Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
| Definition and etiology |
|
| Cognitive and behavioral symptoms, in order of prevalence at presentation |
|
| Summary of diagnostic criteria | Primary Criteria for the National Institute of Neurological Disorders and Stroke Consensus Diagnostic Criteria for Traumatic Encephalopathy Syndrome : Components I, II, and III are required. Component IV grades the level of function.
|
| Imaging findings |
|
| Treatment |
|
| Top differential diagnoses |
|
A 63-year-old man presented with progressive memory, concentration, mood, and behavior problems over several years. He was a veteran of the army for six years in his twenties, and reported being “knocked out” or “dazed” more than a dozen times while in combat. In the army he also boxed competitively for several years and frequently had his “bell rung,” although he reported only being knocked unconscious five times. After the army he married and owned a successful small business. For the past 4 to 5 years his wife noted that he became increasingly withdrawn and moody. After making several poor financial decisions he closed down his business. In the last three years he began very uncharacteristic behaviors including yelling and “flying off the handle” over minor issues. His primary care physician referred him to a psychiatrist who prescribed fluoxetine, which improved his mood and anger. Two years ago, his mood and anger worsened, and increasing doses of fluoxetine and other selective serotonin reuptake inhibitors (SSRIs) could not control the symptoms; after an episode of physical aggression toward his wife risperidone was prescribed. In the past year he had clear-cut impairment of his concentration, memory, and function. His wife notes that he now has “no short-term memory” and that he “does nothing” all day long. Neurological examination revealed mild bilateral 3–4 Hz tremor present at rest and with action. He scored 15 on the Montreal Cognitive Assessment (MoCA), making errors on the visuospatial/executive, attention, delayed recall, and orientation sections. Head computed tomography (CT) scan revealed atrophy (most notably in hippocampi and frontal lobes, bilaterally) and a cavum septum pellucidum.
There is increasing evidence that head trauma may be associated with encephalopathy and dementia later in life. The exact pathogenesis of how head trauma at one point in life can cause dementia decades later is complex and is still being determined. We do know that, in addition to causing an encephalopathy that is maximal at the time of the head injury and generally improves (though not necessarily back to baseline), repetitive head injury has been associated with chronic traumatic encephalopathy, a progressive tauopathy with distinctive clinical and pathological features ( ) (see Table 15.1 and Fig. 15.1 ).
| Stage | Pathology | Clinical Symptoms and Signs |
|---|---|---|
| I | Perivascular phospho-tau neurofibrillary tangles in focal epicenters at the depths of the sulci in frontal cortex | Headache, loss of attention and concentration |
| II | Stage I plus neurofibrillary tangles in superficial cortical layers adjacent to the focal epicenters and in the nucleus basalis of Meynert and locus coeruleus | Depression and mood swings, explosivity, loss of attention and concentration, headache, and short-term memory loss |
| III | Stage II plus mild cerebral atrophy, septal abnormalities, ventricular dilatation, concave third ventricle, depigmentation of locus coeruleus and substantia nigra, dense phospho-tau pathology in the cortex, medial temporal lobe, diencephalon, brainstem, and spinal cord | Cognitive impairment with memory loss, executive dysfunction, loss of attention and concentration, depression, explosivity, and visuospatial abnormalities |
| IV | Stage III plus further cerebral, medial temporal lobe, hypothalamic, thalamic, and mammillary body atrophy, septal abnormalities, ventricular dilatation, and pallor of substantia nigra and locus coeruleus; phospho-tau in widespread regions including white matter, with prominent neuronal loss, gliosis of cortex, and hippocampal sclerosis | Dementia with profound short-term memory loss, executive dysfunction, attention and concentration loss, explosivity, and aggression. Most also show paranoia, depression, impulsivity, and visuospatial abnormalities. Many also have parkinsonism, speech, and gait abnormalities |
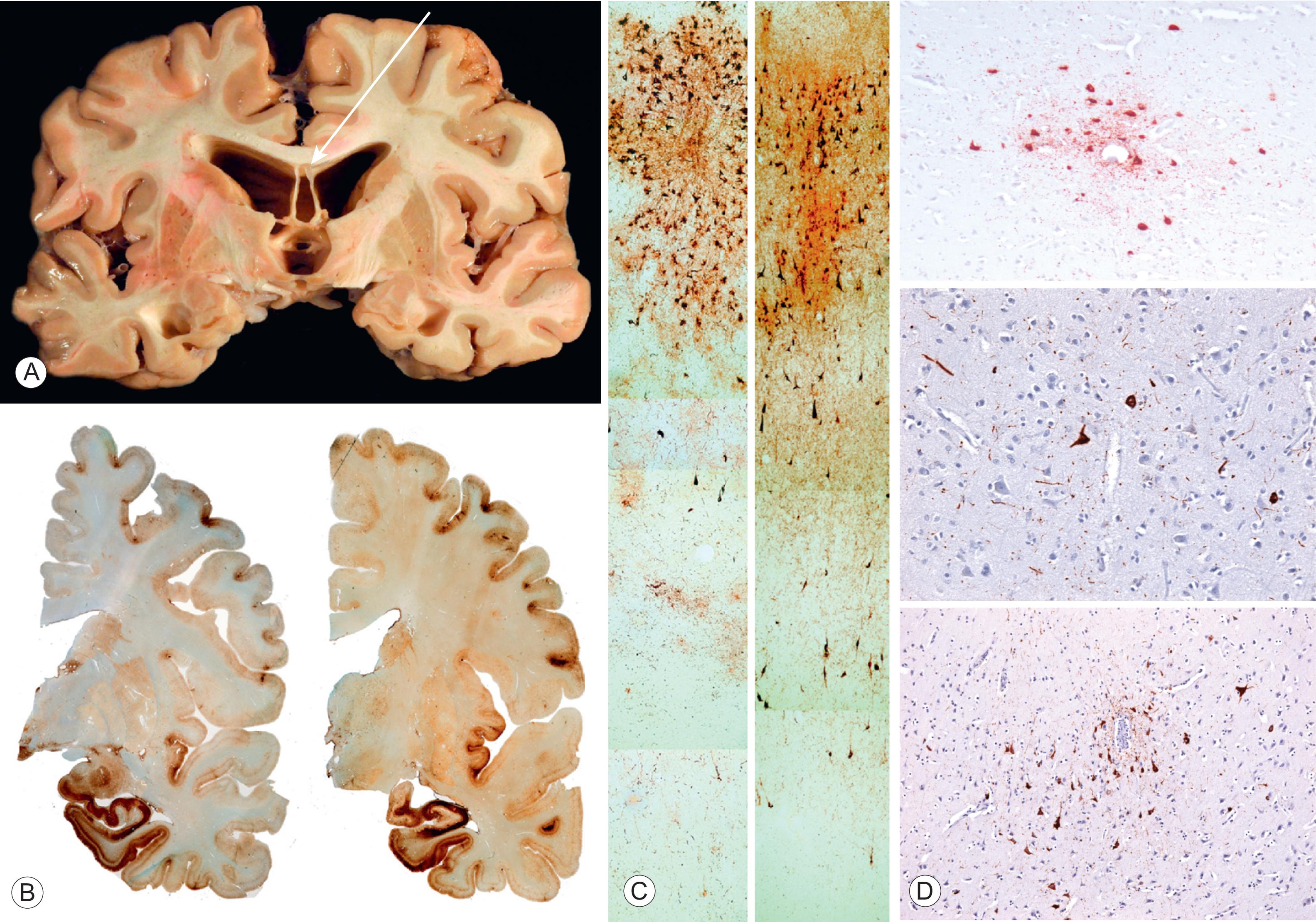
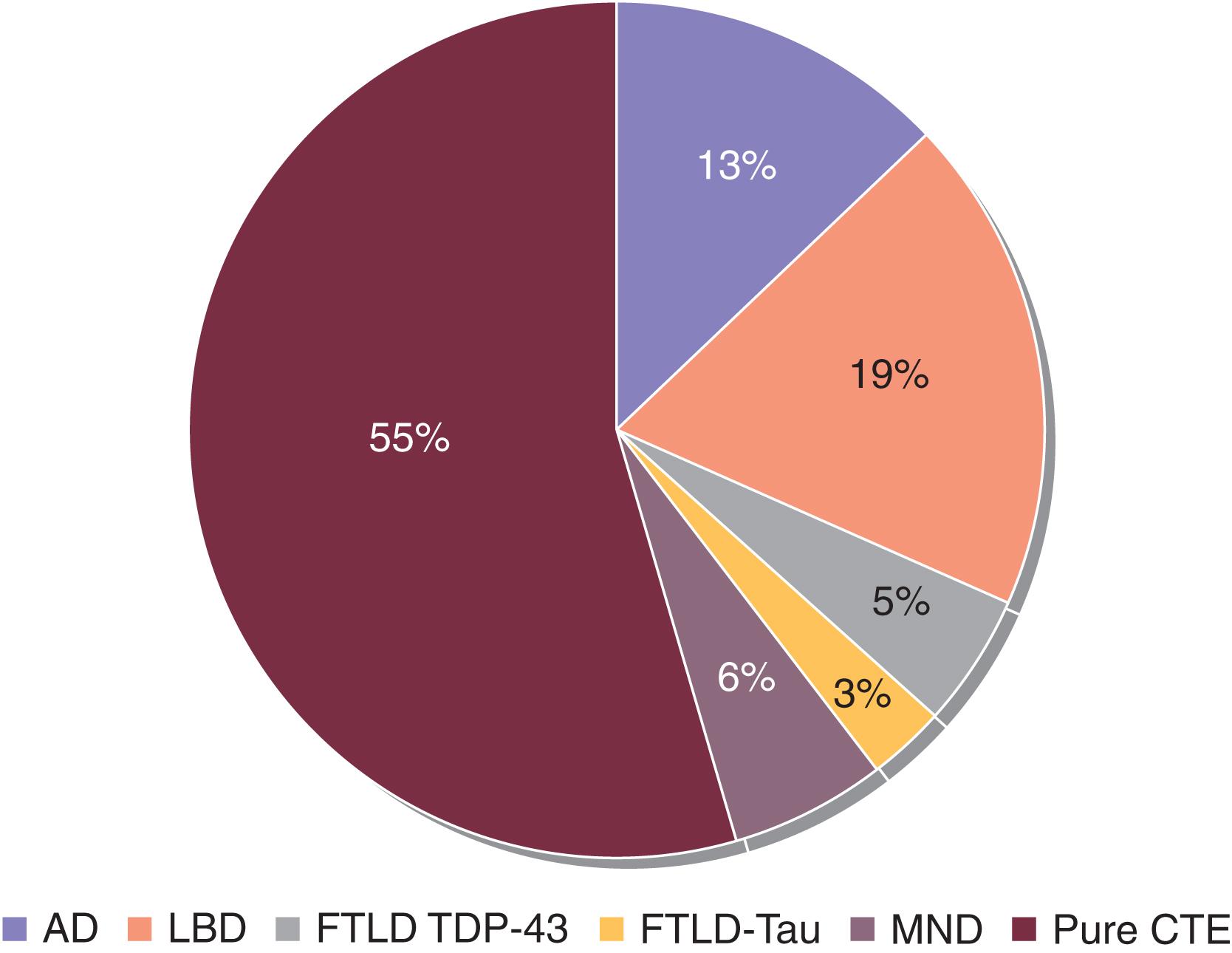
In one series McKee and colleagues analyzed the brains of 85 individuals with a history of repetitive mild traumatic brain injury and found evidence of chronic traumatic encephalopathy (CTE) in 68 (80%) of them, including 64 athletes, 21 military veterans (most of whom were also athletes), and one individual with self-injurious head-banging behavior. The athletes included those who played football, hockey, boxing, rugby, soccer, and wrestling; the veterans included those who fought in World War II, Vietnam, Gulf War, Iraq, and Afghanistan ( ). Another series showed that multiple pathologies are common; of 177 football players who came to autopsy, 55% had pure chronic traumatic encephalopathy and 45% had additional pathologies, the most common being Lewy body disease (19%) ( Fig. 15.2 ) ( ). CTE has also been observed in individuals who regularly engaged in bull riding and mixed martial arts. Because of the selection bias of cases referred to autopsy, the exact prevalence of chronic traumatic encephalopathy in athletes, veterans, and the general population is unknown. Three studies of American professional football players, each with more than 1000 subjects, have found the risk of all types of neurodegenerative disease between three and five times greater than that of the general United States population ( ).
Katz and colleagues have developed research criteria for traumatic encephalopathy syndrome ( ). See the Quick Start for a summary of the primary criteria and Box 15.1 for an abbreviated version of the primary criteria.
Components I, II, and III are required. Component IV grades the level of function.
Substantial Exposure to Repetitive Head Impacts
Impacts may or may not have been associated with concussion or traumatic brain injury (TBI). Examples include:
Involvement in ‘high exposure’ contact or collision sports such as boxing, American football, ice hockey, soccer, rugby, professional wrestling, mixed martial arts, as well as others.
For American football, minimum of 5 years organized play is required, including 2 or more years at the high school level or beyond.
Exposure risk thresholds for other contact or collision sports should involve a substantial number of years, such as 5 or more.
Military service involving repetitive head impacts, including combat exposure to multiple blast and other explosions, non-combat exposure to explosions (including blasting and forced opening of lock doors), or multiple blows to the head over an extended period of time (such as repeated blows with a padded military training weapon).
Other sources involving multiple head impacts over an extended time including domestic/intimate partner violence, head banging, and vocational activities such as breaching locked doors and other barriers by first responders.
Cognitive Impairment or Neurobehavioral Dysregulation or both, plus a progressive course
Cognitive Impairment (all 4 are required)
As reported by self or informant, or by clinician’s report.
Representing a significant decline from baseline functioning.
With deficits in episodic memory and/or executive functioning (+/- additional domains).
Substantiated by impaired performance:
At least 1.5 standard deviations below appropriate norms on formal neuropsychological testing.
If formal neuropsychological testing is not available, substantial evidence of impairment below a person’s estimated baseline in episodic memory and/or executive functioning on a standardized mental status examination (e.g., Montreal Cognitive Assessment [MoCA], Mini-Mental State Examination [MMSE]) by a clinician experienced in the evaluation of cognition.
Neurobehavioral Dysregulation (all 3 are required)
As reported by self or informant, or by clinician’s report.
Representing a significant change from baseline functioning.
With symptoms and/or observed behaviors representing poor regulation or control of emotions and/or behavior, including explosiveness, impulsivity, rage, violent outbursts, “short fuse,” or emotional lability.
Preferably substantiated by standardized measures.
Not from a transient response to life events, e.g., divorce, death of loved one, financial problems.
Progressive Course
Progressive worsening of these clinical features over at least 1 year in the absence of continued repetitive head impacts or TBI. Supported by:
Serial standardized testing (if available), or
Clear history supporting a change in functioning over time (e.g., clinician reports, job performance evaluations, or self- or informant-report).
Not Fully Accounted for by Other Disorders
The pattern of the cognitive deficits is not fully accounted for by other pre-existing, established, or acquired non-degenerative nervous system, medical, or psychiatric disorders and conditions.
The Core Clinical Feature of Neurobehavioral Dysregulation , if present, is not fully accounted for by other pre-existing, established, or acquired non-degenerative nervous system, medical, or psychiatric disorders and conditions.
Comorbid diagnosis of another neurodegenerative disease does not exclude a TES diagnosis.
However, TES may be excluded if the clinical features and any available biomarkers are fully accounted for by another neurodegenerative disorder.
Comorbid diagnosis of substance use disorder, posttraumatic stress disorder (PTSD), mood or anxiety disorders , or a combination of these, can be present and do not exclude a TES diagnosis, unless they are determined to account for all Core Clinical Features.
Level of Functional Dependence/Dementia
The level of functional dependence should be based on the impact of Cognitive Impairment and/or Neurobehavioral Dysregulation and not on physical limitations or medical illness.
Independent . Independent at usual level in job, household responsibilities, or family, social, and community roles. Able to engage in hobbies and intellectual activities at usual levels; fully independent instrumental and basic activities of daily living (ADLs, see Box 2.2 ).
Subtle/Mild Functional Limitation . Slightly reduced performance in job, household responsibilities, or family, social and community roles; slight problems in hobbies and intellectual interests reported; mostly independent but may be more challenged in some instrumental ADLs and fully independent in basic ADLs.
Mild Dementia . Definite impairment of instrumental ADLs; may be engaged in some home, family, social, and community activities; more difficult activities abandoned; needs cues for some basic ADLs.
Moderate Dementia . Not independent but can be taken to some functions outside the home; only simple chores preserved; very restricted interests; needs assistance with basic ADLs.
Severe Dementia . Cannot participate in functions outside the home; no significant function in home; impaired basic ADLs; not independent with self-care; frequently incontinent.
have defined four pathological stages of chronic traumatic encephalopathy and the common symptoms and signs associated with each ( Table 15.1 ). There has also been the recognition that there are two common clinical presentations of chronic traumatic encephalopathy ( Box 15.1 ; ; ):
A behavioral/mood variant whose initial features develop at a younger age with behavioral and/or mood disturbance, and
A cognitive variant whose initial features develop at an older age and involve more cognitive impairment.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here