Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The analysis of spontaneous activity is the first part of the needle electromyography (EMG) examination of every muscle. The presence of abnormal spontaneous activity on EMG is of key importance and yields several important pieces of information. First, the distribution of abnormal spontaneous activity often indicates the neuroanatomic localization of the lesion. For example, in an isolated radiculopathy, denervation potentials are restricted to muscles in the same myotome. Second, the type of spontaneous activity often provides specific diagnostic information. Certain types of spontaneous activity are associated only with specific disorders. For example, myotonic discharges are seen only in a few myopathies and in hyperkalemic periodic paralysis. Third, the degree or amount of spontaneous activity often helps to determine the severity of the lesion. Finally, the presence of abnormal spontaneous activity may yield information regarding the time course of the lesion. For example, in a radiculopathy, several weeks must pass before fibrillation potentials are seen in the limbs.
The identification of any spontaneous activity can be achieved by either pattern recognition or analysis of the waveform. With experience, the characteristic appearance and sound of each waveform become easily recognizable. However, when first learning needle EMG or when encountering an unusual waveform, one must be able to systematically analyze the waveform according to the following attributes: (1) morphology, (2) stability, and (3) firing characteristics ( Fig. 14.1 ). Using this information, nearly every spontaneous waveform can be identified correctly.
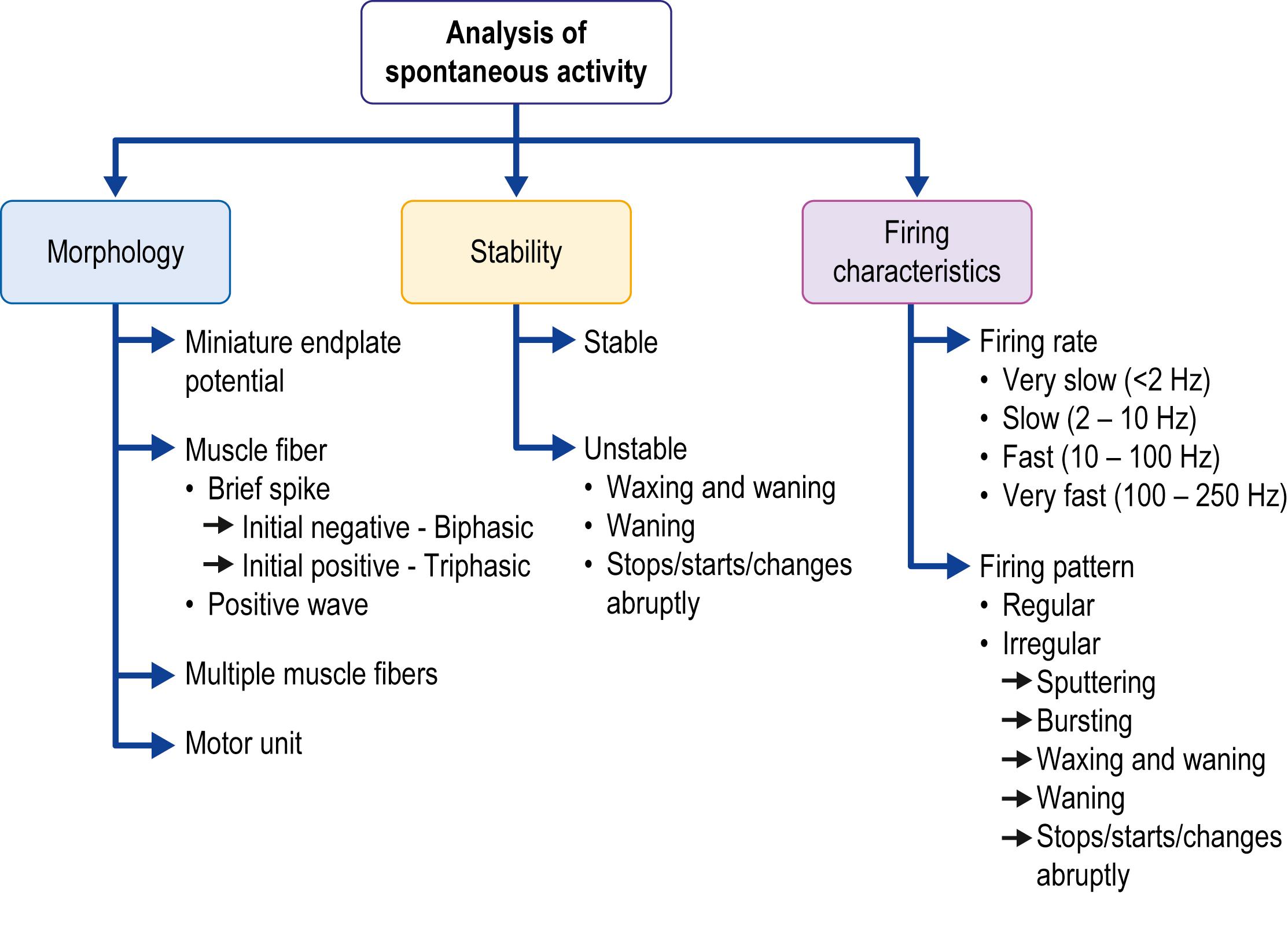
The source of a spontaneous discharge often can be identified by its distinctive morphology, specifically the size and shape of the potential (amplitude, duration, number of phases) and its initial deflection. By defining the source generator, the differential diagnosis of the discharge can be significantly narrowed. The source generators that must be differentiated are ( Figs. 14.2 and 14.3 , Table. 14.1 ):
The neuromuscular junction (NMJ)
A single muscle fiber
The terminal axon twig
A motor neuron/axon
Multiple muscle fibers linked together

| Potential | Source Generator/Morphology | Sound on Loudspeaker | Stability | Firing Rate | Firing Pattern |
|---|---|---|---|---|---|
| Endplate noise | Miniature endplate potential (monophasic negative) | Seashell | – | 20–40 Hz | Irregular (hissing) |
| Endplate spike | Muscle fiber initiated by terminal axonal twig (brief spike, diphasic, initial negative) | Sputtering, like fat in a frying pan | Stable | 5–50 Hz | Irregular (sputtering) |
| Fibrillation potential | Muscle fiber (brief spike, diphasic or triphasic, initial positive) | Rain on a tin roof or tick-tock of a clock | Stable | 0.5–10 Hz (occ. up to 30 Hz) | Regular |
| Positive sharp wave | Muscle fiber (diphasic, initial positive, slow negative) | Dull pops, rain on a roof | Stable | 0.5–10 Hz (occ. up to 30 Hz) | Regular |
| Myotonic discharge | Muscle fiber (brief spike, initial positive; or positive wave) | Revving engine | Waxing/waning amplitude | 20–150 Hz | Waxing/waning |
| Complex repetitive discharge | Multiple muscle fibers time-linked together | Machine | Usually stable; may change in discrete jumps | 5–100 Hz | Perfectly regular (unless overdriven) |
| Fasciculation potential | Motor unit (motor neuron/axon) | Corn popping | Stable | Low (0.1–10 Hz) | Irregular |
| Doublets, triplets, multiplets | Motor unit (motor neuron/axon) | Horse trotting | Usually stable; may change in number of potentials | Variable (1–50 Hz) | Bursts of twos, threes or a few potentials |
| Myokymic discharge | Motor unit (motor neuron/axon) | Marching soldiers | Usually stable; the number of potentials may change within the burst | 1–5 Hz (interburst) 5–60 Hz (intraburst) |
Bursting of the same individual motor unit potential |
| Cramp potential | Motor unit (motor neuron/axon) | Usually stable | High (20–150 Hz) | Interference pattern or one or more individual motor unit potentials | |
| Neuromyotonic discharge | Motor unit (motor neuron/axon) | Pinging | Decrementing amplitude | Very high (150–250 Hz) | Waning |
| Rest tremor | Motor unit (motor neuron/axon) | Marching soldiers | Rising and falling amplitude | 1–5 Hz (interburst) | Bursting—synchronous bursting of many different motor unit potentials |
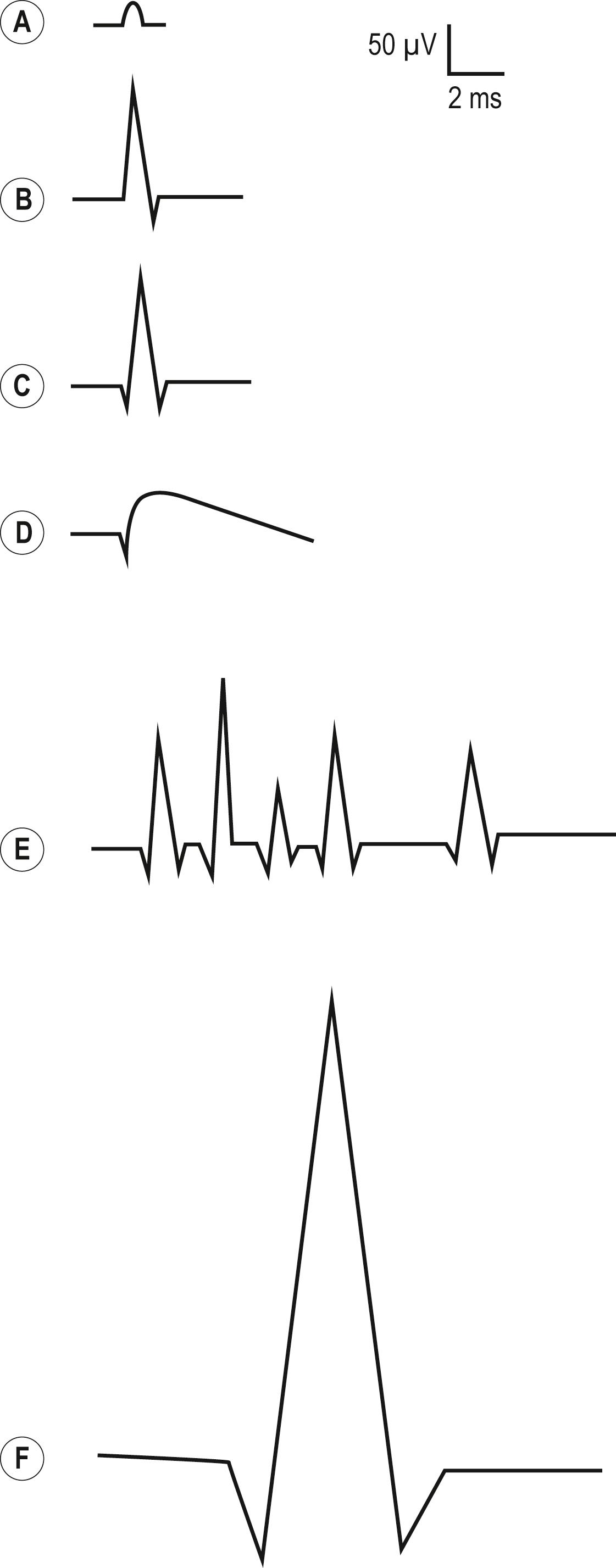
At the NMJ (i.e., endplate zone), miniature endplate potentials (MEPPs) occur spontaneously. They result from the normal spontaneous exocytosis of individual quanta of acetylcholine traveling across the NMJ, leading to a nonpropagated, subthreshold endplate potential. If the EMG needle is near the endplate zone, MEPPs can often be recorded. They have a distinctive small amplitude and monophasic negative morphology ( Fig. 14.2A ). These potentials are normal spontaneous discharges and are referred to as endplate noise .
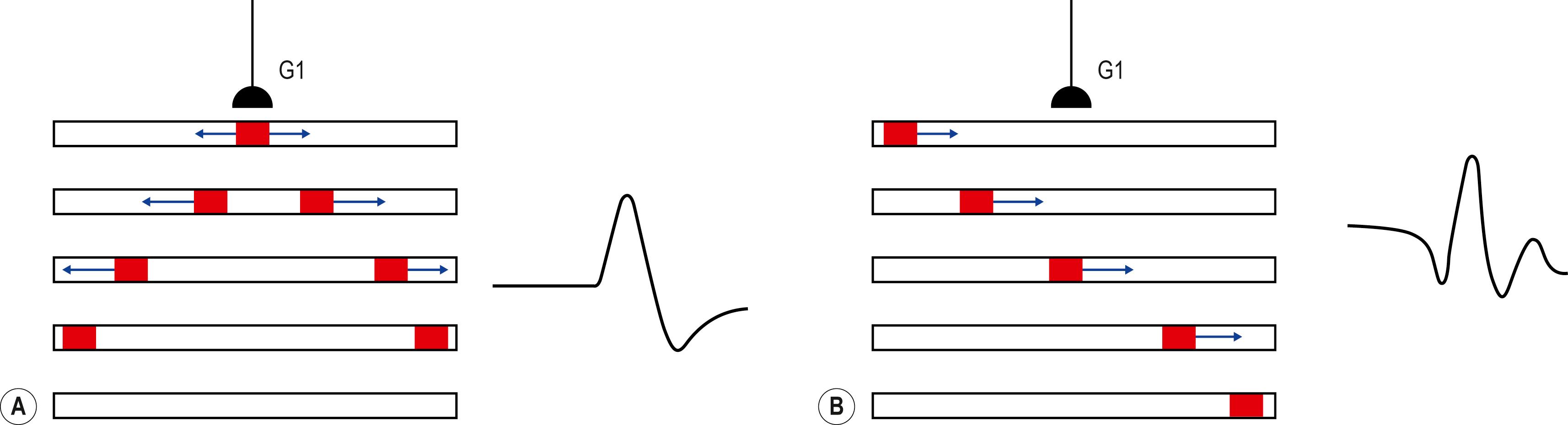
When a muscle fiber depolarizes to threshold, a muscle fiber action potential (MFAP) is created. The MFAP can assume one of two basic morphologies, either a brief spike or a positive wave. The brief spike typically is 1–5 ms in duration, with a low amplitude (typically 10–100 μV). The brief spike can be either biphasic or triphasic. A brief spike is seen when a single muscle fiber depolarizes spontaneously (e.g., in denervation), but it can also occur as the result of an individual terminal axon twig depolarizing and then propagating across the NMJ to create an MFAP. Attention to the initial deflection and to whether the brief spike is biphasic or triphasic often can help distinguish between the two ( Fig. 14.4 ). If the depolarization begins under the recording needle electrode, a biphasic potential is seen with an initial negative deflection (i.e., negative peak followed by a short positive phase) ( Fig. 14.2B ). This signifies that the needle is at the endplate zone, where the depolarization begins, and usually is the result of the EMG needle irritating the terminal nerve twigs near the endplate zone. A nerve twig action potential then leads to an MFAP, known as an endplate spike , which is a normal finding (see Endplate Spikes section). The reason for the initial negativity is similar to that of the compound muscle action potential in motor nerve conduction studies, wherein the initial deflection is negative when the active recording electrode is properly placed over the motor endplate zone. Otherwise, brief spikes that occur from the spontaneous depolarization of single muscle fibers are associated with an initial positive deflection, usually with a triphasic morphology. When the depolarization begins at a distance from the needle, there is an initial positive deflection as it moves toward the needle, followed by a negative phase as it moves beneath the needle, and then a final positive deflection as it moves away from the needle ( Figs. 14.2C and 14.4B ).
In addition to the brief spike, an MFAP can assume a positive wave morphology, with an initial brief positive phase followed by a long negative phase ( Fig. 14.2D ). Both positive waves and initial positive, triphasic brief spikes are seen most often as denervating potentials, known as positive sharp waves and fibrillation potentials , respectively. However, it should not be surprising that myotonic discharges, which also originate in muscle fibers, have the same basic morphology as denervating potentials, either positive waves or brief spikes. This point exemplifies the important concept that morphology alone cannot be used to identify a potential . Although the morphology of a potential usually can be used to correctly identify its source generator, additional information regarding its stability and firing characteristics is needed to fully characterize and identify any potential (see later).
The next major category of spontaneous discharges are those that arise from motor neurons or their axons. Any discharge that occurs as a result of the spontaneous depolarization of a motor neuron or its axon (prior to its terminal branches) leads to a potential with the morphology of a motor unit ( Fig. 14.2F ), known as a motor unit action potential (MUAP). Spontaneous discharges generated by the motor neuron or its axon include fasciculation potentials, doublets, triplets, and multiplets, myokymic discharges, neuromyotonic discharges, and cramp potentials, all of which lie along the spectrum of abnormal spontaneous MUAPs. They can be differentiated from each other, however, by their stability and firing characteristics (described in the following subsections). If the motor unit is normal, the MUAP morphology will be normal: typically two to four phases, 5–15 ms in duration, and variable amplitude depending on the needle position. If the motor unit is pathologic, the number of phases, duration, and amplitude of the MUAP may be abnormal. Differentiating a MUAP from an MFAP usually is straightforward and typically can be done quite simply by analyzing its duration and amplitude.
The last distinctive waveform that must be recognized is that of time-linked individual muscle fibers, such as occurs in complex repetitive discharges (CRDs) ( Fig. 14.2E ). One might ask how this waveform differs from a MUAP, which also represents many muscle fibers linked together. The difference is that the muscle fibers in a motor unit fire more or less synchronously and, in almost every situation, summate to create a larger potential 5–15 ms in duration. In contrast, the multiple muscle fibers in a CRD fire consecutively and usually are discernible as individual spikes that are time linked together.
Assessment of the stability of a waveform can be very informative. Nearly all spontaneous potentials are relatively stable in their morphology. If the morphology of the potential changes, note should be made of whether it waxes and wanes (amplitude goes up and down), wanes (amplitude goes down), or changes abruptly. MFAPs that wax and wane in amplitude are characteristically seen in myotonic discharges. Marked decrementing of an MUAP amplitude occurs in neuromyotonic discharges. CRDs typically are perfectly stable, but if additional loops or circuits drop in or out, the morphology may change abruptly in distinct or quantal jumps.
After assessing the potential’s morphology and stability, the electromyographer should look at the potential’s firing characteristics, both the discharge pattern and firing rate. Note whether the pattern is regular or irregular. If it is regular, is it perfectly regular? Fibrillation potentials and positive sharp waves are more or less regular (they may occasionally slow down or speed up ever so gradually), but CRDs are perfectly regular. If it is irregular, is it sputtering (e.g., endplate spikes), waxing/waning (e.g., myotonic discharges that speed up and slow down), or waning (e.g., neuromyotonic discharges that slow down)? Is there a bursting pattern (relative electrical silence between groups of discharges)? Such a pattern is characteristic of doublets and triplets as seen in tetany, and myokymic discharges. Note if the firing rate is very slow (<2 Hz), slow (2–10 Hz), fast (10–100 Hz), or very fast (>100 Hz). If the potentials fire very slowly, <4–5 Hz, this is important because this slow of a firing rate signifies that the discharges cannot be voluntary. Voluntary activation of a motor unit has a firing frequency of at least 4–5 Hz. Any potential that fires more slowly than 4–5 Hz cannot be under voluntary control and must be spontaneous. Conversely, extremely high firing rates are characteristic of neuromyotonic discharges, which can fire as fast as 150–250 Hz.
Table 14.1 summarizes the morphology, stability, and firing characteristics of the common spontaneous potentials seen during the needle EMG.
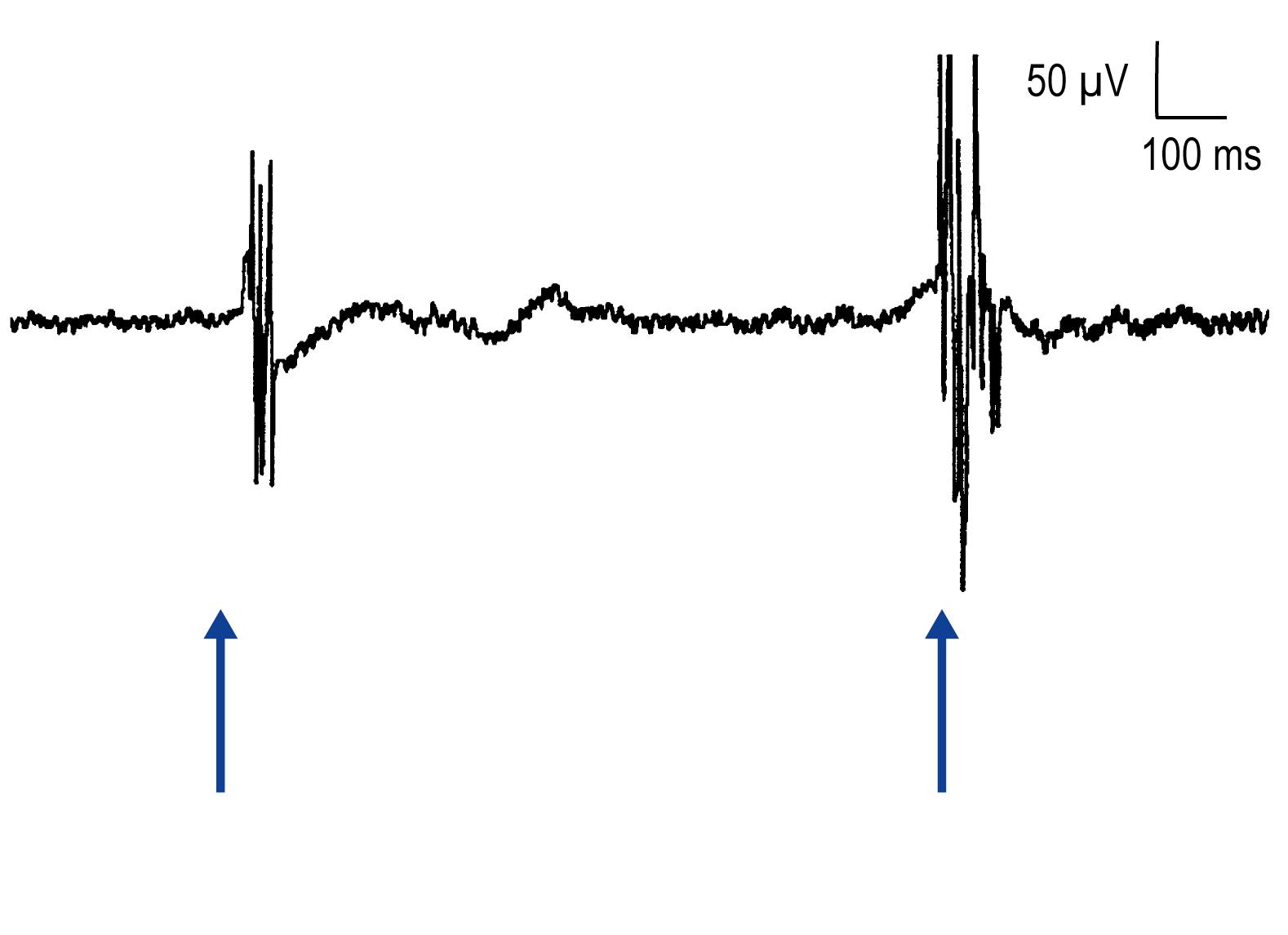
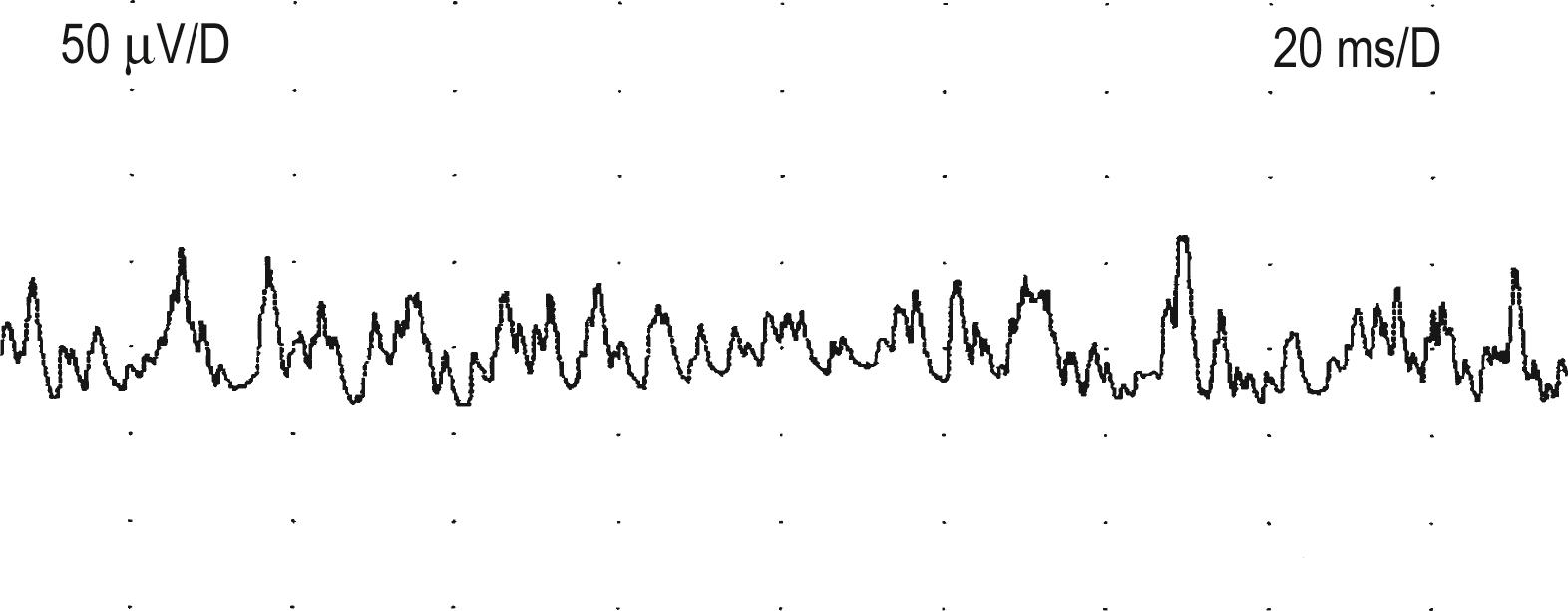
The assessment of spontaneous activity on needle EMG examination of each muscle begins with first looking at insertional activity. When a needle is quickly moved through muscle, muscle fibers depolarize in a brief burst for several hundred milliseconds, known as insertional activity, which is a normal finding ( Fig. 14.5 ). The presence of insertional activity is important to the electromyographer to confirm that the needle is in muscle rather than fat or subcutaneous tissue. At least four to six brief needle movements are made in four quadrants of each muscle to assess insertional activity. Needle movement resulting in any waveform other than endplate potentials (see the following section) that lasts longer than 300 ms indicates increased insertional activity. Increased insertional activity may be seen in both neuropathic and myopathic conditions. In rare conditions, where muscle has been replaced by fat and fibrous connective tissue, insertional activity may actually be decreased.
All spontaneous activity is abnormal, with the important exception of potentials that occur in the muscle endplate zone (i.e., the NMJ). Muscle endplate usually is found near the center of the muscle belly and often is encountered during routine EMG. Patients frequently perceive a deep, burning, unpleasant sensation when the needle is placed in the endplate zone. Two types of spontaneous activity occur here: endplate noise and endplate spikes. It is of utmost importance to properly identify these potentials so as not to mistake them for pathologic spontaneous activity.
These are low-amplitude, monophasic negative potentials that fire irregularly at 20–40 Hz and have a characteristic “seashell” sound on EMG ( Fig. 14.6 ) [Video 14.1]. Physiologically, they represent MEPPs. They are recognized by their characteristic shape and sound and by their frequent association with endplate spikes (described in the next subsection).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here