Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Talking with the family (or other caregivers) is critical to obtaining an accurate history.
Important elements of the history to investigate include:
Characterization of the onset and course of the disorder
Memory loss and memory distortions
Word-finding
Fluctuations in attention
Getting lost in a new or familiar environment
Problems with reasoning and judgment
Changes in behavior
Depression and anxiety
Loss of insight
Current functional status including basic and instrumental activities of daily living.
Review of systems, past medical history, physical examination, and laboratory studies should evaluate for medical, neurological, and psychiatric problems that can impair cognition and memory, such as strokes, Parkinson’s disease, and depression.
Cognitive testing is essential, whether with brief tests in the office or a formal neuropsychological evaluation.
Interpret current cognition and function in light of the patient’s previous abilities.
Routine screening for memory loss will allow patients to be diagnosed and treated earlier, which can help them to delay a decline in function and maintain quality of life.
A brain CT or MRI scan is essential for evaluating possible strokes and other anatomic lesions.
A functional imaging scan (technetium SPECT or fluorodeoxyglucose PET) can be helpful to confirm the diagnosis of an atypical dementia and to provide additional diagnostic information for young patients.
A lumbar puncture, amyloid PET scan, or tau PET scan can confirm the diagnosis of Alzheimer’s disease with a high degree of certainty.
Beware of diagnosing dementia in the patient hospitalized for a medical issue!
In this chapter we will discuss how to evaluate a patient with memory loss and possible dementia, including the history, physical examination, cognitive testing, and laboratory and imaging studies. We will illustrate this evaluation by focusing on the most common cause of memory loss, Alzheimer’s disease. Elements of the evaluation are similar to other medical assessments and should include:
a history of present illness
medical history
current and relevant past medications
allergies to medications
social history, including education, occupation, and any possible learning disabilities
family history, including a history of late-life memory problems even if considered normal for age at that time
physical and neurological examination
cognitive examination
laboratory studies
neuroimaging studies.
One aspect of the evaluation that is both critically important and different from most other appointments is the need to speak with a family member or other caregiver. The family or caregiver must be interviewed to obtain an accurate history. Commonly, patients with memory loss truly do not remember the various instances in which they forget things. Or patients may remember at least some of these instances, but are reluctant to share them with the clinician. This reluctance may stem from a variety of issues. Often patients find it frightening to admit—even to themselves—that they have memory problems, because in our society the label of “Alzheimer’s disease” has become tantamount to what cancer was 30 years ago: synonymous with a death sentence. Sometimes patients do not want to admit their memory problems to the clinician or their families, for fear that, at best, they will be condescended to and, at worst, they will be sent to a nursing home.
Ideally, family or other caregivers are interviewed separately from the patient. Family members are often reluctant to give a full, accurate, and detailed history to the clinician in the presence of the patient. Sometimes this reluctance is present because the history includes inappropriate sexual behavior, aggression, poor driving, or other sensitive subjects that families prefer to discuss in private. More often the reluctance is present because patients will often deny that they have memory problems for the reasons mentioned above. Some patients may become upset when confronted by what they view as accusations leveled against them by their family. Other patients may become visibly depressed. Even if family members begin to give an accurate history in front of the patient, they usually stop when they see their loved one becoming angry or depressed. In addition, family members quite correctly view it as impolite to discuss the patient in front of him or her as if they were not there. Lastly, talking in private can provide a comfortable atmosphere for the family or caregiver to discuss the patient candidly.
There are many different ways to successfully set up a clinic appointment to evaluate the patient with memory loss. The part of the evaluation that is different from many others is the opportunity to speak with the family, preferably alone ( Table 2.1 ). Because this takes time, the evaluation is often best divided into two or even three visits.
| Medical Evaluation | Dementia Evaluation |
|---|---|
| Self-history important | Self-history can be unreliable |
| Family observations secondary | Family observations critical |
| Mental status examination can be deferred | Mental status examination critical |
| Laboratory studies often critical for diagnosis | Most laboratory studies are exclusionary, not diagnostic |
| Imaging studies may not be needed | Imaging studies critical |
Another reason to divide the evaluation into separate visits is that time is necessary to build up a rapport with patients and families. When patients come to the clinic for an initial visit with laboratory studies and scans already completed and the diagnosis clear, it would seem logical to provide the diagnosis in that visit. However, we would not recommend doing this. It is our experience that many patients and families are simply not prepared to hear a diagnosis of Alzheimer’s or another dementia from a clinician they have just met. Although it will still be emotionally difficult for patients and families, it is better to invite the patient back to the clinic to discuss the diagnosis and treatment plan on another day. In the initial visit, the patients quite correctly perceive that they are seeing “a new doctor.” Upon returning to the clinic on a later day, many patients will now feel that they are seeing “one of their doctors.”
In our memory clinics we have the opportunity to have the patient perform cognitive testing with a member of the clinic staff, and it is during this time that we typically talk with the family alone. On occasions when the patient would not have testing with a member of the clinic staff, we will often simply ask the patient to sit in the waiting room for a few minutes while we speak with the family. There are, however, many other opportunities to speak with a family member alone. For example, in the busy internal medicine practice of one of our colleagues, when she is worried that a patient of hers is having memory problems, she will talk with the family member for a few minutes in a spare examination room while the patient is changing into a gown. Calling the family member on the phone at a different time is, of course, another option, and a necessary one if the family member did not accompany the patient. If a patient does not have a close family member (or one that they want contacted), talking with a close friend is a good substitute. For those patients who are still working, talking with an employer can sometimes be helpful, particularly if difficulties at work are the main issue. One must be careful, however, to maintain patient confidentiality when talking with any of these individuals, but particularly when talking with friends and employers.
In all cases we believe it is important to begin by describing to the patient and the family what is going to happen in the appointment, and what the follow-up will be. Here is one example of a typical preamble that might be used by a clinician, in this case a neurologist:
Hi, Mr. Jones, I hear there are some concerns about your memory. Let me begin by telling you how I like to do my memory evaluations. I want to start by talking with you, to find out what problems you have noticed, if any, with your thinking and memory. We will then go over your medical history, medications, family history, and other things like that. I am glad that you brought your family with you—I’m going to ask for their help when we go over your medical history, etc., so that I don’t miss anything. We’ll then do a physical and neurologic exam: listen to your heart and lungs, tap on your reflexes, that sort of thing. Next, we’ll decide what blood work and CT or MRI scans need to be performed. Then you’re going to spend some time with my assistant, who will give you some paper and pencil tests of your thinking and memory. While you’re doing that, I’ll spend a couple of minutes chatting with your family to get their perspective on your thinking and memory difficulties, if that is OK with you. That will be what we’ll have time to do today, and then when I see you back in our next appointment we’ll go over the results of all these tests, and make a plan of what to do to try to improve your memory. How does all that sound to you?
Here is another example, one that might better fit a busy internist’s practice for an existing patient:
Hi, Mr. Jones, your wife is worried that you are having a bit of difficulty with your memory. While it may be part of normal aging, I don’t want to miss any treatable diseases. To find out if there is anything going on—besides the fact that you’re getting a bit older—I want to start by talking with you, to find out what problems you have noticed, if any, with your thinking and memory. We will then briefly review your medical history, medications, family history, and other things like that. We’ll then do a physical exam. Next week I’d like you to come back to the office. At that visit I’ll chat privately with your wife for a few minutes, if that is OK with you, to get her perspective on things. We’ll also do a few minutes’ pencil and paper tests to see how your thinking and memory are doing. Finally, we’ll decide what blood work needs to be done, and we may get a CT or MRI scan to take a look at your brain. When I see you back next month we’ll go over the results of all these tests, and see what we can do to improve your memory. How does all that sound to you?
Sometimes an evaluation of memory loss takes place in the inpatient setting of a hospital. Some things are much easier to accomplish in the hospital, and others are more difficult. It is usually easier to find time to speak with a family member, and it may also be easier to have laboratory and imaging studies completed in the hospital. It is more difficult, however, to see patients at their cognitive best. Often, the hospital setting alone will make a patient disoriented and confused, even aside from the illness or procedure that they are in the hospital for. Because of this, being in the hospital is a fine place to begin an evaluation of memory loss, but the evaluation must include an outpatient visit so that the clinician has the opportunity to see the patient at their cognitive best. Beware of diagnosing patients with memory loss or dementia having seen them only in the inpatient setting!
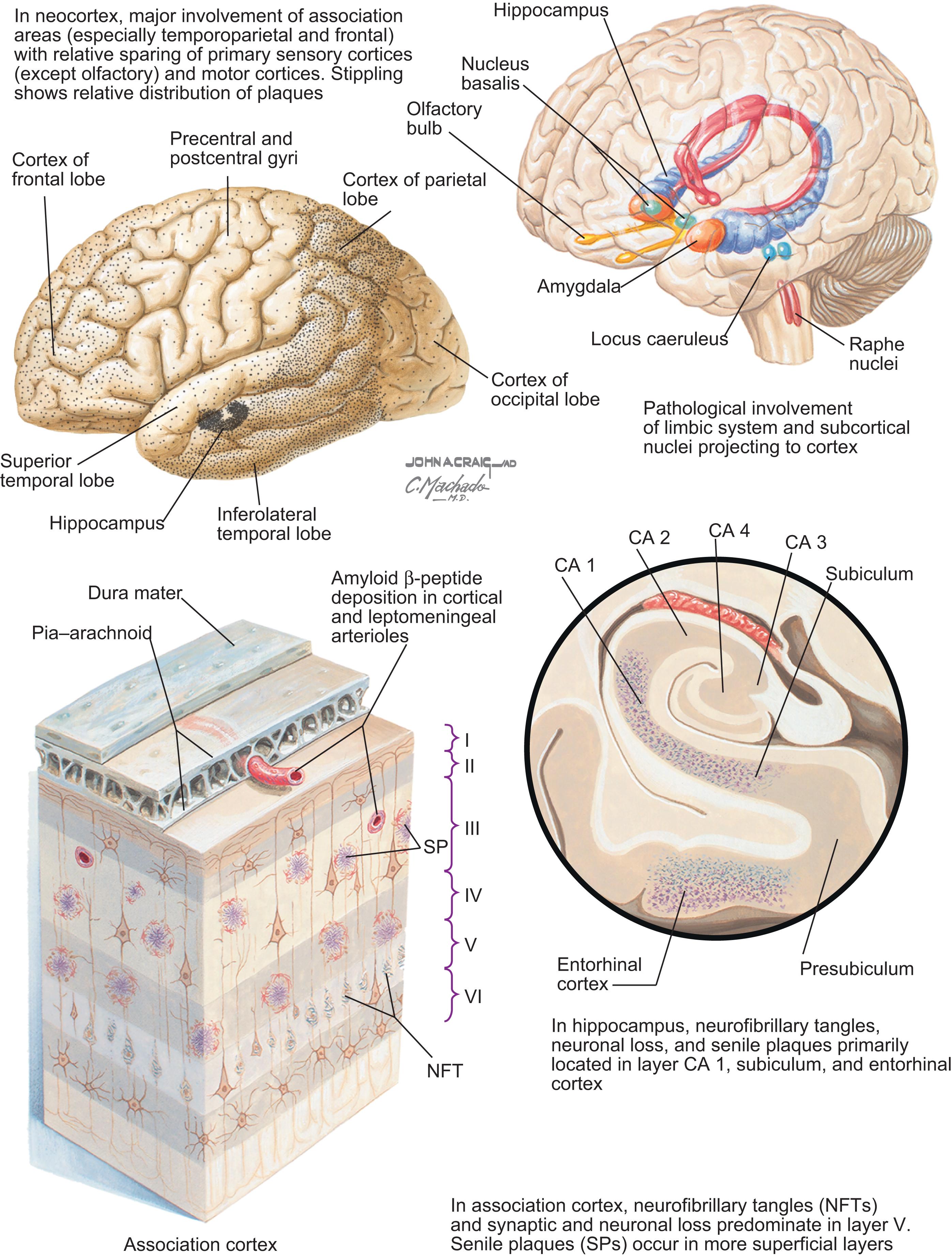
One of the keys to understanding the history of signs and symptoms in a patient with Alzheimer’s disease is to understand the relative timing and distribution of Alzheimer’s pathology in the brain. Alzheimer’s pathology has a predilection for a number of particular regions of the brain ( Fig. 2.1 ). These regions include the hippocampus and amygdala, as well as the parietal, temporal, and frontal lobes. Alzheimer’s pathology also affects subcortical nuclei that project to the cortex, such as the basal forebrain cholinergic nuclei (which produce acetylcholine), the locus coeruleus (which produces norepinephrine), the raphe nuclei (which produce serotonin), and certain nuclei of the thalamus. Damage to particular regions leads to particular signs and symptoms ( Box 2.1 and Table 2.2 ).
Rapid forgetting
Repeats questions and stories
Loses items
Puts items in wrong place
Memory distortions
Word-finding difficulties
Pauses in sentences
Family members automatically filling in for missing words
Word substitutions, either wrong word or a simpler word for a more complex one
Difficulty learning a new route
Becomes confused or lost in familiar places
Makes poor decisions
Difficulty planning and/or carrying out activities such as a simple repair or preparing a meal
Apathy
Depression
Anxiety
Irritability
Delusions such as people are in the house or stealing money
| Cognitive Domain | Examples of Symptoms or Observations | Examples of Assessments |
|---|---|---|
| Complex attention (sustained attention, divided attention, selective attention, processing speed) |
|
|
| Executive function (planning, decision making, working memory, responding to feedback/error correction, overriding habits/inhibition, mental flexibility) |
|
|
| Learning and memory (immediate memory, recent memory [including free recall, cued recall, and recognition memory], very-long-term memory [semantic; autobiographical], implicit learning) |
|
|
| Language (expressive language [including naming, word-finding, fluency, and grammar and syntax] and receptive language) |
|
|
| Perceptual-motor (includes abilities subsumed under the terms visual perception, visuoconstructional, perceptual-motor, praxis , and gnosis ) |
|
|
| Social cognition (recognition of emotions, theory of mind) |
|
|
The hippocampus and other medial temporal lobe structures are the earliest and most severely affected brain regions in Alzheimer’s disease. The hippocampus is the brain structure that is most directly responsible for learning of new personal experiences, such as remembering a short story or what you had for dinner the previous night. This type of memory is usually referred to as episodic memory because it is memory for a specific episode of your life (see Appendix C ). Thus impairment of episodic memory is usually one of the earliest signs of Alzheimer’s disease.
Common symptoms of this memory loss include asking the same questions repeatedly, repeating the same stories, forgetting important appointments, and leaving the stove on. The memory disorder of Alzheimer’s disease, like other disorders of episodic memory, follows a particular pattern identified by Ribot in 1881 ( ). Following Ribot’s law, the patients show anterograde amnesia or difficulty learning new information. They also show retrograde amnesia or difficulty retrieving previously learned information. However, the patients typically demonstrate preserved memory for remote information. Thus a patient may report, “I’ve got short-term memory problems—I cannot remember what I did yesterday but I can still remember things from thirty years ago.” Not understanding that this pattern is suggestive of the memory impairment common in Alzheimer’s disease, family members may report that they feel confident that—whatever the patient’s problem is—it “isn’t Alzheimer’s disease,” because the patient can still remember what happened many years ago. The memory deficits experienced by patients with Alzheimer’s disease are often referred to as rapid forgetting of information they have recently learned.
In addition to rapid forgetting, patients with Alzheimer’s disease also experience distortions of memory and false memories ( ). These distortions may include falsely remembering that they have already turned off the stove or taken their medications, leading patients to neglect performing these tasks. More dramatic distortions of memory may occur when patients substitute one person in a memory for another, combine two memories together, or think that an event that happened long ago occurred recently. Sometimes a false memory can be confused with a psychotic delusion or hallucination. For example, a patient may claim to have recently seen and spoken with a long-deceased family member. This patient is much more likely to be suffering from a memory distortion or a false memory than a true hallucination. The same is true for the patient who claims that people are breaking into the house and moving things around. That these symptoms likely represent memory distortions—rather than true hallucinations or delusions—has implications when the time comes for treatment, as memory distortions are best treated with memory-enhancing medications (such as cholinesterase inhibitors) rather than antipsychotic medications. (A true hallucination, on the other hand, may suggest dementia with Lewy bodies rather than Alzheimer’s disease; see Chapter 8 .)
After memory loss, difficulty finding words (often referred to as an anomia) is one of the most common symptoms of Alzheimer’s disease. There are several areas of the brain that are critical for word-finding, the majority of which are affected by Alzheimer’s disease. There is evidence to suggest that the lower, lateral portion of the temporal lobes is involved in the representations of words and their meanings ( ). This part of the brain is involved in our general store of conceptual and factual knowledge, such as the color of a lion or the first president of the United States, which is not related to any specific memory (see the section on semantic memory in Appendix C ). The frontal lobes, by contrast, are thought to be involved in the selection or choice of the particular word that is searched for ( ). Both the inferolateral temporal lobes and the frontal lobes are affected by the pathology of Alzheimer’s disease ( ) (see Fig. 2.1 ).
Word-finding difficulties manifest in several different ways in patients with Alzheimer’s disease. Frequently, patients will substitute a simpler word for a more complex one or they may be unable to complete sentences. Sometimes there will be circumlocutions, in which patients will describe the word because they cannot retrieve it. For example, the patient may say, “He went to the place where they sell the food,” referring to the grocery store. Some patients will refer to missing words by using generic terms, such as “Bring me the whatchamacallit” or “use the thing if you’re going to do that.” Family members become accustomed to filling in missing words. As the disease progresses, word substitutions (often referred to as paraphasic errors) occur. These word substitutions are typically not random, but instead are usually related to the word by meaning (often referred to as semantic paraphasic errors) or sound (often referred to as phonemic paraphasic errors). For example, the patient who meant to say “Are we going in the boat?” may instead say either “Are we going in the car?” or “Are we going in the coat?” Sometimes the speech is fluent, but is relatively uninformative (often called empty speech ). For example, when asked what he or she did before retiring, the patient may respond, “I worked at my job,” rather than mentioning a specific company or occupation. As the disease progresses, speech may remain fluent, but almost devoid of content. For example, a patient attempting to describe what they did yesterday might say, “I went with them to the thing over there.”
The parietal lobe is another region of the brain affected very early by Alzheimer’s disease. The parietal lobe is involved in spatial function, and is particularly important for real-time spatial navigation, such as when walking or driving ( ). It is, in part, because of the parietal involvement in Alzheimer’s disease that patients with the disorder often make wrong turns and become lost or confused. These difficulties occur even when traveling familiar routes, and patients with Alzheimer’s disease have great difficulty planning new routes. Families often report that they suspected something was wrong when the patient became lost in an airport, couldn’t find the way to a new place, or had to search the restaurant to find the right table after using the restroom. Later, the patient may become lost when going to a familiar location. For example, a patient we have cared for was trying to go to her doctor’s office, a location that she had been to frequently for many years. Although it was only 20 minutes away in a neighboring town, she spent over 7 hours trying to find the office, driving through many towns that were far from the office. She ultimately gave up and went home.
Alzheimer’s disease affects the frontal lobes, specifically the prefrontal cortex. This part of the frontal lobes is involved in many aspects of brain functioning, including problem solving, abstraction, reasoning, and judgment. These cognitive abilities are sometimes collectively referred to as executive function . The frontal lobes are also critical for attention, concentration, and working memory—the ability to temporarily maintain and manipulate information (see Appendix C for details).
Patients with Alzheimer’s disease manifest difficulties in these areas in several different ways. Difficulties with complex tasks such as paying bills and balancing a checkbook occur frequently. They may be unable to perform tasks requiring even simple reasoning that would have been easy for them previously. For example, an electrical engineer may be unable to connect a DVD player to a television, and a gourmet cook may be unable to make anything but the simplest meals. They may also have difficulty planning and organizing a task, such as a household repair or Thanksgiving dinner.
In addition to reasoning, judgment, and attention, the frontal lobes are involved in the control of behavior, as well as personality and affect. The amygdala, a small brain structure in the anterior medial temporal lobe, is affected by Alzheimer’s pathology early in the course of the disease and is involved in regulation of behavior and affect. Over 80% of individuals diagnosed with Alzheimer’s disease experience a change in behavior and affect at some point in the disease; these changes often occur early in the disease course and progress with the disease. Although how these changes manifest is somewhat variable; apathy is the most common behavioral change early in the disease, followed by irritability. As the disease progresses, many patients show an exacerbation of their previous personality characteristics. A person who was always competitive may become aggressive, whereas a person who was a wallflower may stop initiating conversation entirely. Sometimes patients exhibit more dramatic changes in personality, as when someone who was previously aggressive becomes passive, or vice versa. In general, however, the personality changes in Alzheimer’s disease are relatively mild. Although the patient may be acting in a more aggressive or more passive manner than usual, family members still think of the patient as their “father” or “husband” acting differently, rather than as a completely different person (in contrast to many patients with behavioral variant frontotemporal dementia, see Chapter 10 ). Often these mild personality changes will not be apparent during the formal office evaluation or even in brief social settings. One good rule of thumb is that the patient with mild Alzheimer’s disease can appear normal at a cocktail party for 5 minutes, and can “pull it together” in a doctor’s office and behave normally during an evaluation. Because of this fact, it is important to discuss changes in behavior and personality during the interview with a family member or friend.
Several symptoms often result from the combination of frontal lobe dysfunction in conjunction with cognitive loss. Apathy and disinterest are two such symptoms. For example, an avid reader may not be able to remember enough of a book to enjoy it. A builder of model ships may no longer possess the attention, spatial, and problem-solving skills necessary to put together a model consisting of several hundred parts. Suspiciousness and paranoia are two other common symptoms that may result from frontal lobe dysfunction in conjunction with cognitive dysfunction. The usual scenario is that the patient puts their valuables away in a safe place so that they cannot be stolen, forgets where they put them, and then is certain that they have been stolen—only to be found later.
Depression and anxiety are extremely common in the earliest stages of Alzheimer’s disease ( ). These symptoms are understandable, because there are few things as depressing and anxiety-provoking as realizing that one has memory loss or worrying that one has Alzheimer’s disease. It has long been thought that depression is a common cause of memory problems. Although it is true that individuals with depression will often complain of memory problems, it has been our experience that it is more likely that patients with memory complaints in addition to depression or anxiety will have an underlying primary memory disorder, such as Alzheimer’s disease. We discuss the relationship between depression and Alzheimer’s disease in Chapter 17 .
An older rule of thumb that some clinicians have used is that if the patient complains of memory problems then he or she does not have a memory disorder; it is the patient who denies memory problems who has Alzheimer’s disease or another dementia. This rule of thumb brings up the issue of insight. Commonly, patients in the very early stages of Alzheimer’s disease—particularly those with the pre-dementia stage of mild cognitive impairment (MCI) (see Chapter 3, Chapter 4 for details)—show insight into their memory deficits ( ). Occasionally, even patients with moderate Alzheimer’s disease dementia demonstrate some preserved insight. In our experience younger patients, regardless of their disease stage, are more likely than older patients to demonstrate insight into their difficulties. Presumably this is attributable to younger patients having better preserved frontal lobe function than older patients. Thus many patients in the very earliest stage of Alzheimer’s disease are aware of and complain about their memory difficulties.
Understanding the patient’s ability to function is critical in any evaluation of memory loss or dementia. Part of the definition of dementia is that the patient has had a noticeable decline from their prior level of functioning. For mildly affected patients, we often ask about their ability to organize and prepare meals (both simple and more involved for holiday gatherings), do volunteer or other work, pay bills, balance their checkbook, and go grocery shopping. For the more impaired patients we often ask about being able to take their medications independently, whether there is any wandering from the house, and whether there are any difficulties with bathing, dressing, and toileting. One good method of evaluating patients’ level of function is to determine how they are doing in their basic and instrumental activities of daily living ( Box 2.2 ).
Knowing if a patient has difficulties with instrumental and/or basic activities of daily living is one way to quickly understand how much function the patient does and does not have. (See the section below in this chapter, Evaluating Function , for additional information.)
Bathing
Dressing and undressing
Eating
Transferring from bed to chair and back
Walking
Control of bowel and bladder
Using the toilet
Light housework
Preparing meals
Taking medications
Shopping for groceries and clothes
Using the telephone
Managing money and paying bills
As with any disorder, it is important that the clinician conducts a review of systems that includes signs and symptoms of disorders in the differential diagnosis of memory loss. Ask about whether the following have ever occurred:
A significant brain infection, such as meningitis or encephalitis
A significant head injury in which the patient lost consciousness
Repetitive mild head injuries from football, other sports, or other causes
A stroke or a transient ischemic attack
A seizure
Fluctuating levels of alertness or periods of being relatively unresponsive
Visual hallucinations of people or animals
A disturbance of gait
Falls
A tremor
Rigidity and other signs of parkinsonism
A dramatic change in personality such that the patient seems like a different person
Any major psychiatric problems earlier in life, such as major depression or bipolar disease
Any weakness or numbness in the face or of an arm or a leg
Problems with fevers, chills, or night sweats
Problems with nausea, vomiting, or diarrhea
Problems with chest pain or shortness of breath
Any incontinence of bowel or bladder
Problems going to sleep (insomnia), staying asleep, or early morning awakening; any naps?
Acting out dreams during sleep or other abnormal movements while sleeping
Difficulty distinguishing dreams from reality when transitioning to and from sleep.
The significance of these signs and symptoms will be made clearer in Section II: Differential Diagnosis of Memory Loss and Dementia .
In addition to obtaining a general medical history, it is worthwhile asking specifically about disorders that can predispose an individual to memory loss. These include the following, which are mainly related to cerebrovascular disease (note that disorders covered in the review of systems have not been repeated):
hypertension
hypercholesterolemia
coronary artery disease
atrial fibrillation and other cardiac arrhythmias
obstructive sleep apnea.
When eliciting a history of allergies, it is worthwhile to be attuned to two particular kinds of reactions to medications.
First, are there medications that caused significant confusion or agitation when administered? Susceptibility to confusion from medications may be present before the clinical onset of Alzheimer’s disease or other dementia. Such medications may include narcotics, such as Percocet or Darvocet, benzodiazepines, such as diazepam and lorazepam, antihistamines, such as Benadryl and Tylenol PM, and anticholinergic medications, such as scopolamine and meclizine.
Second, are there reactions to medications used to treat Alzheimer’s disease? If so, are these true allergic reactions to the medications, common side effects, or rare and unusual problems? If side effects to potential treatment medication are present (such as nausea to a cholinesterase inhibitor), these should be carefully noted. Discussions regarding how to best deal with side effects to treatment medications are discussed in Section III: Treatment of Memory Loss, Alzheimer’s Disease, and Dementia .
Several elements of the social history are important when diagnosing memory loss.
Cigarette smoking, whether past or present, is of course a risk factor for cerebrovascular disease. Current smoking also poses a significant risk of fires, as the patient with memory loss may forget and leave their lit cigarette or cigar in a place where it may start a fire.
Alcohol use is important to ascertain for two reasons. First, when alcohol use is severe, it can cause memory loss from Wernicke–Korsakoff syndrome (see Chapter 17 ), and even more mild chronic alcohol use can cause frontal/executive dysfunction. Second, many patients with mild memory loss experience an exacerbation of their memory difficulties while drinking, and remember very little during the time that the alcohol is in their system. Some patients may become outright confused with as little as two glasses of wine. Patients may also not remember how many drinks they have had, and end up drinking too much. Lastly, patients with Alzheimer’s disease may also be self-medicating for anxiety and/or depression.
Use or abuse of prescription medications and other drugs should also be elicited. Benzodiazepines and narcotics are all too commonly abused, and can present as an apparent dementia, particularly when fluctuations in mood, behavior, and cognition are present.
When making a diagnosis of memory loss, other cognitive impairment, or dementia—particularly when symptoms are very mild—it is critical to take into account the patient’s education and previous occupation. We expect, of course, that a college professor with a PhD would score better on most standard cognitive tests than an individual with a high school education. Taking education and occupation into account is particularly important when interpreting standard cognitive tests. For example, scoring 28 out of 30 on the Mini-Mental State Examination (MMSE) ( ) or 27 out of 30 on the MoCA (the Montreal Cognitive Assessment; www.mocatest.org ) may be normal for the 65-year-old factory worker with a high school education, but would be very concerning for a retired physician of the same age with 20 years of education.
Does the patient have any longstanding prior problems with attention, memory, or other cognitive function? Do they have dyslexia, another learning disability, or attention-deficit hyperactivity disorder? Has she always had a poor memory for names? Did he always become lost when trying to find a new place? Understanding the patient’s baseline memory and other cognitive abilities can help you interpret the current symptoms and the results of the cognitive tests appropriately.
Patients with memory loss need the support of others. Support can be present in many forms, including emotional, financial, and assistance with daily function at many levels. Knowing what supports the patient has will help to guide treatment options, such as whether prescribed medications can be complicated or need to be simple, and whether options such as day programs, moving in with a family member, or moving to an assisted living facility are available.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here