can be predicted by clinical staging, tumor histology, and underlying genomic changes. Treatment approaches can vary from observation of spontaneous regression without therapy to extremely intensive, multimodal therapy for the highest risk patients. Low- and intermediate-risk patients generally do well with over 90% overall survival with minimal or no therapeutic intervention . However, 5-year survival for high-risk disease, which makes up approximately half of all newly diagnosed cases , has reached only 50% despite an extensive escalation in therapy intensity and the addition of targeted immunotherapy . In this chapter, we will review the clinical presentation and key molecular features of neuroblastoma, several of which are targets for new therapeutic interventions, and discuss the emerging therapeutic targets from laboratory investigations.
The median age at diagnosis for neuroblastoma is 18 months, with more than 90% of tumors diagnosed before age 10 years . This tumor often presents as an incidentally found abdominal or paraspinal mass, and due to its neuroendocrine origin, arises most often from the adrenal glands and/or the sympathetic ganglia. When symptomatic, neuroblastoma can cause localized symptoms such as abdominal pain and distention, constipation, hypertension, Horner syndrome (presenting as ptosis, miosis, anhidrosis, and enophthalmos when there is involvement of the cervical ganglion), and spinal cord compression. Metastatic neuroblastoma, accounting for nearly half of cases, usually involves the bones and bone marrow and presents with fever, weight loss, bone pain, bruising, bleeding, and pallor. Neuroblastoma is unique, in that, in patients less than 18 months of age, with metastases limited to the skin, liver, or <10% of the bone marrow the disease can spontaneously regress without therapy in more than half of the cases. Other rare and unique presentations of neuroblastoma include hypersecretion of the vasoactive intestinal peptide, which can lead to watery diarrhea and opsoclonus-myoclonus syndrome (OMS). OMS is a paraneoplastic syndrome, thought to be due to antineuronal antibodies to neuroblastoma which cross-react with the normal brain, characterized by opsoclonus, myoclonus, and cerebellar ataxia. Interestingly, although OMS affects 2%–3% of patients with neuroblastoma when it is the initial clinical presentation, 50%–80% of patients with OMS are later found to have neuroblastoma .
Diagnostic workup requires a range of serum and urine laboratory testing, radiographic imaging, and histological assessment of the tumor. Elevated levels of catecholamines, primarily dopamine, homovanillic acid and/or vanillylmandelic acid, are present in the urine in 90% of all patients with neuroblastoma . Complete blood count, prothrombin and partial thromboplastin time, comprehensive metabolic panel (electrolytes, creatinine, uric acid, and liver function panel), ferritin, and lactate dehydrogenase can help assess for end organ dysfunction, elevated turnover or inflammation, and/or identify anemia, thrombocytopenia, and coagulopathy. Imaging should assess the location of the primary tumor as well other potential soft tissue and bony sites of disease and is typically completed with computed tomography (CT) or magnetic resonance imaging (MRI) of the primary site, chest, abdomen, and pelvis, and the head and neck, if clinically involved. MRI is preferred to CT because it reduces exposure to ionizing radiation and produces higher contrast resolution images. Approximately 90% of neuroblastomas are metaiodobenzylguanidine (MIBG) avid, due to expression of the norepinephrine transporter that enables MIBG uptake into tumor cells . Thus, 123 I-MIBG scans, which use MIBG radiolabeled with iodine-123, are essential for the assessment of the metastatic extent of disease with good specificity (90%) and sensitivity (99%) . 18 F-FDG-PET(-CT) scans provide a sensitive although less specific alternative for MIBG nonavid tumors (<10% of cases) or in cases where MIBG is not available. One study reported that two of 24 patients with proven neuroblastoma had negative 123 I-MIBG scans but positive 18 F-FDG-PET(-CT) scans . The sensitivity of 18 F-FDG-PET(-CT) imaging as a single diagnostic test has been reported as 100% versus 92% of 123 I-MIBG (SPECT-CT) scintigraphy although the specificity could not be calculated in this study . Interestingly, high-risk neuroblastoma patients with MIBG nonavid tumors have a better event-free survival (EFS) and overall survival than those with MIBG avid tumors .
Finally, histopathology of the tumor itself is an important part of risk stratification and prognosis. The 1984 Shimada classification combined the histopathologic evaluation of the tumor with patient age and a cellular index of mitosis and karyorrhexis , which the International Neuroblastoma Pathology Committee (INPC) later modified to also include the presence or absence of stromal Schwannian cells .
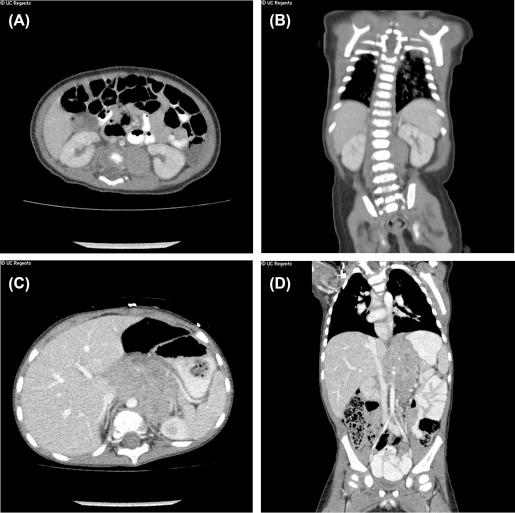
Due to its diverse clinical presentation and course, with some tumors spontaneously regressing, others maturing or differentiating, and others metastasizing, several different staging systems have evolved for neuroblastoma. In order to standardize this process and facilitate the comparison of clinical trials globally, the International Neuroblastoma Staging System (INSS) was developed more than 30 years ago and takes into account the initial extent of surgical resection, with stages 1, 2A/B, 3, 4, and 4S ( Table 14.1 ). Since surgical resection was often deferred in metastatic or very invasive neuroblastoma, a recent international consensus for pretreatment staging was developed in 2004 as the International Neuroblastoma Risk Group (INRG) Staging System (INRGSS), which includes the use of image defined risk factors (IDRFs) rather than surgical resection at diagnosis ( Table 14.2 and Fig. 14.1 ). Image defined risk factors include a detailed list of elements that would make a tumor difficult to completely resect, such as vessel encasement or invasion of an organ or neural foramina ( Table 14.3 ) . Stage L1 tumors are localized and do not involve vital structures as defined by the list of IDRFs. Stage L2 tumors are locoregional with one or more of the 20 described IDRFs. Stage M tumors present with distant metastatic sites of disease. Stage MS is defined as a metastatic disease in patients less than 18 months of age (different from INSS 4s age of <12 months) with involvement confined to the skin, liver, and/or bone marrow only.
| Stage | Description |
|---|---|
| 1 | Localized tumor with complete gross excision, with or without microscopic residual disease; representative ipsilateral lymph nodes negative for tumor microscopically (nodes attached to and removed with the primary tumor may be positive) |
| 2A | Localized tumor with incomplete gross excision; representative ipsilateral nonadherent lymph nodes negative for tumor microscopically |
| 2B | Localized tumor with or without complete gross resection, with ipsilateral noadherent lymph nodes positive for tumor. Enlarged contralateral lymph nodes must be negative microscopically. |
| 3 | Unresectable unilateral tumor infiltrating across the midline, with or without regional lymph node involvement; or localized unilateral tumor with contralateral regional lymph node involvement; or midline tumor with bilateral extension with infiltration (unresectable) or by lymph node involvement |
| 4 | Any primary tumor with dissemination to distant lymph nodes, bone, bone marrow, liver, skin, and/or other organs (except as defined for stage 4S) |
| 4S | Localized primary tumor (as defined for stage 1, 2A, 2B) with dissemination limited to skin, liver, and/or bone marrow a . Limited to infants <1 year. |
a Marrow involvement in stage 4S should be minimal, i.e., <10% of total nucleated cells identified as malignant on bone marrow biopsy or on marrow aspirate. More extensive marrow involvement would be considered to be stage 4. The MIBG (if performed) should be negative in the marrow.
| Stage | Description |
|---|---|
| L1 | Localized tumor not involving vital structures, as defined by IDRFs and confined to one compartment; includes spinal invasion that does not fulfill criteria for IDRF |
| L2 | Loco-regional tumor with one or more IDRFs; ipsilateral tumor that extends over 2 contiguous body parts (i.e., lower chest to upper abdomen) |
| M | Distant metastatic disease (except stage MS); distant lymph nodes and contralateral involvement of 2 body compartments (not including ascites or pleural effusions ± malignant cells) |
| MS | Metastatic disease in children < 18 months (547 days) with involvement of skin, liver, or bone marrow (<10% tumor cells and MIBG scan negative in marrow); primary tumor may be with or without IDRFs (i.e., stage L1 or L2) |
| Ipsilateral Tumor Extension Within Two Body Compartments | Neck-Chest, Chest-Abdomen, Abdomen-Pelvis |
|---|---|
| Neck | Tumor encasing carotid and/or vertebral artery and/or internal jugular vein Tumor extending to base of skull Tumor compressing the trachea |
| Cervico-thoracic junction | Tumor encasing brachial plexus roots Tumor encasing subclavian vessels and/or vertebral and/or carotid artery Tumor compressing the trachea |
| Thorax | Tumor encasing the aorta and/or major branches Tumor compressing the trachea and/or principal bronchi Lower mediastinal tumor, infiltrating the costo-vertebral junction between T9 and T12 |
| Thoraco-abdominal | Tumor encasing the aorta and/or vena cava |
| Abdomen/pelvis | Tumor infiltrating the porta hepatis and/or the hepatoduodenal ligament Tumor encasing branches of the superior mesenteric artery at the mesenteric root Tumor encasing the origin of the coeliac axis, and/or of the superior mesenteric artery Tumor invading one or both renal pedicles Tumor encasing the aorta and/or vena cava Tumor encasing the iliac vessels Pelvic tumor crossing the sciatic notch |
| Intraspinal tumor extension whatever the location provided that: | More than one third of the spinal canal in the axial plane is invaded and/or the perimedullary leptomeningeal spaces are not visible and/or the spinal cord signal is abnormal |
| Infiltration of adjacent organs/structures | Pericardium, diaphragm, kidney, liver, duodeno-pancreatic block, and mesentery |
| Conditions to be recorded, but not considered IDRFs | Multifocal primary tumors Pleural effusion, with or without malignant cells Ascites, with or without malignant cells |
Although amplification of the MYCN oncogene has universally been recognized as an unfavorable prognostic factor since the 1980s , other prognostically significant genomic alterations, histology, and IDRFs need to be consistently integrated into the risk stratification process. Thus, the International Group developed a new risk stratification based on a regression analysis adding to INRGSS and age, the biologic factors of MYCN gene copy number, histology, and segmental chromosome aberrations ( Table 14.4 ) . High-risk features include all patients with metastatic disease 18 months or older at diagnosis, presence of MYCN amplification, unfavorable histology, and segmental chromosome aberrations (stage MS patients >12 months) . Of note, both INSS stage and INRGSS are highly prognostic .
| Stage | Age (mo) | MYCN | INPC | Additional Comments | Segmental Chromosome Aberration | Ploidy | Risk Classification |
|---|---|---|---|---|---|---|---|
| L1 | Any a | Any b | Any | Any | Any | Low | |
| L2 | <18 | NA c | Favorable | Absent | >1 | Intermediate | |
| L2 | <18 | NA | Any | Present | Any | Intermediate | |
| L2 | <18 | NA | Any | Any | D = 1 | Intermediate | |
| L2 | <18 | NA | Unfavorable | Any | Any | Intermediate | |
| L2 | <18 | A | Any | Any | Any | High | |
| L2 | >18 | NA | Favorable | Any | Any | Intermediate | |
| L2 | >18 | NA | Unfavorable | Any | Any | High | |
| L2 | >18 | A | Any | Any | Any | High | |
| L2 | >60 | NA | Unfavorable | Differentiating | Any | Any | Intermediate |
| L2 | >60 | NA | Unfavorable | Poorly differentiating, undifferentiated | Any | Any | High |
| L2 | >60 | A | Any | Any | Any | High | |
| M | <12 | NA | Any | Any | Any | Intermediate | |
| M | <12 | A | Any | Any | Any | High | |
| M | 12–18 | NA | Favorable | Absent | >1 | Intermediate d | |
| M | 12–18 | NA | Any | Present | Any | High | |
| M | 12–18 | NA | Any | Any | D = 1 | High | |
| M | 12–18 | NA | Unfavorable | Any | Any | High | |
| M | 12–18 | A | Any | Any | Any | High | |
| M | >/ = 18 |
Any | Any | Any | Any | High | |
| MS | <12 | NA | Favorable | Absent | D > 1 | Low | |
| MS | <12 | NA | Any | Present | Any | Intermediate | |
| MS | <12 | NA | Any | Any | D = 1 | Intermediate | |
| MS | <12 | NA | Unfavorable | Any | Any | Intermediate | |
| MS | <12 | A | Any | Any | Any | High | |
| MS | 12–18 | NA | Absent | Low | |||
| MS | <18 | NA | Very low | ||||
| MS | 12–<18 | NA | Favorable | Absent | D > 1 | Intermediate d | |
| MS | 12–<18 | NA | Any | Present | Any | High | |
| MS | 12–<18 | NA | Any | Any | D = 1 | High | |
| MS | 12–<18 | NA | Unfavorable | Any | Any | High | |
| MS | 12–<18 | A | Any | Any | Any | High |
a In infants (<12 mo), L1 tumors may be observed without biopsy or surgery for spontaneous regression.
b L1 tumors that are grossly resected are low risk. If not grossly resected with MYCN amplification, they are NOT low risk.
c NA: not amplified; A: amplified.
d M and MS patients between 12 and 18 mo must have all favorable biology to be intermediate risk and otherwise are classified high risk.
Response to therapy is a key element in assessing the achievability of durable remission as well as the risk for recurrence, including bone marrow clearance, and clearance of MIBG-avid lesions during induction chemotherapy . Updated requirements for consistent response assessment by international consensus have recently been published . Recommendations include the assessment of primary and metastatic soft tissue sites using Response Evaluation Criteria in Solid Tumors and semiquantitative scores on MIBG scans (or PET/CT for non-MIBG-avid tumors). Bone marrow should be assessed by histology, or immunohistochemistry and cytology, or immunocytology; and minimal residual disease is classified as <5% tumor involvement . Urine catecholamines are not included in the response criteria as they are not as sensitive as the current radiographic modalities in use.
Future potential biomarkers being studied to improve disease response assessment and possibly predict relapse include mRNA for five neuroblastoma genes ( CHGA, DCX, DDC, PHOX2B , and TH ) in both blood and bone marrow . Marachelian et al. demonstrated that neuroblastoma-mRNA (NB-mRNA) correlated well with current modalities of disease response. When bone marrow morphology MIBG or CT/MRI were positive, NB-mRNA was detected in 99%, 88%, and 81% of bone marrow samples, respectively; it also appeared to be quite specific as it was detected in 55% of samples of patients undergoing therapy for resistant disease and correlated with outcome, even when all three other modalities were negative . This 5-gene TaqMan Low Density Array or TLDA test is being used in clinical trials including biology studies sponsored by the New Approaches to Neuroblastoma Therapy (NANT) consortium. Microarray interrogation of the gene expression profiles of hundreds of neuroblastoma samples was completed by Oberthuer et al., who showed that a 144-gene prediction analysis for microarray (PAM) rivaled current risk stratification methods for patients with contrasting (unfavorable vs. favorable) clinical courses . Circulating tumor DNA (ctDNA) has also been of interest and has been shown to be present in patients without the detection of circulating tumor cells, which suggests two other separate noninvasive biomarkers that may be used to detect and monitor tumors . Given that ctDNA can be used to detect clinically relevant KRAS mutations with a sensitivity of 87.2% and a specificity of 99.2%, it appears to be a useful biomarker not only at diagnosis but possibly at various time points during therapy, to assess clinical response, acquired resistance to therapy, and clonal evolution . In neuroblastoma, serial studies of ctDNA are underway, but thus far, only the detection of a single tumor gene in circulating blood has been reported, such as in detection of an anaplastic lymphoma kinase (ALK) mutation . Furthermore, immunohistochemistry (IHC) is a technique that visualizes antigen-antibody complexes, by typically conjugating the antibody to peroxidase (immunoperoxidase staining) or fluorescein (immunofluorescence). IHC can be useful in identifying tumor cells at diagnosis and relapse as well. Park et al. demonstrate that using neuroendocrine IHC markers such as CD56, chromogranin A, and synaptophysin can be more specific in cases where standard hematoxylin and eosin (H&E) stains are negative . The prognostic impact of staining for MYCN and MYC protein by IHC has also been shown. MYCN protein (+) tumors (associated with MYCN amplification) and MYC protein (+) tumors (without MYCN amplification) had similarly poor outcomes with regard to event-free survival (EFS) and overall survival (OS) ; interestingly, MYC protein (+) expression was statistically significant for predicting poor outcomes independent of other variables including stage, MYCN amplification status, and mitosis-karyorrhexis index . Lastly, microRNAs (miRNAs) are small noncoding RNAs that downregulate translation and have been found to be deregulated in many different cancer types including neuroblastoma , and thus, have recently been studied for their utility as biomarkers or therapeutic targets. MicroRNAs could serve as potential biomarkers for disease, response, and resistance, and given that they appear to be stable in clinical samples (including plasma, serum, and urine), can accurately classify tissue types and disease states, and have been shown to be quickly released from tissues into circulation .
Around 16% of all neuroblastomas and 42%–44% of high-risk neuroblastomas have an amplified MYCN gene. MYCN is a transcription factor oncogene that plays an important role in both healthy and malignant cells with downstream effects promoting sustained growth and survival, cell cycle progression and proliferation, DNA repair and self-renewal, pluripotency, and angiogenesis . MYCN was first discovered in 1983, and it was quickly shown that amplification of MYCN (3–300 copies) strongly correlated with a poor prognosis in neuroblastoma . MYCN can additionally suppress the expression of genes that induce differentiation, halt the cell cycle, regulate immune surveillance, and antagonize metastasis . This prominent role in neuroblastoma biology makes MYCN a tempting therapeutic target, but because it is a transcription factor and not an enzyme, effective clinical targeting of MYCN has, thus far, proven to be challenging.
While MYCN gene amplification is the molecular aberration that is most strongly and consistently a poor prognostic marker, ALK amplification is also associated with inferior outcomes and is present in less than 15% of high-risk neuroblastomas and localized next to MYCN on chromosome 2p . However, ALK is a tyrosine kinase receptor found on the cell surface, and as a highly druggable enzyme, perhaps presents the most immediate molecular target in neuroblastoma. Mosse et al. used whole genome sequencing to identify three separate germline missense mutations in the ALK tyrosine kinase domain for eight separate neuroblastoma pedigrees, implicating germline mutations as the driving mutation for a majority of cases of familial neuroblastoma . Several groups simultaneously reported somatically acquired mutations in the same ALK domain, for 8%–12.4% of high-risk neuroblastoma samples studied that were also predicted to be oncogenic drivers for disease . ALK structure and function are actually relatively well conserved across species, which is how studies of ALK inhibition in zebrafish later demonstrated the cooperation between ALK and MYCN in neuroblastoma tumorigenesis . Genetic alterations of ALK can involve translocations of the ALK locus; however, point mutations, gene amplification or copy number gains, and overexpression (without gene amplification or copy number gains) are typically seen in neuroblastoma . Nonetheless, the two most well-studied fusion proteins that result from translocations involving the ALK locus are the NPM-ALK fusion protein, seen classically in anaplastic large cell lymphomas and non-Hodgkin's lymphoma, and EML4-ALK fusion protein, first reported in non-small-cell lung carcinoma ; both confer constitutive ALK activity and were instrumental in further understanding the downstream pathways and signaling interactions of ALK. Germline gain of function point mutations in ALK are the most common drivers of familial neuroblastoma although nonhereditary high-risk neuroblastomas can have somatic point mutations in ALK, and these mutations are often coexpressed with MYCN amplification, due to similar locations on 2p . Janoueix-Lerosey et al. used genome-wide comparative genomic hybridization analysis on a large sample of neuroblastoma tumors and showed that more than a quarter of neuroblastomas have a copy number increase at the ALK locus and confirmed that mutated ALK does result in constitutive activation of the kinase . George et al. found that one ALK mutation, F1174 L, along with several other variants, could transform interleukin-3 dependent cell lines in murine models of neuroblastoma to cytokine independent growth; these cell lines were subsequently also found to be sensitive to small molecule ALK inhibitors , and thus, demonstrating the rationale for ALK inhibitor therapy in neuroblastoma. Chen et al. similarly reported that most mutations occurred within the kinase domain and identified two hotspots at F1174 and R1275; they demonstrated that NIH3T3 cells expressing mutant ALK showed increased colony formation in soft agar and formed subcutaneous tumors when injected into nude mice, supporting the tumorigenic nature of mutated ALK . Caren et al. identified ALK amplification or in-gene rearrangements in 5% of tumors and mutations in 11% including two more novel point mutations at 3733 and 3735 and further corroborated that ALK mutations and amplifications are found in advanced, higher stage disease with unfavorable features and poor outcome . Downstream signaling of ALK is known to promote cell survival and proliferation and involves the PI3K-AKT, MAPK/ERK, JAK-STAT, and SHH cascades .
In addition to gene amplifications in MYCN and ALK, many segmental chromosome alterations (SCA) have been identified in neuroblastoma that also correlates with an adverse prognosis with decreased EFS and OS. Loss of heterozygosity for chromosome 1p is a known marker of risk, also very often closely linked to MYCN amplification . Aberration of 11q is inversely correlated with MYCN amplification, and is also indicative of a worse outcome . In fact, more recently, any segmental chromosomal aberration has been shown to adversely affect prognosis . DNA content (ploidy) is closely associated with prognosis in an age-dependent fashion, as patients less than 12 months of age with hyperdiploidy (D > 1) have a much higher chance of long-term disease-free survival (>90% of cases) while diploidy or tetraploidy uniformly predict early treatment failure and aggressive disease in patients 12–24 months of age . It has also been demonstrated that unbalanced 17q rearrangements resulting in a partial 17q gain, the most common molecular aberration in neuroblastoma found in >60% of tumors, is also a predictor of poor outcome . Assessing the presence or absence of these other genetic changes is especially helpful in risk stratifying patients who are MYCN nonamplified. Because they are so strongly predictive of outcome, these chromosome gains and losses are also tempting therapeutic targets; however, because many different genes are encoded on any given segmental alteration, choosing which gene product to target is a therapeutic challenge.
The other rare germline mutation with a predisposition to neuroblastoma is PHOX2B, a regulator of neural crest development associated with Hirschsprung's disease and central congenital hypoventilation syndrome, with an autosomal dominant inheritance pattern . However, PHOX2B has not been identified as a common somatic mutation in nonfamilial neuroblastoma.
Genomic surveys of neuroblastoma tumors using whole genome sequencing, for example, have further identified loss-of-function genetic alterations in alpha thalassemia/mental retardation syndrome X-linked (ATRX, more common in adolescent neuroblastoma) gene and telomerase reverse transcriptase (TERT) gene promoter rearrangements that may serve as therapeutic targets . Since the ATRX gene is thought to regulate the expression of other genes via chromatin remodeling, its regulation could impact a broad range of downstream pathways. TERT encodes for telomerase, an enzyme that elongates chromosomes by acting as reverse transcriptase and adding to the telomeres, which are the protective caps on the ends of chromosomes that consist of repetitive TTAAGGG sequences. It has been shown that telomerase activity is primarily absent in most somatic cells except for quickly replicating, mitotically active cells such as skin cells and lymphocytes. Mutations in the TERT promoter typically allow for increased telomerase activity, which results in the elongation of chromosomes with repeated cell replication as opposed to gradual shortening, arrest of cell replication, and replicative senescence . However, as Pugh et al. published, the mutation rate from primary neuroblastoma tumors is quite low at 0.6 mutations per Mb, when compared to adult tumors, and often limited to only a few genes of significance including primarily MYCN, PTPN11, ATRX, ALK, and NRAS .
Lastly, there are several known genes which cause cancer when associated with germline mutations and can predispose to neuroblastoma including TP53, NF1, NRAS, BRCA1, BRCA2, PTPN11, EZH2, and APC . PTPN11 encodes for a protein tyrosine phosphatase that regulates the RAS/MAPK pathway that itself plays a role in cell growth, differentiation, replication, and tumorigenesis. Furthermore, there are several common polymorphisms that may cooperate to lead to sporadic tumorigenesis such as BARD1, LMO1, and LIN28B. B RCA1- A ssociated R ING D omain-1 (BARD1) was first identified as a protein interacting with the N-terminus of BRCA1 . However, it was later shown to not only form a stable complex with BRCA1 but also that it was almost always coexpressed with BRCA1 and cooperated to drive cancer growth . LIM domain only genes 1–4 (LMO1-4) have all been implicated in tumorigenesis, specifically LMO1 and LMO2 in inducing T-cell leukemias; LMO1 itself has been described as a neuroblastoma oncogene since polymorphisms in the gene locus are associated with neuroblastoma susceptibility and tumorigenesis . LIN28B is an RNA binding protein that has an important role in cell growth and metabolism in both normal and cancerous cells and elevated expression has been associated with chronic myelogenous leukemia (CML), T-ALL, hepatocellular carcinoma (HCC), Wilm's tumor, neuroblastoma, and cancers of the colon, prostate, lung, breast, ovary, and cervix . LIN28B has been identified as a driver for high-risk neuroblastoma by not only influencing the expression of the GTP-binding nuclear protein RAN but also by directly binding RAN mRNA and impacting Aurora kinase A activity, which is hypothesized to stabilize MYCN and prevent its degradation . LIN28B furthermore is known to be a key repressor of the let-7 microRNA family, which mediates the differentiation of embryonic stem cells; thus, high LIN28B activity is hypothesized to lead to neuroblastoma tumorigenesis by causing low let-7 activity which subsequently results in a more pluripotent cellular state . Please refer to Table 14.5 for the most pertinent genetic alterations and their associated prognosis in neuroblastoma.
| Genetic Alteration | Prognosis |
|---|---|
| MYCN amplification | Unfavorable |
| Loss of 1p (typically associated with MYCN amplification) | Unfavorable |
| 11q deletion (negatively correlated with MYCN amplification) | Unfavorable |
| Gain of 17q (typically associated with MYCN amplification) | Unfavorable |
| Diploidy/tetraploidy (in patients 12–24 mo) | Unfavorable |
| Hyperdiploidy (in patients <12 mo) | Favorable |
| ATRX mutation | Unfavorable |
| TERT overexpression | Unfavorable |
| NRAS/KRAS mutation | Unfavorable |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here