Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The bacterial hypothesis of the origin of mitochondria suggests that approximately 1–2 billion years ago, alpha-purple bacteria were incorporated into evolving eukaryotic cells. During evolution, these bacteria transferred many of their essential genes to the nuclear chromosomes. Mitochondria still have many remnants of their bacterial origin, such as the use of N -formylmethionyl-tRNA (transfer ribonucleic acid) as the initiator of protein synthesis.
Our current knowledge of mitochondrial genetics began with evidence of cytoplasmic genetic inheritance (rho factor in yeast) in the 1940s. Two decades later, mitochondrial deoxyribonucleic acid (mtDNA) was first recognized in chick cells and shortly thereafter in yeast, establishing the identity of the rho factor with mtDNA. In 1951, Denis Leigh first described the striking neuropathology resembling Wernicke encephalopathy in a child who had died of a neurological disease that now bears his name, Leigh syndrome . In 1959, following astute bedside clinical observations made in a single patient with nonthyroidal hypermetabolism, Rolf Luft deciphered biochemical abnormalities involving a defect in oxidative phosphorylation (OXPHOS) and described a rare neurological condition that we now call Luft disease . In the 1960s, morphological abnormalities of mitochondria were recognized by electron microscopy and special stains (Gomori trichrome and its modification) in newly characterized muscle diseases. In the early 1970s, abnormalities in respiratory chain function were associated with disorders mainly involving the central nervous system (CNS) and muscle. In the following year, the first examples of myopathies due to isolated deficiencies of muscle carnitine and carnitine palmitoyltransferase (CPT) were reported. These clinical discoveries were the starting point for a rapid expansion in the field of mitochondrial pathophysiology. By 1981, the complete sequence of human mtDNA was elucidated.
In 1988 a major breakthrough in our understanding of mitochondrial disorders occurred with the report of the association of sporadic human encephalomyopathies with large deletions of mtDNA ( ) and of Leber hereditary optic neuropathy (LHON) with a point mutation at nucleotide pair (np) 11778 in the mtDNA ( ). More than 250 pathogenic point mutations of the mtDNA, large-scale mtDNA deletions, and rearrangements have been subsequently reported (MITOMAP [2019]: A Human Mitochondrial Genome Database. http://www.mitomap.org , 2019). More than 85% of mitochondrial proteins are encoded by the nuclear DNA (nDNA), with at least 300 nuclear genes linked to mitochondrial disease ( ). However, given that approximately 1500 mitochondrial proteins are nuclear-encoded ( ), it is highly probable that many unknown mitochondrial disorders due to nDNA defects still exist. The delineation of human mtDNA variation and genetics has also provided startling new insights into the evolution and migration of human populations ( ). Mitochondria may also play an important role in neurodegenerative diseases and the aging process ( ).
The diseases included under the term mitochondrial disorders are so diverse and involve so many parts of the nervous system and other organs that the whole spectrum cannot be easily addressed in any one chapter. Therefore the disorders related to intermediate metabolism and mitochondrial Krebs cycle are discussed with inborn errors of metabolism in Chapter 91 . The syndrome that combines epilepsy and ragged-red muscle fibers (myoclonic epilepsy and ragged-red fibers [MERRF]) is discussed in Chapter 48, Chapter 100 . The syndrome of progressive external ophthalmoplegia (PEO) is discussed with other abnormalities of eye movement ( Chapter 17 ), and LHON with other causes of vision loss ( Chapter 16 ). This chapter overviews the principles of mitochondrial genetics and pathophysiology. It also provides a summary of the clinical features and management of patients with mitochondrial disorders and a brief review of those neurodegenerative diseases where mitochondrial dysfunction is best characterized ( ).
MtDNA is a 16,569-np double-stranded, closed, circular molecule located within the matrix of the double-membrane mitochondrion. Each human cell contains a dynamic network of mitochondria and hundreds of mtDNA molecules. Human mtDNA encodes 13 of the 89 subunits of the mitochondrial respiratory chain, as well as the small (12S) and large (16S) ribosomal RNAs (rRNAs) and 22 tRNAs necessary for intramitochondrial protein synthesis ( Fig. 93.1, A ).
![Fig. 93.1, A , Human mitochondrial DNA (mtDNA) map. The mtDNA encompasses 16,569 np, with numbering starting at OH and proceeding counterclockwise around the circular map. Each gene is identified by shading, and the transfer RNA gene is identified by the letter of its cognate amino acid. Mutation sites of common mitochondrial diseases are indicated. B , Schematic representation of the mitochondrial respiratory chain located in the inner mitochondrial membrane. Electrons are transferred from complexes I and II to complex III via the mobile lipid carrier, coenzyme Q 10 (CoQ 10 [ubiquinone]). Electrons are then transferred to complex IV through the protein mobile carrier, cytochrome c (Cyt c ). Electrons are finally transferred to molecular oxygen by complex IV. Three of the respiratory complexes (I, III, and IV) have a proton pumping mechanism coupled to the electron transfer. Pumping of protons to the intermembrane space generates a membrane potential and a proton gradient that flows back through complex V. The flow of protons through complex V enables ATP synthesis. ATP , Adenosine triphosphate; HSP , heavy strand promoter; LHON , Leber hereditary optic neuropathy; LSP , light strand promoter; MELAS , mitochondrial encephalomyopathy with lactic acidosis and stroke-like episodes; MERRF, myoclonic epilepsy with ragged-red fibers; MILS, maternally inherited Leigh syndrome; NADH , nicotinamide adenine dinucleotide; NARP, neuropathy, ataxia, and retinitis pigmentosa; PEO, progressive external ophthalmoplegia. Fig. 93.1, A , Human mitochondrial DNA (mtDNA) map. The mtDNA encompasses 16,569 np, with numbering starting at OH and proceeding counterclockwise around the circular map. Each gene is identified by shading, and the transfer RNA gene is identified by the letter of its cognate amino acid. Mutation sites of common mitochondrial diseases are indicated. B , Schematic representation of the mitochondrial respiratory chain located in the inner mitochondrial membrane. Electrons are transferred from complexes I and II to complex III via the mobile lipid carrier, coenzyme Q 10 (CoQ 10 [ubiquinone]). Electrons are then transferred to complex IV through the protein mobile carrier, cytochrome c (Cyt c ). Electrons are finally transferred to molecular oxygen by complex IV. Three of the respiratory complexes (I, III, and IV) have a proton pumping mechanism coupled to the electron transfer. Pumping of protons to the intermembrane space generates a membrane potential and a proton gradient that flows back through complex V. The flow of protons through complex V enables ATP synthesis. ATP , Adenosine triphosphate; HSP , heavy strand promoter; LHON , Leber hereditary optic neuropathy; LSP , light strand promoter; MELAS , mitochondrial encephalomyopathy with lactic acidosis and stroke-like episodes; MERRF, myoclonic epilepsy with ragged-red fibers; MILS, maternally inherited Leigh syndrome; NADH , nicotinamide adenine dinucleotide; NARP, neuropathy, ataxia, and retinitis pigmentosa; PEO, progressive external ophthalmoplegia.](https://storage.googleapis.com/dl.dentistrykey.com/clinical/MitochondrialDisorders/0_3s20B9780323642613000930.jpg)
The mtDNA is replicated and transcribed by using an origin and promoter for each of the two DNA strands, the G-rich heavy (H) strand and the C-rich light (L) strand. The H- and L-strand replication origins (OH and OL; see Fig. 93.1, A ) are relatively distant within the molecule, but the H- and L-strand promoters (PH and PL) are closely spaced and located adjacent to OH in the approximately 1000-np noncoding control region. This region also encompasses the D-loop, which is formed by replication initiation events from the OH. Research involving evolution of mammalian species and origin and migration of humans on earth has focused on the variation in a small hypervariable noncoding region within the D-loop. The replication mechanism of mtDNA may be more complex than originally suggested, in that the mtDNA can also replicate by the extension of both leading and lagging strands, a process resembling nDNA replication ( ).
The respiratory chain (see Fig. 93.1, B ) is located within the mitochondrial inner membrane and is composed of five multimeric enzyme complexes whose genes are dispersed between the mtDNA and nDNA. Complex I (nicotinamide adenine dinucleotide [NADH]–ubiquinone oxidoreductase) accepts electrons from the reduced form of NADH, whereas complex II (succinate–ubiquinone oxidoreductase) collects electrons from succinate. Both NADH and succinate are the products of the Krebs cycle. Enzyme complexes I and II transfer electrons to coenzyme Q 10 (CoQ 10 ). From CoQ 10 , the electrons flow through complex III (ubiquinone–cytochrome c oxidoreductase) to cytochrome c , then to complex IV (cytochrome c oxidase), and finally to oxygen to yield water. The electron transfer is coupled to proton (H + ) pumping by complexes I, III, and IV from the matrix to the intermembrane space, creating an electrochemical gradient across the inner membrane. This electrochemical gradient is used by complex V (adenosine triphosphate [ATP] synthase) as a source of energy to condense adenosine diphosphate (ADP) and inorganic phosphate (Pi) to synthesize ATP. ATP and ADP are then exchanged across the mitochondrial membrane by the adenine nucleotide translocator (ANT).
Complex I comprises approximately 46 subunits, 7 of which (ND-1, -2, -3, -4, -4L, -5, and -6) are encoded by the mtDNA; complex II has 4 subunits, none from the mtDNA; complex III includes 11 subunits, 1 (cytochrome b ) from the mtDNA; complex IV contains 13 subunits, 3 (COX-1, -2, and -3) from the mtDNA; and complex V contains 13 subunits, 2 (ATPase-6 and -8) from the mtDNA. The remaining subunits of complexes I, III, IV, and V; the entire complex II; the two small electron carriers, CoQ 10 and cytochrome c , and ANT are encoded by the nDNA. The mitochondrial rRNA and tRNA genes provide the structural RNAs for mitochondrial protein synthesis (i.e., for the expression of 13 mtDNA-encoded polypeptides). The majority of mitochondrial respiratory chain proteins are encoded by the nDNA in the cytosol. A complex mitochondrial importation process therefore enables the cytosolically synthesized nuclear-encoded mitochondrial respiratory chain subunits to be coassembled with mtDNA-encoded counterparts in the inner mitochondrial membrane. There are more than 1000 other nuclear genes which express mitochondrial proteins that are important for mitochondrial function.
Mitochondrial diseases therefore can arise from defects in the mtDNA (sporadic or maternal inheritance, see following section) or nDNA (sporadic or Mendelian inheritance). nDNA-related mitochondrial disorders result from defects involving nDNA-encoded mitochondrial polypeptides, including respiratory chain complexes, respiratory chain assembly, mtDNA maintenance, protein import, lipid dynamics, and biosynthesis of CoQ 10 . Table 93.1 summarizes a simplified clinical and genetic classification of mitochondrial diseases.
| Defects of Mitochondrial DNA | |||
|---|---|---|---|
| Disease/Syndrome | Main Mutation | Gene Location | Mode of Inheritance |
| PEO/multisystem with PEO | Single large deletion | Sporadic | |
| Deletion/duplication | Sporadic | ||
| nt-A3243G | tRNA Leu(UUR) | Maternal | |
| nt-C3256T | tRNA Leu(UUR) | Maternal | |
| KSS | Single large deletion | Sporadic | |
| Large tandem duplication | Sporadic | ||
| Pearson syndrome/KSS | Single large deletion | Sporadic | |
| MELAS | nt-A3243G | tRNA Leu(UUR) | Maternal |
| nt-T3271C | tRNA Leu(UUR) | Maternal | |
| MERRF | nt-A8344G | tRNA Lys | Maternal |
| Myopathy | Single large deletion | Sporadic | |
| nt-A3243G | tRNA Leu(UUR) | Maternal | |
| nt-G15762A | Cytochrome b | Sporadic | |
| MiMyCa | nt-C3254G | tRNA Leu(UUR) | Maternal |
| NARP/MILS | nt-T8993G | ATPase 6 | Maternal |
| LHON | nt-G3460A | ND1 | Maternal |
| nt-G11778A | ND4 | Maternal | |
| nt-T14484C | ND6 | Maternal | |
| Diabetes, optic atrophy, deafness | Single large deletion | Sporadic | |
| Tubulopathy, diabetes, ataxia | Large tandem duplication | Maternal | |
| Sideroblastic anemia | nt-T6721C | COX-I | Sporadic |
| Defects in Nuclear DNA Affecting Mitochondrial DNA or Enzyme Complexes | |||
|---|---|---|---|
| Disease/Syndrome | mtDNA/Enzyme Defect | Nuclear Gene/Locus | Mode of Inheritance |
| PEO | Multiple mtDNA deletions | PEO1(Twinkle), ANT1, POLG1 and 2, SLC25A4 | Autosomal dominant/recessive |
| MNGIE | Multiple mtDNA deletions | ECGF1 | Autosomal recessive |
| Leigh syndrome | Complex IV | SURF1 | Autosomal recessive |
| Complex I | NDUFS4, 6, 7, 8, NDUFV2 | Autosomal recessive | |
| Leukodystrophy/myoclonus | Complex I | NDUFV1 | Autosomal recessive |
| Encephalopathy/cardiomyopathy | Complex I | NDUFV2 | Autosomal recessive |
| Leigh syndrome | Complex II | SDH | Autosomal recessive |
| GRACILE syndrome | Complex III | BCS1L | Autosomal recessive |
| Leigh syndrome | Complex IV | SCO1, COX10, COX15, RPPRC | Autosomal recessive |
| Encephalomyopathy/cardiomyopathy | Complex IV | SCO2 | Autosomal recessive |
| Encephalopathy, tubulopathy | Complex IV | COX10 | Autosomal recessive |
| Hypertrophic cardiomyopathy | Complex IV | COX15 | Autosomal recessive |
| Encephalopathy | Complex V | ATPAF2, ATP5E | Autosomal recessive |
| Encephalopathy, hepatopathy | mtDNA depletion | DGUOK, SUCLA2 | Autosomal recessive |
| Infantile myopathy | mtDNA depletion | Thymidine kinase 2 | Autosomal recessive |
| Alpers syndrome | mtDNA depletion | POLG | Autosomal recessive |
| CMT2 | Mitochondrial dynamics | MFN2, MT-ATP6 | Autosomal dominant, maternal |
| Optic atrophy, deafness, neuropathy | Mitochondrial dynamics | OPA1 | Autosomal dominant |
| Ataxia, Leigh syndrome, hepatorenal failure. | Coenzyme Q 10 function | Coenzyme Q 10 biosynthesis protein | Autosomal recessive |
| X-linked ataxia/sideroblastic anemia | Iron exporter | ABCB7 | X-linked |
| Friedreich ataxia | Iron storage protein | Frataxin | Autosomal recessive |
| Hereditary spastic paraplegia | Metalloprotease | Paraplegin | Autosomal recessive |
| Parkinsonism | Oxidant-sensing protein | DJ1 | Autosomal recessive |
| Parkinsonism | Respiratory chain function, mtDNA, maintenance, mitophagy | PTEN-induced kinase 1 | Autosomal recessive |
| Juvenile parkinsonism | Mitophagy | Parkin | Autosomal recessive |
Patients inherit mtDNA from their mothers, and therefore the mode of transmission of mtDNA, including pathogenic mtDNA mutations, follows maternal line inheritance. A single case report has demonstrated paternal transmission of an mtDNA mutation ( ), although there is emerging evidence that biparental inheritance of mtDNA occurs in exceptional circumstances ( ). Maternal inheritance implies maternal transmission of mtDNA to all offspring but subsequent transmission only by females. Thus a disease expressed in all children of both sexes of an affected individual, without evidence of paternal inheritance, strongly suggests an mtDNA point mutation. However, exceptions to this general rule are encountered in clinical practice. First, a de novo point mutation in the mtDNA of the maternal germ cell line will not necessarily be transmitted to all children. Second, for unknown reasons, mtDNA mutations involving large-scale deletions, rearrangements, and point mutations in some protein-coding genes may occur sporadically and be due to mutations arising in the oocyte. Bottleneck expression of an mtDNA mutation may be enhanced in the fetus. Multiple deletions and depletion of mtDNA are autosomally transmitted, because they are the consequence of mutations in nuclear-encoded factors involved in mtDNA metabolism or replication. Third, maternal inheritance may not always be clinically evident because of extreme variability of clinical expression among family members due to heteroplasmy and the threshold effect (described in the following section).
Each cell contains thousands of mtDNA copies in a network of cytoplasmic mitochondria. MtDNA is constantly undergoing replication, fission, and fusion even in terminally differentiated cells. When all mtDNA molecules are identical, the mtDNA is homoplasmic . If pathogenic mtDNA mutations exist with normal (wild-type) mtDNA, then there are two populations of mtDNA in the system, and this is heteroplasmy . The severity of the phenotypic effects of the mtDNA mutations in heteroplasmic cells is determined by the proportion of the wild-type and mutant mtDNA. Neutral polymorphic sites (nonpathogenic mutations) of mtDNA are generally homoplasmic, whereas pathogenic mutations are mostly, but not invariably, heteroplasmic.
Heteroplasmy may occur at the level of the cell or at the level of the individual mitochondrion (intramitochondrial heteroplasmy). At cell division, mitochondria and mtDNA are randomly partitioned to be carried into the two daughter cells (mitotic segregation). Therefore mtDNA mutation is typically represented in a variable proportion of mitochondrial genomes, with the consequence that cells, tissues, and the whole individual would harbor variable proportions of mutant and wild-type mtDNA. Mitotic segregation explains how certain patients with mtDNA-related disorders may present with one manifestation at an early age and shift to another as they grow older as the proportions of heteroplasmy change with time in different tissues. For a disease to manifest in a tissue, the proportion of mutant mtDNA must be greater than the threshold level.
Threshold effect denotes the minimal critical number of mutated mtDNA molecules that would cause mitochondrial dysfunction in one or more tissues or organ systems. Variable somatic load of mtDNA mutation in different tissues and organ systems, or skewed heteroplasmy, is a universal finding in heteroplasmic states. It often changes over time, particularly in postmitotic cells such as neurons, and it increases with age. This in part explains the age-dependent penetration of many mitochondrial clinical phenotypes and age-related variability in their clinical features. The mtDNA mutation load needed for clinical expression is typically high and in the range of 70%–90% for both point mutations and deletions. The mutation threshold effect is believed to be affected by the oxidative metabolic requirement of a particular tissue. For example, the threshold effect may manifest itself at lower concentrations of mutated mtDNA in tissues that are inherently dependent on high oxidative metabolism, such as brain, eye, myocardium, and skeletal muscle.
Examples of threshold effect and mitotic segregation include patients with mitochondrial encephalomyopathy with lactic acidosis and stroke-like episodes (MELAS) who may present with only episodic headache in childhood but with stroke-like episodes and neurological deficits as they age and the pathogenic mutations accumulate in brain and cerebral vasculature. Infants with Pearson syndrome (a hematopoietic disease) may survive their disease because the proportion of mtDNA with deletions may decrease as bone marrow cells with heavy mutation loads are selected against. Following this process of outgrowing the hematopoietic disease in childhood, individuals with Pearson syndrome may later develop a different clinical phenotype such as Kearns-Sayre syndrome (KSS) as the mutation accumulates in their postmitotic neurons and muscle fibers.
Mitochondria have several functions in maintaining cellular homeostasis, such as transient storage of intracellular calcium, fatty acid oxidation, the Krebs cycle, and iron metabolism ( ). Mitochondria also have a key role in the regulation of apoptosis ( ). One of the most important roles of mitochondria is to catalyze the phosphorylation of the majority of cellular ADP to ATP. ATP is generated by oxidation of intermediates such as NADH and reduced flavin adenine dinucleotide (FADH2) via the process of OXPHOS within mitochondria by the respiratory chain enzymes. Several intermediary metabolic pathways from carbohydrates, fatty acids, and amino acids converge in mitochondria at the level of acetyl coenzyme A (acetyl CoA) for the final conversion of the fuel into ATP. Pyruvate is the terminal product of anaerobic glycolysis and is transported across the inner mitochondrial membrane to the mitochondrial matrix where it is converted to acetyl CoA. The transportation of pyruvate is coupled with the influx of hydrogen ions down their electrochemical gradient across the inner mitochondrial membrane. Pyruvate can also be generated during the catabolism of the amino acids alanine, serine, glycine, and cysteine. Transport of free fatty acids across the mitochondrial membrane requires two enzymes (CPTs I and II), a carrier molecule ( l -carnitine), and a translocase (carnitine-acylcarnitine translocase). Fatty acids are also metabolized into acetyl CoA. Acetyl CoA enters the Krebs cycle, where three molecules of NADH and one molecule of FADH 2 are produced from each acetyl CoA. Molecules of NADH and FADH 2 donate electrons to the electron transport chain (NADH to complex I and succinate to FAD in complex II). The functional unit comprising the electron transport chain (complex I–IV) and complex V (ATP synthase) constitutes the OXPHOS system (see Fig. 93.1 , B ).
Lactic acid is the end product of glycolytic anaerobic metabolism and acts as a reservoir for excess pyruvate. Physiological states such as exercise may cause transient lactic acidosis. Pathological lactic acidosis occurs during anoxia/ischemia, in metabolic failure from liver disease and diabetes mellitus (secondary lactic acidosis), and in defects of OXPHOS (primary lactic acidosis) such as mitochondrial disorders. The blood lactate-to-pyruvate ratio reflects the NADH to NAD + ratio, or redox state , and is useful in the diagnosis of primary lactic acidosis. Defects in pyruvate dehydrogenase (PDH), which catalyzes the conversion of pyruvate to acetyl CoA with the conversion of NAD + to NADH, are associated with a low redox state (due to increased NAD + ), and usually produce elevated levels of lactate and pyruvate with normal or slightly low lactate/pyruvate ratios (<20). OXPHOS defects often cause a high redox state (due to increased NADH accumulation) and generally produce a high lactate/pyruvate ratio (>20) as NADH and pyruvate are converted to lactate by lactate dehydrogenase.
Neurons, myocardial and skeletal muscle, liver, and renal tissues are highly dependent on oxidative metabolism and are most commonly involved in mitochondrial diseases. Neurons especially require high levels of ATP production to maintain ion homeostasis following controlled flux of ions across the cell membrane during electrical signaling. Within the brain, the high metabolic activity of the basal ganglia makes them vulnerable to oxidative metabolic defects. Necrosis of the basal ganglia and brainstem is an early feature of Leigh syndrome and is common in other mitochondrial cytopathies.
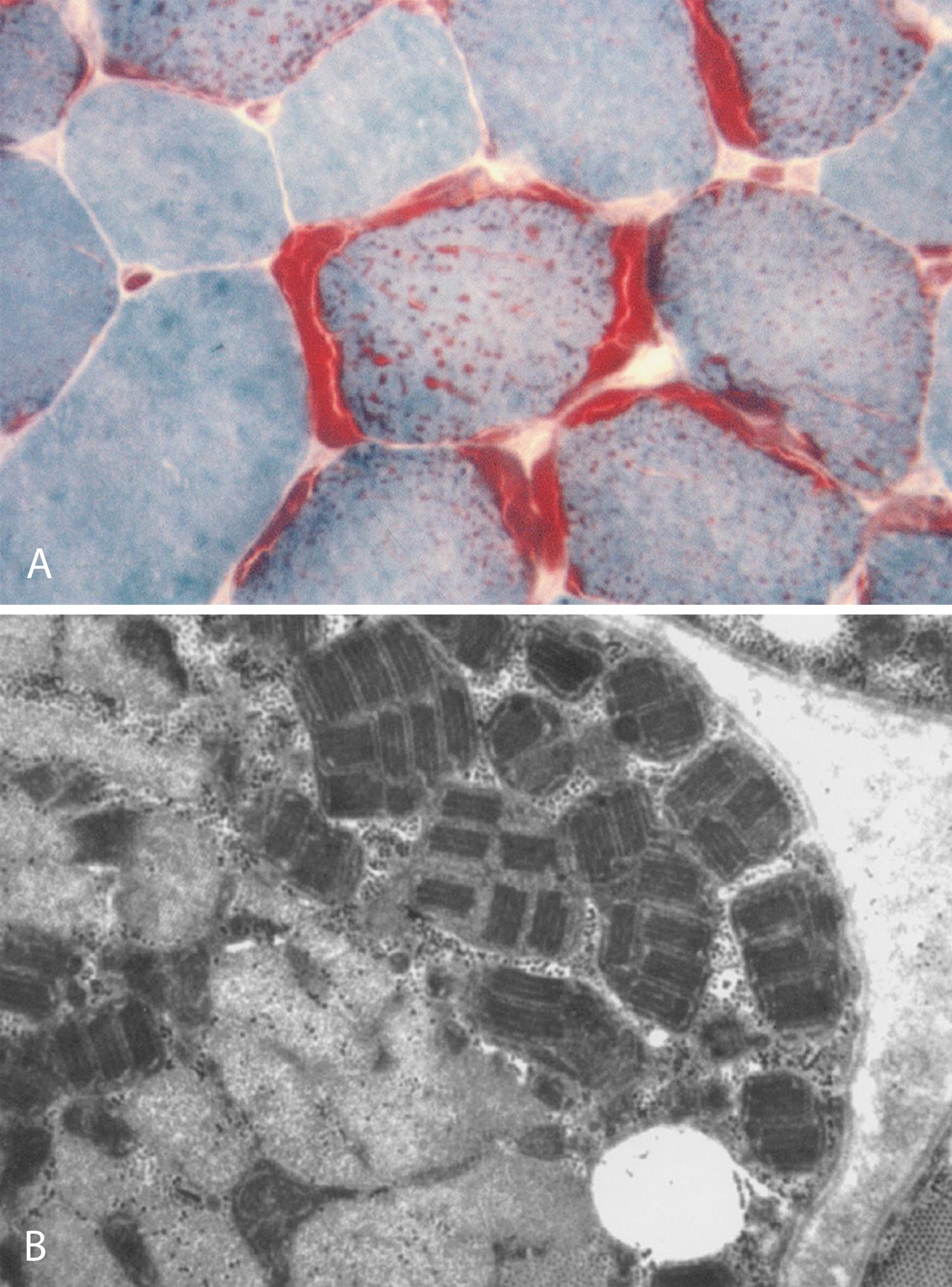
In skeletal muscle, some fibers are severely involved and others may appear normal on histological analysis. With more severe involvement, the combination of patchy myofibrillar degeneration along with mitochondrial proliferation gives rise to the so-called ragged-red appearance of fibers on modified Gomori trichrome staining ( Fig. 93.2 , A ). Defective OXPHOS may result in compensatory mitochondrial proliferation, particularly in type I and IIA muscle fibers. Ultrastructural analysis can demonstrate abnormal mitochondrial morphology such as intramitochondrial paracrystalline inclusions (see Fig. 93.2 , B ). Patients with mitochondrial disorders can show a wide range of symptoms, including any combination of developmental delay, short stature, small muscle bulk, seizures, vision loss, hearing impairment, peripheral neuropathy, autonomic nervous system difficulties, gastrointestinal dysfunction, endocrine problems, hematopoietic disease, and failure to thrive ( Box 93.1 ). The presentation of a particular mitochondrial disorder can be variable, even among affected individuals in the same family. Conversely, more than one pathogenic mutation can give rise to similar clinical phenotypes.
Cognition dysfunction
Seizures
Myoclonus
Migrainous headache
Stroke-like episode
Ataxia
Dystonia
Parkinsonism
Visual impairment
Sensorineural deafness
Spinal muscular atrophy
Sensorimotor polyneuropathy
Autonomic polyneuropathy
Progressive external ophthalmoplegia
Proximal limb myopathy
Exercise intolerance, myalgia, and fatigue
Rhabdomyolysis, myoglobinuria
Hypertrophic cardiomyopathy
Dilated cardiomyopathy
Cardiac conduction defects
Hepatic steatosis
Liver failure
Renal tubular acidosis
Fanconi syndrome
Myoglobinuric renal failure
Gastroparesis
Intestinal pseudo-obstruction
Constipation, diarrhea
Pancreatitis
Diabetes mellitus
Hypothalamic hypogonadism
Hypothyroidism
Hypoparathyroidism
Hypoadrenalism
Failure to thrive
Developmental delay or regression
Short stature
Cataracts
Anemia
Pancytopenia
Lipomas
The complex inheritance patterns and clinical heterogeneity of mitochondrial diseases often result in incorrect or delayed diagnosis of the affected individuals. This delay can result in increased morbidity or mortality. For example, patients with specific metabolic defects such as β-oxidation of fatty acids can benefit from appropriate manipulations of diet and physical activity. CoQ 10 (ubiquinone) and l -carnitine replacements are often effective in rare metabolic disorders of CoQ 10 and primary systemic carnitine deficiencies. Failure to make a precise genetic diagnosis and, in turn, the lack of appropriate genetic counseling, can lead to the subsequent birth of affected children in unsuspecting families. Leigh syndrome is a good example in that the phenotype can vary among members of the same family and can be inherited in the maternal line (mtDNA-related mutations) or in Mendelian (autosomal or sex-linked) inheritance patterns.
A detailed clinical history and examination in conjunction with experienced interpretation of a battery of complex laboratory results are often required to make an accurate diagnosis. This process is often best carried out in a specialist mitochondrial clinic and subsequently discussed at a multidisciplinary meeting involving neurologists, pediatricians, geneticists, pathologists, and biochemists. Diagnostic criteria for mitochondrial disorders have previously been proposed ( ). However, the usefulness of categorizing patients as having “possible” mitochondrial disease has recently been questioned ( ).
Although the overall clinical spectrum of mitochondrial disorders is broad, recognized patterns of clinical presentations, clinical signs, and investigations have emerged. A detailed extended family history is essential in deciphering subtle clues suggesting a maternal line of inheritance. Any patient with unexplained multisystem problems, particularly affecting the nervous system, skeletal muscle, liver, kidney, and heart, may have mitochondrial disease. Rare presentations can be of mitochondrial origin, such as stroke-like episodes with MELAS, chronic ophthalmoplegia in KSS, and a movement disorder in children or young adults with Leigh syndrome. Patients and families often report a history of periods of severe fatigue with intercurrent illnesses, trauma, or surgery. Affected individuals may develop exacerbations, such as an increase in seizures, or new symptoms, such as an episode of lactic acidosis, during a seemingly minor illness. The patient may develop a permanent neurological deficit following these physiological stressors.
The mitochondrial metabolic test battery includes serum creatine kinase (CK), lactate and pyruvate, plasma and urine acylcarnitines, blood and urine amino acids, urine organic acids, and cerebrospinal fluid (CSF) lactate and pyruvate (if the CNS is involved). The lactate/pyruvate ratio may differentiate disorders of the OXPHOS system in comparison to more proximal metabolic defects such as PDH deficiency. However, normal values for the lactate and lactate/pyruvate ratio in a patient do not exclude mitochondrial disease; mtDNA-related diseases are generally associated with normal or only mildly elevated resting blood lactate levels but often with a significant rise with exercise. Serum CK is usually normal or mildly elevated in patients with mitochondrial myopathies. Blood levels of free carnitine are often decreased in mtDNA-related disorders, with a relative increase in acylcarnitine levels. The interpretation of test results of free and total carnitine, blood and urine amino acids, and urine organic acids is discussed in Chapter 91 .
A controlled muscle exercise test may offer a useful noninvasive tool to investigate muscle oxidative metabolism. Lactate level, oxygen extraction from hemoglobin (near-infrared spectroscopy), and the ratio of phosphocreatine (PCr) to Pi ( 31 P magnetic resonance spectroscopy [MRS]) have been measured in muscle at rest and during exercise and recovery. In patients with mitochondrial dysfunction, PCr:Pi ratios are lower than normal at rest, decrease excessively during exercise, and return to baseline values more slowly than normal controls. However, normative PCr:Pi values overlap with those in patients with mitochondrial disorders, and this test is not suitable for infants and young children because it requires a high degree of patient cooperation.
The four most common neuro-ophthalmological mitochondrial disorders are LHON, PEO, pigmentary retinopathy, and retrochiasmal visual loss. Standard flash electroretinograms are typically normal in LHON. Visual evoked responses are predictably abnormal in patients with visual loss. KSS is a subset of PEO associated with ataxia, cognitive dysfunction, cardiac conduction defects, and elevated protein in CSF. The most common pigmentary retinopathy appearance in mtDNA-related diseases is that of “salt-and-pepper” retinopathy that typically becomes more prominent with advancing age. Macular involvement and vascular attenuation are common in pigmentary retinopathy. Fluorescein angiography in LHON reveals vasculopathy without leakage, whereas rod-and-cone–specific electroretinography may help to confirm subtle changes of pigmentary retinopathy. Disruption of retrochiasmal visual pathways, generally due to stroke-like episodes, causes homonymous hemianopic defects or cortical blindness in patients with MELAS.
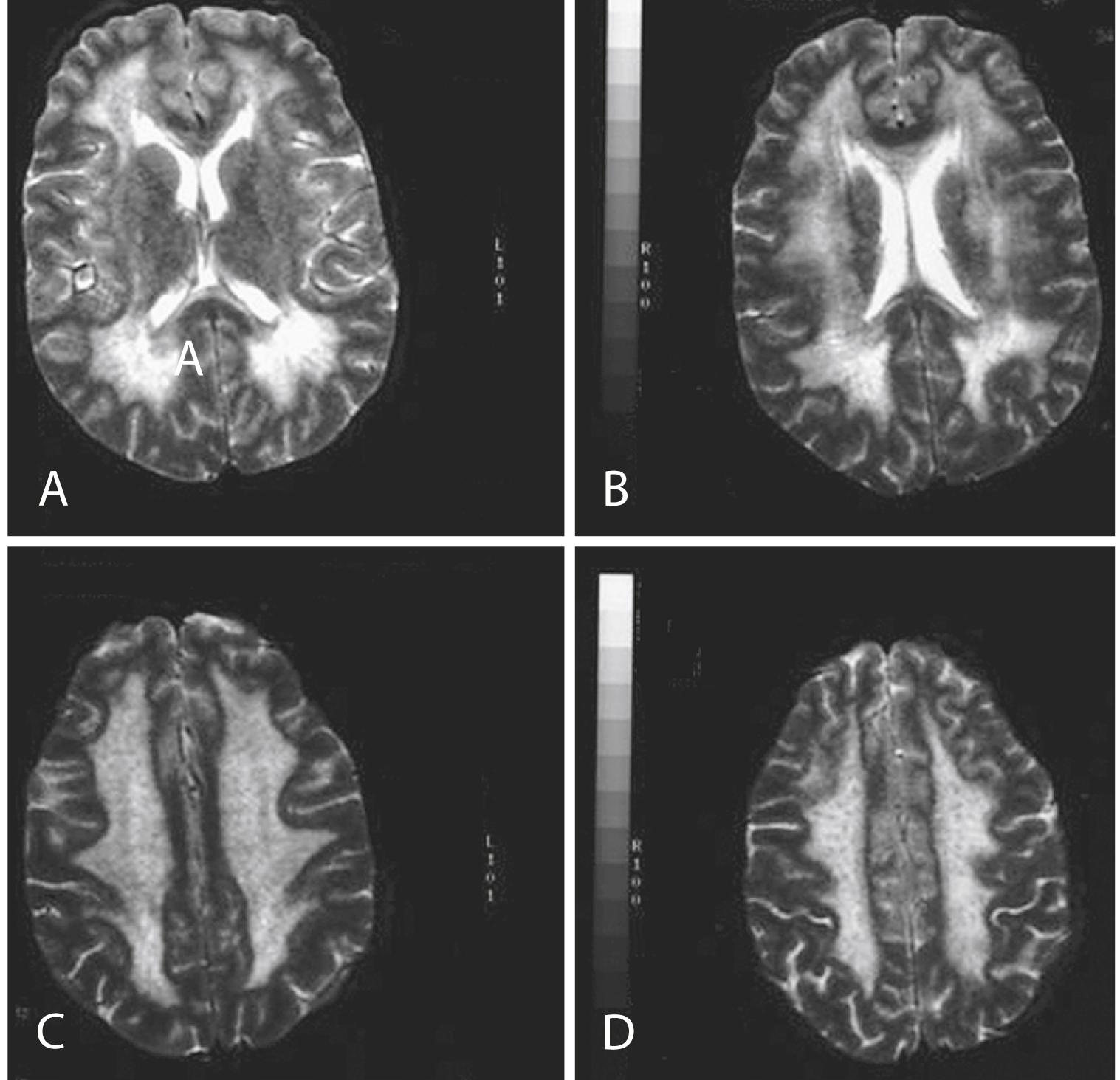
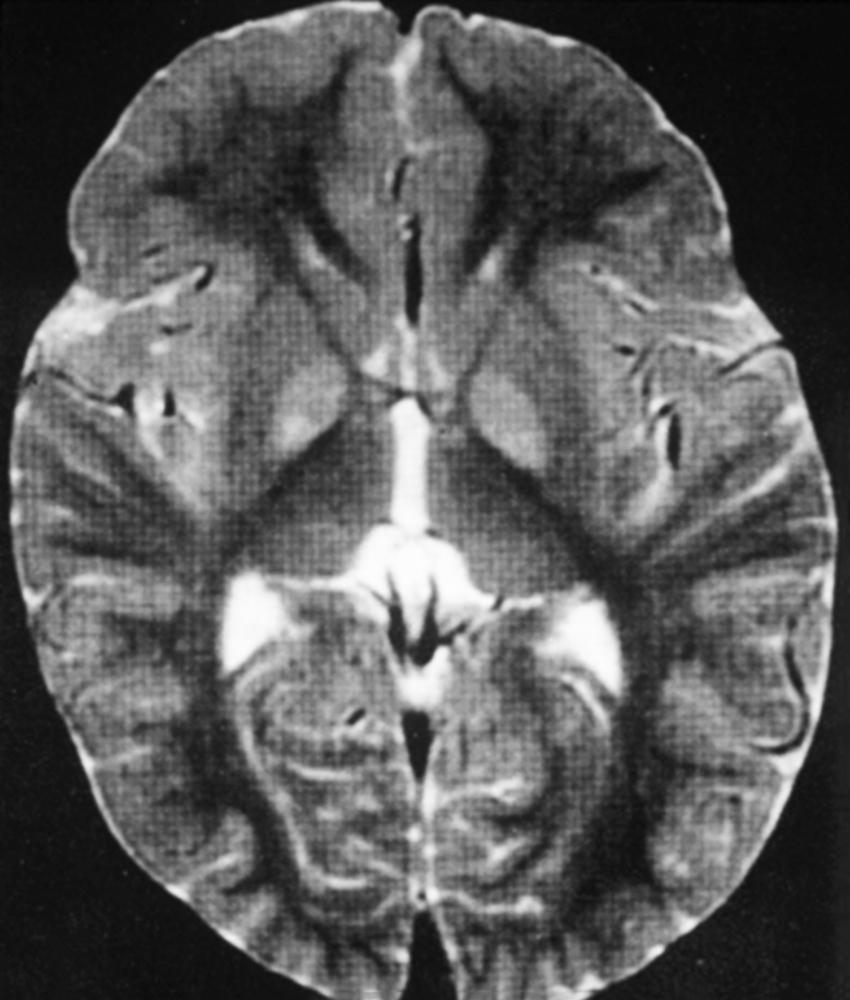
The use of neuroimaging, especially brain magnetic resonance imaging (MRI), has greatly facilitated the detection of CNS involvement in mitochondrial disorders. Brain atrophy is common in children with mitochondrial disease. Developmental delay and basal ganglia calcification are common in KSS and MELAS, and diffuse signal abnormalities of the white matter are characteristic of KSS and myoneurogastrointestinal encephalopathy (MNGIE) ( Fig. 93.3 ). The diagnosis of MELAS can be aided by the clinical association of stroke-like episodes with radiological lesions that do not conform to the anatomical territories of blood vessels and predominantly involve cortical gray matter ( Fig. 93.4 ). The initial or predominant lesions in MELAS are characteristically in the parietal-occipital region, and new lesions generally appear with acute illness and elevated CSF lactate levels. Leigh syndrome characteristically shows bilateral hyperintense signals on T2-weighted and fluid-attenuated inversion recovery (FLAIR) MRIs in the putamen, globus pallidus ( Fig. 93.5 ), and thalamus.

Extraocular muscle T2 signal is elevated in chronic progressive external ophthalmoplegia (CPEO) and correlates negatively with ocular movements, thus providing a potential quantitative measure of disease severity ( ). 1 H-MRS often detects lactate accumulation in the CSF and in specific areas of the brain, whereas positron emission tomography (PET), which measures metabolic flux, has identified several metabolic abnormalities in mitochondrial disease patients using radioisotopically labeled metabolites relevant to the study of bioenergetics.
An open muscle biopsy under local anesthesia provides material for histochemistry, ultrastructural studies, biochemistry, myoblast culture, and molecular genetic studies.
Many of the histopathological abnormalities found in muscle biopsies from patients with mitochondrial diseases are nonspecific and include excessive variability of muscle fiber size, fiber type–specific atrophy, scattered myofibrillar necrosis and regeneration, and intermyofibrillar lipid or glycogen accumulation. Mild peripheral nerve involvement is common in mitochondrial diseases, and the muscle biopsy may reveal evidence of partial denervation. Oxidative enzyme staining may show core targetoid fibers and fiber type grouping.
The hallmark feature in mitochondrial diseases is the ragged-red fiber (RRF) (see Fig. 93.2 , A ). In frozen sections stained with modified Gomori trichrome, subsarcolemmal and intermyofibrillar accumulation of mitochondria appear as bright red masses on at least three sides of the fiber, against the background of the blue myofibrils. These abnormal accumulations represent a compensatory proliferation of mitochondria, some of which are ultrastructurally normal and others dystrophic (see Fig. 93.2 , B ). The same fibers stain intensely blue with the histochemical reaction for succinate dehydrogenase (SDH), an OXPHOS enzyme encoded entirely by the nDNA. SDH staining is more sensitive than the modified Gomori trichrome in detecting mitochondrial proliferation. NADH-tetrazolium reductase (NADH-TR) stains mitochondria-rich fibers even more intensely, but the enzyme reaction is less specific than SDH for mitochondria. RRFs are seen in most patients with mtDNA defects and in some patients with nDNA mutations, but RRFs are neither a universal feature in mitochondrial disorders, nor are they specific for primary mitochondrial diseases. RRFs can occur in other neuromuscular diseases such as inflammatory myopathies or inclusion body myositis, as well as in normal aging. They also occur in the toxic myopathy caused by the drug zidovudine, where the underlying pathogenesis is drug-induced damage of the mtDNA. Mitochondrial proliferation in the smooth muscle of intramuscular vessels results in strongly SDH-reactive vessels in MELAS. The histochemical stain for cytochrome oxidase (COX) activity may be helpful. COX or complex IV of the mitochondrial respiratory chain has 13 subunits; three—COX I, II, and III—are encoded in mtDNA, and the others are encoded in the nuclear genome. COX may be absent in myofibers from patients with defects of mtDNA, mitochondrial transcription and translation, or assembly of complex IV. RRFs which are COX negative suggest impaired mitochondrial protein synthesis in the face of mitochondrial proliferation and are typically seen in mtDNA deletions. In the combined COX-SDH histochemical stain, COX-negative fibers with normal or high concentrations of SDH stain blue against a background of normal brown fibers that have both COX and SDH. Single-fiber polymerase chain reaction (PCR) from these fibers (RRF/SDH rich and COX negative) shows higher levels of mutated mtDNA molecules, suggesting that these mutations are deleterious. Discordance between RRF status and COX activity is not uncommon in muscle fibers in mitochondrial diseases. In patients with mutations in mtDNA protein-coding genes and defects in complex IV, RRF and many non-RRFs are COX negative or deficient, whereas in patients with defects of complex I or III and tRNA mtDNA point mutations, many RRFs with normal COX activity may be seen. SCO2 and SURF1 nDNA mutations, which cause complex IV deficiency, are generally associated with diffuse COX deficiency but without RRFs. The absence of either RRFs or COX-negative fibers does not rule out mitochondrial disease. For instance, patients with neuropathy, ataxia, and retinitis pigmentosa–maternally inherited Leigh syndrome (NARP-MILS) or LHON do not have RRF or COX-negative fibers.
Electron microscopy of muscle biopsy specimens from patients with mitochondrial diseases may reveal subsarcolemmal and intermyofibrillar proliferation of mitochondria and the presence of abnormal mitochondria in muscle fibers. Enlarged, elongated, irregular, and dumbbell-shaped mitochondria with hypoplastic and dystrophic cristae and paracrystalline inclusions (see Fig. 93.2 , B ) may be seen in a patient’s muscle biopsy with a diagnosis of mitochondrial disease. However, they are nonspecific and can be present in other neuromuscular disorders. Significant intermyofibrillar mitochondrial proliferation should be detectable by light microscopy in the modified Gomori trichrome, NADH-TR, and SDH stains. Isolated focal collections of mitochondria in the subsarcolemmal space or near the A–I junction in muscle fiber can be normal and should not be mistaken for pathological accumulation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here