Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
This chapter discusses the surgical management of common fractures in the lower extremity in adults. Basic techniques of fixation are discussed in Chapter 53 . The treatment of lower extremity fractures in children is discussed in Chapter 36 .
Nonoperative treatment generally is restricted to stable, minimally displaced fractures or to fractures in patients with significant comorbidities that preclude surgery. Intramedullary nailing has become the treatment of choice for most femoral and tibial diaphyseal fractures, including select fractures with proximal and distal metaphyseal involvement; plating is most commonly indicated for periarticular fractures; and external fixation is most commonly indicated for periarticular fractures, fractures with severe soft-tissue injury, and temporary fixation before definitive fixation with another method. The indications, contraindications, and limitations of these techniques are discussed for each type of lower extremity fracture.
Operative management of fractures of the hip and pelvis is discussed in Chapter 55, Chapter 56 . Fractures and dislocations of the foot are discussed in Chapter 89 .
Injuries around the ankle joint cause destruction of not only the bony architecture but also often the ligamentous and soft-tissue components. Treatment of the soft-tissue and ligamentous components is discussed in Chapter 83 . With fractures of the ankle, only slight variation from normal is compatible with good joint function. Radiographs after reduction should be studied with these requirements in mind: (1) the normal relationships of the ankle mortise must be restored, (2) the weight-bearing alignment of the ankle must be longitudinal axis of the leg, and (3) the contours of the articular surface must be satisfactorily reduced. The best results are obtained by anatomic joint restoration, and the method used to accomplish this may be either closed manipulation or open reduction and internal fixation (ORIF). For most fractures, the latter method most often ensures anatomic joint restoration and union.
Ankle fractures can be classified purely along anatomic lines as monomalleolar, bimalleolar, or trimalleolar. The Lauge-Hansen classification attempted to associate specific fracture patterns with the mechanism of injury and proposed a detailed classification, with each broad classification subdivided into four groups ( Box 54.1 ). According to this classification, most fractures are supination-eversion, supination-adduction, pronation-abduction, and pronation-eversion injuries. In this classification system, the term eversion is a misnomer; it more correctly should be external or lateral rotation . The first word in the designation refers to the foot’s position at the time of injury; the second word refers to the direction of the deforming force.
∗ Classification into fracture type (A to C) and group (1-3).
Transverse avulsion-type fracture of the fibula below the level of the joint or tear of the lateral collateral ligaments
Vertical fracture of the medial malleolus
Disruption of the anterior tibiofibular ligament
Spiral oblique fracture of the distal fibula
Disruption of the posterior tibiofibular ligament or fracture of the posterior malleolus
Fracture of the medial malleolus or rupture of the deltoid ligament
Transverse fracture of the medial malleolus or rupture of the deltoid ligament
Rupture of the syndesmotic ligaments or avulsion fracture of their insertions
Short, horizontal, oblique fracture of the fibula above the level of the joint
Transverse fracture of the medial malleolus or disruption of the deltoid ligament
Disruption of the anterior tibiofibular ligament
Short oblique fracture of the fibula above the level of the joint
Rupture of posterior tibiofibular ligament or avulsion fracture of the posterolateral tibia
Fracture of the medial malleolus
Fracture of the anterior margin of the tibia
Supramalleolar fracture of the fibula
Transverse fracture of the posterior tibial surface
The most common mechanism is supination-eversion (supination-external rotation). The identifying feature is a spiral oblique fracture of the distal fibula and a rupture of the deltoid ligament or fracture of the medial malleolus. The supination-adduction type of injury is characterized by a transverse fracture of the distal fibula and a relatively vertical fracture of the medial malleolus. The pronation-abduction mechanism produces a transverse fracture of the medial malleolus and a short oblique fracture of the fibula that appears relatively horizontal on the lateral radiograph. The pronation-eversion (pronation-external rotation) mechanism is characterized by a deltoid ligament tear or a fracture of the medial malleolus and a spiral oblique fracture of the fibula relatively high above the level of the ankle joint. Analysis of the fracture configuration, and hence the mechanism of forces producing the fracture, is especially important if closed reduction and immobilization are planned as definitive treatment. Generally, the mechanism of forces producing the fracture is reversed by the closed reduction manipulation; for example, if the fracture is produced by a supination, eversion, or external rotation mechanism, reduction is achieved by a pronation, inversion, or internal rotation manipulation.
Some authors caution against using the Lauge-Hansen classification alone to determine treatment and recommend that treatment be based on a clinical determination of stability. O’Leary and Ward described an abduction-external rotation mechanism that resulted in fracture of the medial malleolus and avulsion of the deltoid ligament, emphasizing the difficulty in determining the full extent of injury after high-velocity impact. This injury results from initial abduction and external rotation, followed by violent adduction that fractures the medial malleolus. Whitelaw et al. recommended evaluation of ankle joint stability by the anterior drawer and talar tilt tests after bony stabilization and surgical repair of any concomitant ligamentous disruption.
The Danis-Weber classification ( Fig. 54.1 ) is based on the location and appearance of the fibular fracture. Type A fractures are caused by internal rotation and adduction that produce a transverse fracture of the lateral malleolus at or below the plafond, with or without an oblique fracture of the medial malleolus. Type B fractures are caused by external rotation resulting in an oblique fracture of the lateral malleolus, beginning on the anteromedial surface and extending proximally to the posterolateral aspect. The injury may include rupture or avulsion of the anteroinferior tibiofibular ligament, fracture of the medial malleolus, or rupture of the deltoid ligament. Approximately 80% to 90% of lateral malleolar fractures fall into the Danis-Weber type B category. Type C fractures are divided into abduction injuries with oblique fracture of the fibula proximal to the disrupted tibiofibular ligaments (C-1) and abduction-external rotation injuries with a more proximal fracture of the fibula and more extensive disruption of the interosseous membrane (C-2). Type C injuries may involve a medial malleolar fracture or a deltoid ligament rupture. Fracture of the posterior malleolus may accompany any of the three types. The AO classification divides the three Danis-Weber types further for associated medial injuries ( Box 54.2 ). Malek et al. reported high interobserver and intraobserver reliability using the Danis-Weber classification system of 78% and 85%, respectively.

A1: isolated
A2: with fracture of medial malleolus
A3: with a posteromedial fracture
B1: isolated
B2: with medial lesion (malleolus or ligament)
B3: with a medial lesion and fracture of posterolateral tibia
C1: fracture of the fibula, simple
C2: diaphyseal fracture of the fibula, complex
C3: proximal fracture of the fibula
Authors have demonstrated that there is considerable interobserver variability between the classification systems for ankle fractures. In addition, although the Lauge-Hansen and Danis-Weber classifications have proved useful for understanding the mechanisms of injury and planning treatment, neither has been shown to have prognostic significance. Furthermore, the Lauge-Hansen classification scheme has demonstrated limitations in predicting associated soft-tissue injuries when evaluated with MRI.
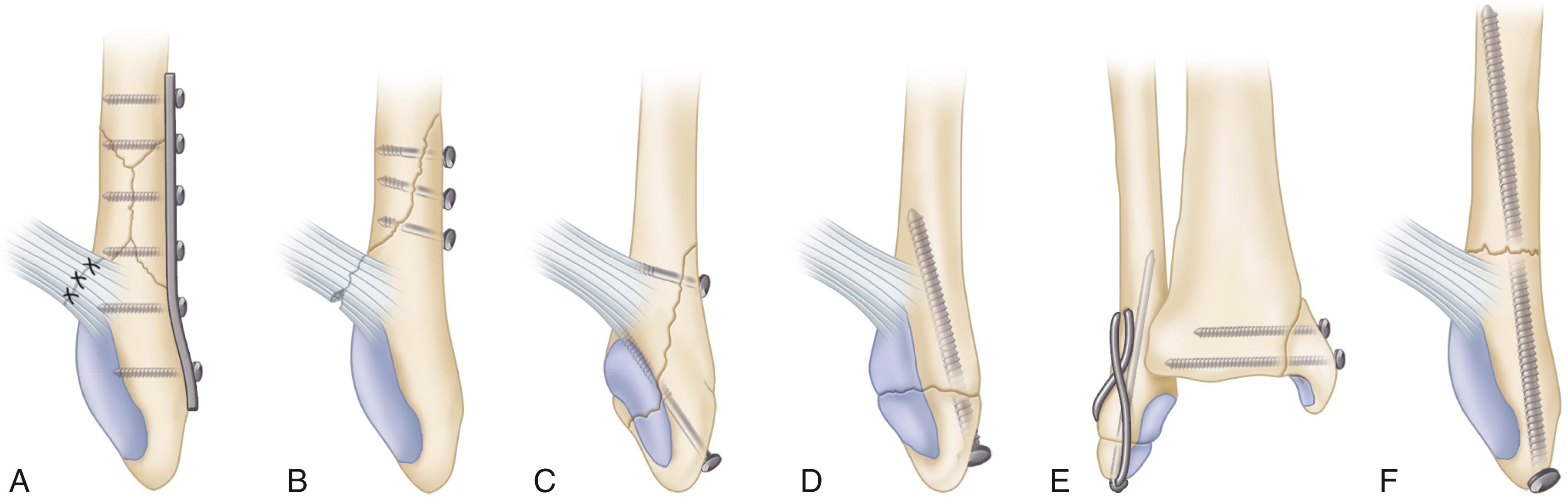
Nondisplaced fractures of the medial malleolus usually can be treated with cast immobilization; however, in individuals with high functional demands, internal fixation may be appropriate to hasten healing and rehabilitation. Herscovici et al. obtained a high rate of union and functional outcome with conservative management of isolated medial malleolar fractures. Displaced fractures of the medial malleolus should be treated operatively because persistent displacement allows the talus to tilt into varus. Avulsion fractures involving only the tip of the medial malleolus are not as unstable as fractures involving the axilla of the mortise and do not require internal fixation, unless displacement is significant. Delayed internal fixation can be done if symptoms warrant. Fixation of the medial malleolus usually consists of two 4-mm cancellous lag screws oriented perpendicular to the fracture. Some authors have advocated fixation with bicortical 3.5-mm lag screws, rather than 4-mm cancellous screws, because biomechanical data suggest increased construct strength ( Fig. 54.2A ).

Smaller fragments can be fixed with one lag screw and one Kirschner wire to prevent rotation ( Fig. 54.2B ). Fragments that are too small or comminuted for screw fixation can be stabilized with two Kirschner wires and a tension band ( Fig. 54.2C ). Alternatively, minifragment screws have become readily available and are an excellent option for stabilization of smaller fractures. Vertical fractures of the medial malleolus require horizontally directed screws or antiglide plating techniques ( Fig. 54.2D and E ). Dumigan et al. demonstrated that fixation of vertical medial malleolar fractures with neutralization plating is biomechanically advantageous.
Although stainless steel implants are used most commonly for medial malleolar fractures, the safety and efficacy of bioabsorbable implants have been investigated. The main theoretical advantage of these implants is that they reduce the incidence of late implant removal stemming from persistent prominence or tenderness around the screw heads. Although bioabsorbable implants have been used successfully, with no differences in outcomes noted between stainless steel and polyglycolide, drainage from sterile sinuses has been reported in 5% to 10% of patients, possibly related to the breakdown of polyglycolide. Also, in a series of 2528 patients, a 4.3% occurrence rate of clinically significant local inflammatory tissue reaction has been reported. Bioabsorbable implants are discussed in more detail in Chapter 53 .
Our preference is for metallic implants, typically screws or screw and plate combination, depending on the fracture morphology. Absorbable implants have a role in the treatment of associated articular fragments but are not a substitute for traditional internal fixation options.
Stress fractures of the medial malleolus usually present as localized pain, swelling, and tenderness over the medial ankle. Initially, they may not be apparent on radiographs but usually can be demonstrated on bone scan, CT, or MRI. Often stress fractures become apparent on follow-up radiographs. Shelbourne et al. recommended internal fixation for fractures that are immediately apparent on radiographs and cast immobilization for those only apparent on bone scans. Stress fractures of the medial malleolus have a high risk of progression to complete fracture, delayed union, or nonunion. Often aggressive treatment, including surgery, is necessary.
Although fractures of the lateral malleolus without significant medial injury are common, the indications for open reduction of these fractures are still controversial. The maximal acceptable displacement of the fibula reported in the literature has ranged from 0 to 5 mm. In most patients, 2 to 3 mm of displacement is accepted, depending on their functional demands. Displacement of the talus has been shown to accompany displacement of the lateral malleolus in bimalleolar ankle fractures; therefore, anatomic reduction of the lateral malleolus is necessary in these injuries. Biomechanical studies have shown that isolated fractures of the lateral malleolus do not disturb joint kinematics or cause talar displacement with axial loading, and long-term clinical follow-up studies of closed treatment of supination-external rotation stage II fractures have demonstrated 94% to 98% good functional results, even with 3 mm of fibular displacement. Results after operative treatment are similar to those of closed treatment of supination-external rotation stage II injuries, regardless of whether anatomic reduction has been obtained. If the stability of a lateral malleolar fracture is uncertain, stress radiographs can be obtained to detect displacement of the talus indicative of medial injury. This can be done by a manual or gravity stress evaluation. Koval et al. evaluated whether a positive stress test predicts the need for operative fixation of lateral malleolar fractures. In their study, all patients with positive findings of stress radiographs of the ankles had an MRI to evaluate the integrity of the deltoid ligament complex. Only complete ruptures required operative stabilization. Patients with partial disruptions had successful nonoperative management with a minimum 1-year follow-up. Others have proposed ultrasonographic evaluation of the deltoid ligament to differentiate between a bimalleolar equivalent fracture and an isolated lateral malleolar injury. Others have proposed that preoperative radiographic and CT findings are effective in predicting syndesmotic injuries in supination-external rotation type ankle fractures. Choi et al. suggested that a fracture height of more than 3 mm and medial joint space of more than 4.9 mm on CT, and fracture height of more than 7 mm and medial joint space of more than 4.0 mm on radiographs, is a good indicator of an unstable syndesmotic injury. However, the ideal preoperative diagnostic modality for assessing a medial-sided injury for decision-making regarding operative or nonoperative management remains unclear. We routinely obtain gravity or manual stress radiographs for appropriate injuries because of their simplicity.
Bimalleolar ankle fractures disrupt the medial and lateral stabilizing structures of the ankle joint. Displacement reduces the tibiotalar contact area and alters joint kinematics. Closed reduction can often be accomplished but not maintained in anatomic position as swelling subsides. Nonunion has been reported in approximately 10% of bimalleolar fractures treated by closed methods, although these are not always symptomatic. Twenty percent of bimalleolar fractures involve intraarticular injuries to the talus and tibia; these injuries go untreated when closed methods are used. Randomized, prospective, and long-term follow-up studies of bimalleolar or bimalleolar-equivalent ankle fractures have shown superior results of operative over nonoperative treatment. A long-term follow-up study also showed superior results after operative treatment of supination-external rotation stage IV fractures. Tile and the AO group recommended ORIF of both malleoli for almost all bimalleolar fractures.
For most displaced bimalleolar fractures, we also recommend ORIF of both malleoli. Most Weber type B and type C lateral malleolar fractures are stabilized with plate and screw fixation. In some patients, lateral implants in the ankle may become symptomatic; however, in one study only half the patients had relief of pain after implant removal. Posterior plating of Weber type B fractures of the lateral malleolus using an antiglide technique has been advocated to avoid the possibility of intraarticular screws, decrease the incidence of palpable implants, and provide a stronger construct. In a prospective series of 32 patients, there were no nonunions, malunions, wound complications, loss of fixation, or intraarticular or palpable screws. Four patients had transient peroneal tendinitis, and in two patients the plates were removed because of symptoms caused by a poorly placed lag screw. Weber et al. documented peroneal tendon lesions precipitated by posterior antiglide plating of the lateral malleolus. In their series, 30% of patients demonstrated peroneal tendon injury at the time of implant removal. However, only 22% of these patients had symptoms preoperatively. The authors concluded that the tendon lesions correlated with distal plate placement and screw insertion through the most distal hole of the plate and therefore advocated either avoiding distal implant placement or removing the plate early.
Implant prominence also may be decreased in some lateral malleolar fractures by using a lag screw–only technique ( Fig. 54.3 ). Several authors have reported successful treatment of lateral malleolar fractures with lag screw–only fixation, with no nonunions, loss of reduction, or soft-tissue complications. They cite less implant prominence and pain compared with patients who had plate fixation for similar injuries. Ideal candidates are patients younger than 50 years with a simple oblique lateral malleolar fracture and minimal comminution that allows the placement of two lag screws at least 1 cm apart.
Augmenting plate fixation with intramedullary Kirschner wires in osteopenic fibular fractures has been recommended in one study; 89% had minimal or no pain. In a biomechanical study, plates supplemented by Kirschner wires had an 81% greater resistance to bending than plates alone and twice the resistance to motion in torsional testing.
Operative treatment of periarticular fractures in general, ankle fractures in particular, probably is limited to two time periods: early and late. ORIF may be possible within the first 12 hours after injury but may not be possible again for 2 to 3 weeks because of excessive swelling, but this can be variable. Delayed closure and even skin grafting may be necessary when too much swelling exists at surgery. Equally good functional results have been found with immediate and delayed ORIF of Danis-Weber type B bimalleolar or bimalleolar equivalent ankle fractures, with no differences in complications, adequacy of reduction, range of motion, or operative time, although hospitalization was briefer and pain was diminished with immediate surgery in one study. Although delayed surgery may be technically more difficult, it is justified in patients with severe closed soft-tissue injury or fracture blisters. If open reduction of a fracture-dislocation is delayed, immediate closed reduction of the dislocation and splinting are mandatory to prevent skin necrosis.
Injuries to the syndesmotic complex continue to be a center of controversy and continuing focus. Syndesmotic injuries are most commonly caused by pronation-external rotation, pronation-abduction and, infrequently, supination-external rotation mechanisms (Danis-Weber type C and type B injuries). These forces cause the talus to abduct or rotate externally in the mortise, leading to disruption of the syndesmotic ligaments.
Anatomic restoration of the distal tibiofibular syndesmosis is essential. If the fibular fracture is above the level of the distal tibiofibular joint, this joint is assumed to be disrupted and must be anatomically reduced. In the past, internal fixation of all syndesmotic injuries was considered mandatory, but a cadaver study showed that disruption of the syndesmosis did not cause ankle instability if no medial injury was involved. If a medial lesion was present, syndesmotic injuries extending more than 4.5 cm proximal to the ankle joint altered joint mechanics, but syndesmotic injuries extending less than 3 cm proximal to the ankle joint did not. Syndesmotic disruptions of 3.0 to 4.5 cm produced variable results. These findings suggested that syndesmotic fixation was unnecessary if the disruption extended less than 3 cm above the plafond or if the medial and the lateral injuries were stabilized by fixation of the medial malleolus or repair of the deltoid ligament.
A prospective study evaluating syndesmotic screw fixation of Weber type C ankle fractures in which the lateral malleolar fracture was located within 5 cm of the ankle joint found that syndesmotic screw fixation was not necessary if the fracture was anatomically reduced and was immobilized for 6 weeks postoperatively. This has not yet been extensively evaluated clinically, however. Others have more recently proposed an “anatomic” restoration of the syndesmosis, citing repair of the deltoid ligament and posteroinferior tibiofibular ligament to be equivalent to trans-syndesmotic fixation from a functional outcome perspective, but with improved syndesmotic reductions noted.
There is general agreement that syndesmotic fixation is indicated for (1) syndesmotic injuries associated with proximal fibular fractures for which fixation is not planned and that involve a medial injury that cannot be stabilized and (2) syndesmotic injuries extending more than 5 cm proximal to the plafond. Whether syndesmotic fixation should be used in lateral malleolar fractures located 3 to 5 cm from the ankle joint in which the medial injury (deltoid ligament) is not repaired remains controversial. If a high fibular fracture associated with a syndesmotic injury is not fixed, restoration of fibular length can be difficult to determine accurately. Furthermore, fixation of midshaft fibular fractures with associated syndesmotic injuries demonstrates improved biomechanical characteristics when compared with syndesmosis fixation alone.
The integrity of the syndesmosis can be evaluated intraoperatively by performing an external rotation stress test and Cotton test. Cotton described this test to determine incompetence of the ankle syndesmosis intraoperatively. Distraction is applied to the fibula with a bone hook to try to separate it from the tibia, to which an opposing force has been applied to prevent tibial motion. If no significant motion is noted between the distal tibia and fibula, the syndesmotic ligaments are intact. If more than 3 to 4 mm of lateral displacement occurs, syndesmotic fixation is necessary. Intraoperative radiographs should show a clear space of less than 5 mm between the medial wall of the fibula and the lateral wall of the posterior tibial malleolus. Persistent widening indicates an unreduced syndesmosis. A cadaver study showed that syndesmotic disruption, measured as posterior displacement of the fibula on an external rotation stress lateral radiograph, correlated more closely with anatomic diastasis than did displacement on stress mortise radiographs. Stark et al. recommended intraoperative external rotation stress evaluation for unstable Weber B fractures after identifying a 39% incidence of syndesmotic instability after lateral malleolar fixation.
Various methods have been used to fix the syndesmosis. Most commonly screws are inserted through the lateral malleolus and into the distal tibia. These screws not only hold the joint anatomically reduced but also stabilize the lateral buttress of the ankle mortise. If screw fixation is chosen, either one or two 3.5-mm or 4.5-mm cortical screws are necessary; both have been found to be equivalent biomechanically. Two syndesmotic screws have been found to provide more secure fixation than one screw, and the use of two screws has been suggested in large or noncompliant patients. The syndesmotic screw should be placed through both cortices of the fibula and either one or two cortices of the tibia. In a survey of members of the Orthopaedic Trauma Association and the American Orthopaedic Foot and Ankle Society, Bava et al. sought to identify the current state of syndesmotic injury management. Fifty-one percent used 3.5-mm cortical screws, 24% used 4.5-mm cortical screws, and 14% routinely used a suture fixation device. Forty-four percent used one screw, 44% used two screws, and the remainder was undecided. The most common construct was use of 3.5-mm screws engaging four cortices that were routinely removed at 3 months. Bioabsorbable screws also have been used for fixation of the syndesmosis and have shown comparable results to metallic implants. Suture bridge techniques have gained in popularity. The proposed benefit is decreased implant issues requiring secondary intervention and dynamic stabilization. Retrospective data have demonstrated some loss of syndesmotic reduction at short-term follow-up. Implant prominence and suture knot irritation can still occur. A recent meta-analysis demonstrated improved functional outcomes as well as lower rates of broken implants and syndesmotic malreduction with the use of suture button fixation when compared to traditional syndesmotic screws.
Whether and when syndesmotic screws need to be removed are controversial subjects. Recommendations in the literature range from routine removal of the screw before weight bearing is allowed (in 6 to 8 weeks) to removal after the fracture has healed only if symptoms develop. Advocates of screw removal contend that the syndesmotic fixation disrupts ankle mechanics by restricting the normal external rotation of the fibula that occurs with dorsiflexion. Removing the screw too early may allow recurrent diastasis of the syndesmosis, however. Syndesmosis displacement has been reported when the screw was removed before weight bearing was allowed, and screw breakage has been reported with weight bearing with the screw in place. If tricortical fixation is used, the screw usually loosens rather than breaks and may not disrupt normal ankle mechanics. If fixation through four cortices is used, both ends of the screw can be removed easily if breakage occurs. In general, late diastasis of the syndesmosis creates a much more difficult clinical problem than broken screws; it is advisable to leave the screw in place for at least 12 weeks. Furthermore, another study revealed that at 1-year follow-up there was no difference in clinical outcome of patients with intact or removed syndesmotic screws. In fact, the subset with broken screws had improved clinical outcomes; therefore, the authors recommended not removing intact or broken syndesmotic screws. We have transitioned toward not routinely removing syndesmotic fixation unless the ankle is symptomatic, primarily with stiffness limiting dorsiflexion. However, a recent small series has questioned the effect of syndesmotic screw removal, citing no significant improvements in dorsiflexion after implant removal.
The syndesmosis must be anatomically reduced and held with provisional Kirschner wires or a reduction clamp before the syndesmotic screws are inserted. Miller et al. noted a significant decrease in syndesmotic malreductions in a cohort of patients in whom the syndesmosis was directly viewed during reduction. We also advocate open reduction of the syndesmosis with direct viewing. The reduction can therefore be performed manually and maintained with a reduction clamp, in contrast to using the clamp to effect reduction, which can introduce rotational malreduction. The screw should be positioned 2 to 3 cm proximal to the tibial plafond, directed parallel to the joint surface, and angled 30 degrees anteriorly so that it is perpendicular to the tibiofibular joint. If the screw is placed too far proximally, it may deform the fibula and cause the mortise to widen. If the screw is not parallel to the joint, the fibula may shift proximally. If the screw is not perpendicular to the tibiofibular joint, the fibula may remain laterally displaced. The AO group recommended a fully threaded syndesmotic screw in a neutralization mode or position; however, others have suggested that a lag screw provides more secure fixation. Traditionally, it was recommended to maximally dorsiflex the ankle during syndesmotic fixation to prevent postoperative limitation of motion; however, there are data refuting this finding and noting that maximal dorsiflexion may induce an external rotation moment risking malreduction. A cadaver study found no loss of dorsiflexion when lag screws were used for fixation of the syndesmosis with the ankle in plantarflexion. Others have illustrated that postoperative radiographic measurements are unreliable markers of syndesmotic reduction, which is better assessed with CT.
If a small plate has been used to fix the fibular fracture, this transfixing screw can be one of the screws used to secure the plate to the lateral side of the fibula ( Fig. 54.4 ). The reduced and fixed fibula must meet the three requirements for satisfactory function listed earlier in this section. Occasionally, the syndesmotic ligaments may avulse a small fragment of bone. If this is the case, syndesmotic stabilization can be accomplished by lag screw or minifragment fixation through this fragment.

Egol et al. evaluated outcomes after unstable ankle fractures with regard to the effects of syndesmotic fixation. They determined that at 1-year follow-up patients who underwent syndesmotic fixation had poorer outcomes than those who had malleolar fracture fixation alone.
If the fractured fibula is part of a bimalleolar fracture pattern, we usually reduce and internally fix the lateral malleolar or fibular fracture before fixing the medial malleolar component. The exception to this is a comminuted lateral malleolus as part of a bimalleolar or trimalleolar pattern. Occasionally, if comminution is severe, the lateral malleolus can be overreduced in the coronal plane, which inhibits anatomic reduction of the medial malleolar component of the injury. In this circumstance, it may be advisable to proceed with medial malleolar fixation initially.
Expose the lateral malleolus and the distal fibular shaft through a lateral longitudinal incision. Protect the superficial peroneal nerve. Alternatively, a posterolateral incision can be used, and the plate can be inserted with a posterior antiglide technique. The advantage is the ability to achieve distal bicortical fixation in a posterior to anterior direction. An incision placed slightly posteriorly has the theoretical advantage of not being positioned directly over a laterally based implant; however, direct exposure of the syndesmosis (if needed) may be made increasingly difficult. Expose the fibula in extraperiosteal fashion.
If the fracture is sufficiently oblique, if bone stock is good, and if there is no comminution, fix the fracture with one or two lag screws inserted from anterior to posterior to establish interfragmentary compression. Place the screws approximately 1 cm apart ( Fig. 54.5 ). The length of the screws is important; the screws must engage the posterior cortex for secure fixation but must not protrude far enough posteriorly to encroach on the peroneal tendon sheaths.

If the fracture is transverse, an intramedullary device can be used. Expose the tip of the lateral malleolus by splitting the fibers of the calcaneofibular ligament longitudinally.
Insert a Rush rod, titanium elastic nail, interlocking fibular rod, or other intramedullary device across the fracture line into the medullary canal of the proximal fragment. If using an intramedullary device, do not tilt the lateral malleolus toward the talus. The insertion point for intramedullary fixation tends to be in line with the medullary canal of the fibula; because the intramedullary appliance is straight, the lateral malleolus may be inadvertently tilted toward the talus, resulting in narrowing of the ankle mortise and reduced motion. This mistake can be avoided by contouring the intramedullary rod.
If the fracture is below the level of the plafond, if the distal fragment is small, and if the patient has good bone stock, use an intramedullary 3.5-mm malleolar screw for fixation. Rarely, a 4.5-mm lag screw can be used in large patients. Alternatively, orient the malleolar screw slightly obliquely to engage the medial cortex of the fibula proximal to the fracture.
In patients with poor bone quality, place Kirschner wires obliquely from lateral to medial through the distal and proximal fibular fragments and secure them further with a tension band wire. Alternatively, precontoured periarticular locking constructs, which are now readily available, may afford increased stability.
Anatomic reduction and maintenance of fibular length are necessary.
If the fracture is above the level of the syndesmosis, use a small fragment, one third tubular plate for fixation after anatomic reduction has been obtained; a 3.5-mm dynamic compression plate can be used in larger individuals or for more proximal fractures. The plates can be used to supplement lag screw fixation or to span a comminuted segment. In general, place three cortical screws in the shaft of the fibula above the fracture and two or three screws distal to the fracture. Unicortical cancellous screws are placed below the level of the plafond. If the plate is placed posterolaterally, it acts as an antiglide plate. Several commercially available precontoured fixed angle distal fibular locking plates provide alternative fixation options distally, however, often at the expense of increased implant prominence.
Syndesmotic fixation, if necessary, can be done as described in the section on syndesmotic injuries.
Make an anteromedial incision that begins approximately 2 cm proximal to the fracture line, extends distally and slightly posteriorly, and ends approximately 2 cm distal to the tip of the medial malleolus. We prefer this incision for two reasons: (1) the posterior tibial tendon and its sheath are less likely to be damaged, and (2) the surgeon is able to see the articular surfaces, especially the anteromedial aspect of the joint, which permits accurate alignment of the fracture and an opportunity to treat any associated impaction. However, this incision cannot be made extensile distally if associated foot injuries must be treated.
Handle the skin with care, reflecting the flap intact with its underlying subcutaneous tissue. The blood supply to the skin of this area is poor, and careful handling is necessary to prevent skin sloughing. Protect the greater saphenous vein and its accompanying nerve.
Usually the distal fragment of the medial malleolus is displaced distally and anteriorly and a small fold of periosteum commonly is interposed between the fracture surfaces. Remove this fold from the fracture site with a curet or periosteal elevator, exposing the small serrations of the fracture.
Debride small loose osseous or chondral fragments; large osteochondral fragments should be preserved and supported with a bone graft.
With a bone-holding clamp or pointed reduction tenaculum, bring the detached malleolus into the normal position, and, while holding it there, internally fix it with two 2-mm smooth Kirschner wires drilled across the fracture site as temporary fixation devices.
Check the fracture reduction with anteroposterior and lateral radiographs. If the reduction is satisfactory, remove one of the Kirschner wires and insert a 4-mm lag screw; remove and replace the other Kirschner wire ( Fig. 54.6 ). Alternatively, a drill with a 2.5- and a 3.5-mm bit can be used to create a path for the screws; a long pelvic drill bit will be necessary if bicortical lag screw fixation is chosen.

Carefully inspect the interior of the joint, particularly at the superomedial corner, to ensure the screw has not crossed the articular surface, and to treat any associated anteromedial impaction if present.
Use radiographs to verify the position of the screw and the fracture.
If the medial malleolar fragment is very small or comminuted, fixation with a standard screw may be impossible; in these cases, use several Kirschner wires, minifragment screws, or tension band wiring for fixation. Large vertical fractures of the medial malleolus that involve proximal comminution often require a buttress plate to prevent loss of reduction; a small, one third tubular plate usually is sufficient. To avoid wound complications, extreme care must be taken when applying bulky implants to this area of poor skin coverage.
The ankle is immobilized in a posterior plaster splint in neutral position and elevated. If the bone quality is good and the fixation is secure, the splint can be removed on the first postoperative visit and replaced with a removable splint or fracture boot. Range-of-motion exercises are begun. Weight bearing is restricted for 6 weeks, after which partial weight bearing can be started if the fracture is healing well and progressed accordingly.
If skin conditions, bone quality, comorbidities (e.g., diabetes), or other factors have prevented secure fixation, the fracture must be protected longer. The patient is placed in a short leg cast. The patient is not allowed to bear weight on the ankle until fracture healing is progressing well (8 to 12 weeks). A short leg walking boot is worn, and weight bearing is progressed.
A deltoid ligament tear accompanied by a fracture of the lateral malleolus is caused by the same mechanism that produces bimalleolar fractures, that is, supination with external rotation of the foot. Instead of the medial malleolus being fractured, however, the deltoid ligament is torn, allowing the talus to displace laterally ( Fig. 54.7 ). Usually the anterior capsule of the ankle joint is also torn. The deltoid ligament, especially its deep branch, is important to the stability of the ankle because it prevents lateral displacement and external rotation of the talus. A deltoid ligament tear should be suspected if a fracture of the lateral malleolus is accompanied by tenderness, swelling, and hematoma on the medial side of the ankle. Historically, medial-sided ankle tenderness would lead the clinician to suspect a deltoid ligament disruption in the presence of a lateral malleolar fracture. However, it has been established that there is no statistically significant relationship between medial tenderness and deep deltoid ligament rupture. A routine anteroposterior radiograph may show no lateral displacement of the talus, but a radiograph made when the ankle is stressed into supination and external rotation shows displacement and tilting of the talus in the ankle mortise and a wide medial clear space (>4 mm). This radiograph should be obtained with the ankle in neutral position. With the ankle in plantarflexion, the narrowest portion of the talus is within the mortise, which may appear to be wide even without injury. Alternatively, a gravity external rotation stress radiograph can be obtained.

Closed treatment of these injuries is difficult because the talus tends to shift in the mortise. A 1-mm lateral shift of the talus can reduce the effective weight-bearing area of the talotibial articulation by 20% to 40%, and a 5-mm shift can reduce it by 80%. If closed treatment is chosen, the patient must be followed closely for displacement. Optimal treatment of this injury is controversial. Provided that the condition of the skin and the patient’s age and general condition permit, ORIF of the fibula, with or without repair of the deltoid ligament, can be done. Nonoperative treatment also is feasible but requires careful radiographic monitoring to ensure maintenance of a congruent ankle mortise. If only the deltoid ligament tear is repaired, the talus is likely to become displaced laterally after surgery despite the use of a cast. If only the fibular fracture is repaired, the deltoid ligament may be caught between the medial malleolus and the talus, preventing accurate reduction, or the ligament may be relaxed after healing. One-year functional outcomes after nonoperative management are equivalent to ORIF of stress positive lateral malleolar fractures. However, complications may include residual medial clear space widening and lateral malleolar delayed union or nonunion.
Many surgeons advocate fixation of the fibula without routine exploration of the medial side, unless the reduction is blocked. We have found, however, that some fibers of the deltoid ligament can become trapped between the medial malleolus and the talus, even with a seemingly acceptable reduction, and this may lead to late displacement. Medial exploration requires little further surgical dissection; it allows the surgeon to ensure that the deltoid ligament has been cleared from the mortise, and it provides access for repair of the deltoid ligament if desired. We do not routinely repair the deltoid ligament and explore the medial side only in select cases, most often in injuries with a wide medial clear space and delayed presentation, because medial joint access may be required to restore a congruent tibiotalar joint.
Fractures of the lateral malleolus can be stabilized by several different methods, the most common being the use of a one third tubular plate and 3.5-mm cortical or locking screws. Long oblique fractures can be stabilized with lag screws alone. Fractures below the tibial plafond (Danis-Weber type A fracture) can be stabilized by a malleolar lag screw or with Kirschner wires and tension band fixation. We also have used oblique Kirschner wires placed from the distal fibular fragment into the tibia. Intramedullary devices can be used to stabilize transverse lateral malleolar fractures, but these rods do not prevent rotation. Interlocking intramedullary rods have been developed for the fixation of fibular fractures.
Make an anteromedial curved incision similar to, but slightly more distal than, the incision described for internal fixation of the medial malleolus (see Technique 54.2).
Identify the deltoid ligament, which is composed of two parts: a fan-shaped superficial portion and a short, heavy, deep portion. The superficial portion is almost always torn across its middle or is avulsed from the medial malleolus; the fanned-out inferior attachment of this superficial portion makes an inferior tear less likely.
Open the sheath of the posterior tibial tendon and displace the tendon to explore and repair the deep and more important portion of the deltoid ligament. This deep portion may be torn from the tip of the malleolus, avulsed from the side of the talus, or torn in the middle.
If the deep portion has been avulsed from the medial aspect of the talus, place two No. 0 nonabsorbable sutures through the ligaments and pass these through holes drilled diagonally across the body and neck of the talus to exit in the sinus tarsi area. Leave these sutures untied until the fibular fracture has been anatomically reduced and internally fixed. Alternatively, suture anchors can be used.
Make a lateral longitudinal incision and expose the lateral malleolus as described.
Anatomically reduce and fix the fracture of the lateral malleolus as described previously (see Technique 54.1).
When the lateral malleolar fracture has been rigidly fixed, snugly tie the sutures already placed in the deltoid ligament and passed through the talus.
Close the lateral incision.
Return to the medial side of the ankle, replace the posterior tibial tendon in its sheath, and close the sheath.
Repair the superficial portion of the deltoid ligament with multiple interrupted, nonabsorbable sutures.
If the entire deltoid ligament has been avulsed from the medial malleolus, drill two or three small holes in the malleolus and place interrupted sutures through them and the avulsed end of the ligament; alternatively, suture anchors can be used.
Place the sutures in the ligament, but do not tie them before completing the fixation of the lateral malleolus because they may be torn loose during that procedure. If the lateral malleolus is fixed before these sutures are placed, repairing the ligament becomes much more difficult.
The postoperative care is the same as that described after Technique 54.2.
Anatomic reduction of fractures around the ankle is essential for acceptable functional results. One lesion that appears innocent but is nevertheless crippling if left untreated is the widened ankle mortise. Specifically, a widened ankle mortise is lateral displacement of the talus and the fibula that leaves an interval between the talus and the intact medial malleolus. In this lesion, the deltoid ligament has been avulsed or torn and either the distal fibula has been fractured or the distal tibiofibular ligaments have been torn.
It may be impossible to reduce the gap by closed methods. The end of an avulsed deltoid ligament may be caught between the medial malleolus and the talus ( Fig. 54.8 ). Less often, a deltoid ligament tear or an avulsion fracture of the tip of the medial malleolus may release the posterior tibial tendon and sometimes the tibial nerve and posterior tibial vessels and allow them to become trapped between the medial malleolus and the talus ( Fig. 54.9 ). These obstructions must be removed surgically, and then the deltoid ligament tear or avulsion and any fracture of the lateral malleolus can be repaired (see Technique 54.1).
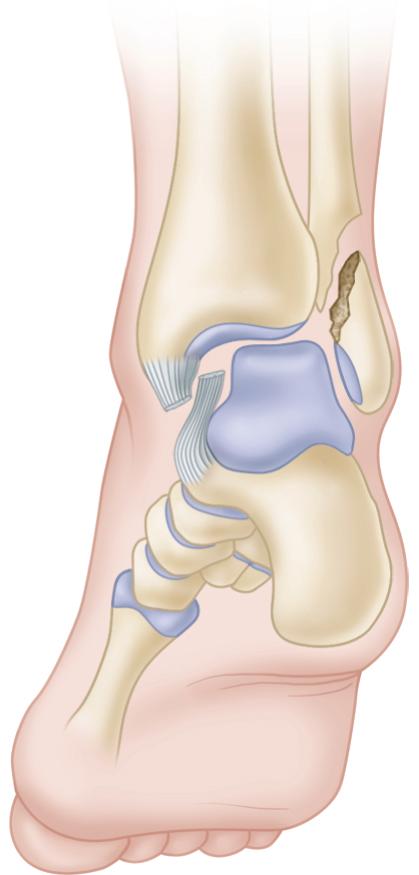

Occasionally, the posterior tibial tendon is interposed between the torn parts of the deltoid ligament and impairs healing ( Fig. 54.10 ). In more severe fracture-dislocations, the posterior tibial tendon may be displaced far laterally between the distal tibia and fibula.

A lesion described by Bosworth ( Fig. 54.11 ) may be the cause of failure to reduce a posterior fracture-dislocation of the ankle. The distal end of the proximal fragment of the fibula may be displaced posterior to the tibia and locked by the tibia’s posterolateral ridge; the bone cannot be released by manipulation because of the pull of the intact interosseous membrane. The fibula is exposed, and a periosteal elevator is used to release the bone; considerable force may be necessary. The fibular fracture is fixed as described in Technique 54.1.

Trimalleolar fractures require open reduction more often than any other type of ankle fracture. The results of treatment of trimalleolar fractures usually are not as good as the results obtained for bimalleolar fractures. Trimalleolar fractures usually are caused by an abduction or external rotation injury. In addition to fractures of the medial malleolus and fibula, the posterior lip of the articular surface of the tibia is fractured and displaced, allowing posterior and lateral displacement and external rotation with supination of the foot. The medial malleolus may remain intact, with a tear of the deltoid ligament occurring instead of a malleolar fracture.
The same principles and indications for open reduction as previously outlined for bimalleolar fractures apply to trimalleolar fractures. Indications for open reduction of the posterior malleolus or posterior tibial fragment depend on its size, displacement, and, most important, its perceived contribution to stability of the injured ankle. A 50-degree external rotation view can be used for the most accurate assessment of the size and displacement of the posterior malleolar fragment. Historically, if the fragment of the posterior malleolus involves more than 25% to 30% of the weight-bearing surface, it should be anatomically reduced and held with internal fixation. Often, satisfactory reduction of the posterior tibial fragment, if small, occurs with anatomic and rigid fixation of the fibula because this fragment most often is posterolateral and attached to the fibula by the posterior tibiofibular ligament. Gardner et al. showed in a cadaver model that fixation of the posterior malleolus imparts syndesmotic stability to a greater extent than syndesmotic screws. If the posterior tibial fragment is small, a proximally displaced position may be of little consequence, but even the slightest posterior subluxation of the talus on the articular surface of the tibia is unacceptable. If there is a persistent step-off or gap of more than 2 to 3 mm or persistent posterior instability, open reduction is warranted. The posterior and proximal displacement of the tibial fragment creates an offset at the fracture. With the foot displaced posteriorly, this irregularity in the articular surface of the tibia is brought against the weight-bearing surface of the talus, and with motion and weight bearing severe traumatic arthritis develops. We routinely treat the posterior malleolus as part of the ankle injury complex because of its contribution to ankle stability. Very small fractures can be treated nonoperatively if ankle stability is proven, and frequently reduce well with anatomic fibular reconstruction. Our preference for larger displaced fragments is ORIF, and the decision for fixation should be made in the context of the extent of articular involvement and the expected contribution to restoring ankle stability.
Fractures of the posterior lip of the tibia usually are associated with fractures of the medial and lateral malleoli, and the approach to the posterior malleolus may depend on what additional open reductions are required. Most often, an anteromedial incision is made to fix a fractured medial malleolus, and a posterolateral incision is used to fix the posterior lip of the tibia and the lateral malleolar fracture. If the posterior fragment is located more medially, a posteromedial approach can be used to treat the medial and posterior malleolar fractures. Alternatively, a separate posteromedial or posterolateral incision can be made adjacent to the Achilles tendon to allow indirect or direct reduction.
Preoperative CT scans are mandatory for evaluation of fracture morphology, including size, location, and any associated marginal impaction of the posterior malleolar fragment. The posterior lip fracture often reduces after reduction of the fibula. If this does not occur and internal fixation is necessary because of the size of the fragment or the presence of posterior instability, the posterior lip fracture should be reduced and internally fixed before reduction of either the medial or the lateral malleolus. The objective is to restore anatomically the articular surface of the distal tibia. Reduction and fixation of either malleolus reduce the distractibility of the tibial and talar joint surfaces, making exposure more difficult. Distraction of the tibiotalar joint can be increased by inserting a large Steinmann pin transversely through the calcaneus, to which a traction bow is applied. An assistant can distract the tibiotalar joint significantly using this technique if neither malleolus has been reattached. Alternatively, a large distractor may be of benefit. If the posterior malleolar fragment is small, a screw directed from posterior to anterior or a fully threaded screw placed by lag technique should be used because a partially threaded screw placed from anterior to posterior may leave screw threads crossing the fracture site. Preoperative planning, including CT scans, facilitates understanding of the orientation of the posterior malleolar segment and therefore aids in selection of an appropriate surgical approach and fixation. The frequent posterolateral position of this fragment often permits fixation through a posterolateral approach.
Proper preoperative templating and review of imaging are necessary.
The posterior malleolus can be exposed through a posteromedial incision by incising the posterior tibial tendon sheath adjacent to the posterior border of the tibia.
Displace the medial malleolar fragment and dissect subperiosteally to gain access to the posterior malleolus. Although this approach permits direct access to a medially located posterior malleolus, fixation may be limited to screws.
Insert two Kirschner wires 1 to 3 cm above the anterior tibial lip, directed from anterior to posterior, to engage the posterior fragment.
When this temporary fixation has been achieved, make a hole from anterior to posterior with the appropriate size drill bit through both fragments; measure with a depth gauge; and insert a malleolar, small fragment screw, tightening the fragments together to produce interfragmentary compression ( Fig. 54.12A-D ).

If a conventional screw is used, overdrill the anterior cortex so that a lag effect is achieved.
Remove the Kirschner wires and anatomically reduce and internally fix the lateral and then the medial malleolus.
If the posterior malleolar fragment is located more laterally, use a posterolateral incision. Make a 7.5-cm incision lateral to the Achilles tendon. Protect the sural nerve.
Retract the Achilles tendon medially and the peroneal tendons laterally to expose the posterior malleolus.
Establish the normal articular relationship between the talus and the tibia by anterior traction on the foot and by adduction and inversion.
Correct the proximal displacement of the posterior lip of the tibia by placement of a joystick for manipulation and fix the fragment by inserting one or two lag screws from posterior to anterior into the tibial metaphysis, or alternatively place a posterior antiglide plate (see Fig. 54.12E ), which is preferred because of its biomechanical advantage.
After the posterior fracture has been fixed, repair the fractures of the medial and lateral malleoli as previously described (see Techniques 54.1 and 54.2).
Carefully inspect the articular surface of the tibia through the anteromedial incision to confirm anatomic reduction of the articular surface.
The postoperative care is the same as for internal fixation of bimalleolar fractures (see Techniques 54.1 and 54.2).
These fractures can be viewed as transitional fractures between traditional ankle fractures and pilon fractures, which typically are the result of axial loading. The treatment of fractures of the anterior margin of the tibia is about the same as that for the posterior margin, although in reverse. The fractures differ in one respect, however. Because fractures of the anterior margin usually are caused by a fall from a height that results in the foot and ankle being forcefully dorsiflexed, crushing of the articular surface of the tibia is likely to be more severe in these fractures. Perfect restoration of the articular surface of the tibia may be impossible. When necessary, associated fractures of the medial and lateral malleoli are treated as described previously. Surgery should be performed within the first 24 hours or delayed until the soft tissue is in good condition. CT is instrumental in preoperative templating to be prepared for treating segments of marginal impaction.
Expose the fracture through an anterolateral incision 7.5 to 10 cm long (see Chapter 1 ), retract the extensor tendons medially, and continue the dissection until the entire anterior surface of the ankle joint has been exposed.
Remove small, loose fragments of bone, preserving intact as much of the articular surface as possible.
Reduce the anterior subluxation of the talus, appose the large anterior triangular fragment to the shaft of the tibia in its normal position, and transfix it with one or two screws or with threaded Kirschner wires if the fragments are small. If the fragment is comminuted, it may be necessary to apply a low-profile, small fragment buttress plate or span the ankle temporarily with an external fixator. Elevation of depressed articular segments can be supported with grafting.
Postoperative care is the same as for internal fixation of bimalleolar fractures (see Technique 54.2).
Although malleolar fractures historically have been considered to be relatively benign injuries, operative treatment in patients with complicated diabetes mellitus is associated with significant complications. Significantly increased risk of unplanned readmission, unplanned reoperation, and mortality has been demonstrated. These patients often are older and may have peripheral vascular disease or peripheral neuropathy, which complicates their care. Complications have been reported to be as high as 43% compared with 15.5% in patients without diabetes. Complications may include deep and superficial infection, loss of fixation, malunion, wound necrosis, and amputation. Although diabetic patients treated nonoperatively have shown a high frequency of loss of reduction and malunion, they can be relatively minimally symptomatic. Nonoperative treatment is recommended for malleolar fractures in older diabetic patients with low functional demands. However, if surgical treatment of the ankle fracture is indicated, it should not be delayed or avoided simply because the patient is diabetic. Inadequate immobilization may lead to rapidly developing neuropathy. If the ankle fracture is nondisplaced or minimally displaced and has a stable configuration, closed management with prolonged casting is an acceptable alternative, but only with close supervision. If the fracture is displaced, and either considerable manipulation is necessary to reduce it or molding is required to maintain the reduction, an open approach with internal fixation is recommended. Regardless of the method of treatment, prolonged immobilization often is necessary to prevent the development of neuropathic complications.
In contrast, a study by Guo et al. compared patients with preoperatively neglected type 2 diabetes and a nondiabetic matched cohort and found no significant increase in postoperative infection after immediate operative stabilization of closed ankle fractures. Jones et al. demonstrated that operatively treated ankle fractures in diabetic patients without comorbidities had comparable complication rates to nondiabetic patients. The presence of diabetic comorbidities and, in particular, a history of Charcot arthropathy increased the likelihood of complications. In one large series, Costigan et al. reported 84 patients who underwent ORIF for acute closed ankle fractures. Open fractures, insulin dependence, patient age, and fracture type affected outcome, and 83% of patients with absent pedal pulses and 92% of patients with preoperative neuropathy developed complications. Others have shown that operatively treated ankle fractures in diabetic patients are associated with higher rates of mortality and length of hospital stay, as well as total hospital charges. Ayoub reported the results of tibiotalar arthrodesis in 17 diabetic patients with unstable bimalleolar ankle fractures complicated by Charcot arthropathy. Results were better with surgery within 3 to 6 months of onset, with absence of dense peripheral neuropathy, and in patients with satisfactory extremity oxygenation. Amputation was required in 17.6% of patients.
We typically use standard fixation techniques in patients with controlled diabetes and unstable ankle fractures. However, in certain patients who are deemed at increased risk for fixation failure, the fixation strategy may be modified in the interest of obtaining rigid fixation. These include bicortical medial malleolar fixation, placement of multiple transfibular or transtibial syndesmotic position screws, adjuvant external fixation, and application of locking plate technology ( Fig. 54.13 ).

Open ankle fractures caused by indirect injury are two to four times more likely to be open medially than laterally. Several studies have shown the advantages of primary internal fixation of open ankle fractures, including Gustilo type III wounds, compared with either closed immobilization with delayed fixation or immediate provisional fixation with Kirschner wires. We also prefer immediate internal fixation after surgical debridement. If the wound is severely contaminated, a temporary external fixator can be placed spanning the ankle and open reduction can be done when the wound is judged to be clean and swelling has decreased. Ngcelwane noted dirt and grass at the syndesmosis in some medial wounds, possibly sucked in by the vacuum created by dislocation of the ankle; he recommended a lateral incision for cross irrigation, especially for displaced Danis-Weber types B and C fractures with gas shadows. In addition to internal fixation, a temporary external fixator that spans the ankle joint can be used to make wound care easier. The fixator can be removed when soft-tissue healing is complete.
Although most patients (80%) can be expected to return to work after the fracture has healed, only approximately 18% return to their preinjury recreational level. The rate of deep infection in open ankle fractures is approximately 5%. We have found that open ankle fractures, especially fracture-dislocations, in diabetic patients, especially patients with neuropathy, are problematic and frequently become infected or have implant failure, sometimes resulting in amputation. Supplemental external fixation is advisable in these patients.
Childress described a method that may be useful for unstable fracture-dislocations in the ankle when the usual treatment is inadvisable. This situation most often arises when an abrasion or superficial infection is present where an incision usually would be made for open reduction. Childress recommended this technique only as a last resort but found it useful several times. The ankle is stabilized by a pin inserted through the calcaneus into the medullary canal of the tibia. Our preferred method of stabilization is application of a uniplanar external fixator with inclusion of the forefoot if warranted to prevent forefoot equinus posturing should a frame become necessary for definitive management. Use of a percutaneous tibiotalocalcaneal pin has been reserved for very rare instances in which existing implants preclude external fixation placement and stability is necessary for soft-tissue protection. We have modified the procedure so that the pin is directed to exit the anterior distal tibial metaphysis to facilitate later extraction should the implant fail. This pin can be directed from the calcaneal tuberosity, posterior to the talus, to enter the distal tibia, therefore remaining extra articular. We have used this technique to supplement more standard fixation when the patient is at risk for equinus contracture of the ankle or for stabilization of an injury before debridements.
(CHILDRESS)
Tape a Kirschner wire longitudinally on the medial side of the ankle exactly in the midline.
Reduce the fracture-dislocation and obtain anteroposterior and lateral radiographs of the ankle.
Using the Kirschner wire as seen in the radiograph as a guide, insert a 2.8-mm, smooth Steinmann pin in the midline on the sole 2.5 cm posterior to the calcaneocuboid joint and aim it toward the center of the tibia.
Advance the pin about 10 cm into the distal tibia and check the position of it and the fragments by radiographs. Leave 1.3 cm of the pin protruding through the sole and pad it well.
Apply a long leg cast that does not incorporate the end of the pin.
The cast is removed at 4 to 6 weeks, and a short cast is applied. The pin is removed at 4 to 8 weeks, depending on the stage of healing and the original stability of the fracture. Weight bearing is not allowed until the pin has been removed, and then only as healing progresses.
Tibial pilon fractures encompass a spectrum of skeletal injury ranging from fractures caused by low-energy rotational forces to those precipitated by high-energy axial compression forces usually resulting from motor vehicle accidents or falls from a height. Rotational variants typically have a more favorable prognosis, whereas high-energy fractures frequently are associated with open wounds or severe, closed, soft-tissue trauma. The fracture may have significant metaphyseal or articular comminution or diaphyseal extension. Classification of these fractures is important in determining their prognosis and choosing the optimal treatment. The fibula is fractured in 85% of these patients, and the degree of talar injury varies.
Rotational fracture of the ankle can be viewed as a continuum, progressing from single malleolar fractures to bimalleolar fractures to fractures involving the distal tibial articular surface. Lauge-Hansen described a pronation-dorsiflexion injury that produces an oblique medial malleolar fracture, a large anterior lip fracture, a supraarticular fibular fracture, and a posterior tibial fracture. Giachino and Hammond described a fracture caused by a combination of external rotation, dorsiflexion, and abduction that consisted of an oblique fracture of the medial malleolus and an anterolateral tibial plafond fracture. These fractures generally have little comminution, no significant metaphyseal involvement, and minimal soft-tissue injury. They can be treated similarly to other ankle fractures with internal fixation of the fibula and lag screw fixation of the distal tibial articular surface through limited surgical approaches.
Classification systems have been devised to describe more accurately the wide range of distal tibial articular fractures. The AO/OTA classification system provides a comprehensive description of distal tibial fractures. Type A fractures are extraarticular distal tibial fractures, which are subdivided into groups A1, A2, and A3, based on the amount of metaphyseal comminution. Type B fractures are partial articular fractures in which a portion of the articular surface remains in continuity with the shaft; these are subdivided into groups B1, B2, and B3, based on the amount of articular impaction and comminution. Type C fractures are complete metaphyseal fractures with articular involvement; these are subdivided into groups C1, C2, and C3, based on the extent of metaphyseal and articular comminution ( Fig. 54.14 ).

Another commonly used system is that proposed by Rüedi and Allgöwer, which divides plafond fractures into three categories. Type I fractures are nondisplaced cleavage fractures that involve the joint surface; type II fractures have cleavage-type fracture lines with displacement of the articular surface but minimal comminution; type III fractures are associated with metaphyseal and articular comminution.
Studies have shown these classification systems to have only moderate interobserver reliability; nevertheless, they have proved to have some prognostic value. Treatment of fractures with little displacement or comminution (Rüedi and Allgöwer type I and type II spiral fractures) has yielded much better functional results with far fewer complications than treatment of the more severe fracture patterns (Rüedi and Allgöwer type III, AO types B3 and C3).
Intraarticular fractures of the distal tibia have been treated by a variety of methods, including plaster immobilization, traction, lag screw fixation, ORIF with plates, and external fixation with or without limited internal fixation. A variety of external fixators have been used: traditional half-pin fixators spanning the ankle, articulated half-pin fixators that allow ankle motion, half-pin fixators that do not span the ankle, and hybrid fixators that combine tensioned wires with half-pins in the tibial diaphysis and do not span the ankle joint. Hybrid frames may be composed of rings proximally and distally (Ilizarov, Monticell-Spinelli).
As a result of disappointing results after acute definitive management, staged protocols have been advocated consisting of temporary external fixation spanning the ankle joint, followed by ORIF with plates and screws after the condition of the soft tissues has improved, usually 2 to 3 weeks after injury. Percutaneous or minimally invasive plating techniques have been developed. Primary arthrodesis has been performed in selected severe fractures with extensive articular comminution and talar injury. In these patients, functional results are likely to be poor with attempts at anatomic restoration, which may not be feasible. There is some overlap in the indications for these differing methods of treatment. The surgeon’s preference and experience should play a role in preoperative decision making.
Several variables must be considered when devising a treatment strategy. One must understand the mechanism of injury because this can reflect on the amount of associated soft-tissue damage. The fracture type should be determined according to the amount and location of displacement, comminution, impaction, and diaphyseal involvement. Fracture extension into the tibial diaphysis and ipsilateral fractures of the foot or tibia may influence the choice of treatment. Some authors have advocated early limited fixation of the fracture extensions into the diaphyseal region for certain fractures to facilitate later staged reconstruction. Radiographs of the contralateral ankle may be beneficial as a template for articular reconstruction.
In addition to plain radiographs, CT scans are extremely useful for determining accurately the direction of fracture lines, the size and displacement of articular fragments, and the extent of articular comminution and impaction. CT scans also are useful in planning surgical incisions and trajectory for screw or fine wire fixation. Traction can be applied using a calcaneal traction pin and Bohler frame or a uniplanar spanning external fixator. Radiographs in traction show the extent to which the articular surface can be reduced by ligamentotaxis. As a result, typically the CT scan should be obtained after the application of an external fixator. Unless a form of external fixation may be considered as definitive treatment, an acutely chosen preoperative CT scan can assist in planning placement of limited internal fixation. Any impacted segments need to be reduced by open or limited open methods. Anatomic reduction may be impossible in some severely comminuted fractures.
The severity of soft-tissue injury should be clearly defined. Open injuries can be classified according to the Gustilo system. Although less obvious than open wounds, closed soft-tissue injuries can be quite severe and can adversely affect the functional outcome, especially if unrecognized.
The extremity should be examined carefully for signs of vascular injury, swelling, fracture blisters, soft-tissue crushing, closed degloving, and compartment syndrome. Blood-filled fracture blisters indicate more extensive cutaneous damage than blisters filled with clear fluid. The Tscherne classification system can be used to describe closed soft-tissue injury. Patient characteristics, such as smoking, alcoholism, peripheral vascular disease, and diabetes, should also be considered.
The ultimate goals of tibial pilon fracture management are restoring an anatomic articular surface, restoring mechanical alignment, maintaining joint stability, achieving fracture union, and regaining functional and pain-free weight bearing and motion, while avoiding complications. Ideal results are not attainable in some patients because of the severity of articular comminution and soft-tissue injury or comorbidities. Poor prognostic indicators are articular comminution (AO C3 and Rüedi-Allgöwer type III fracture), talar injury, severe soft-tissue injury, poor reduction of the articular surface, unstable fixation, and postoperative wound infection.
Many investigators have reported poorer results in the more severe fracture patterns. Anatomic reduction has a better prognosis than a fair or poor reduction but does not guarantee a good result. Some degree of arthrosis has been shown to develop in anatomic reductions; however, in fair or poor reductions (>2 mm of displacement), more severe arthrosis can be expected. In a series of 37 AO type B3 and C3 fractures treated with external fixation and delayed internal fixation of the articular surface, Dickson, Montgomery, and Field identified a subset of patients with “ground-glass” comminution, which was defined as more than three pieces of articular surface less than 2 mm in size seen on CT scan. Posttraumatic arthritis developed in 10 (38%) of the 26 ankles with ground-glass comminution and in none of the ankles without it. Overall, 17% of anatomically reduced fractures (5 of 29) developed arthritis, whereas five of seven nonanatomically reduced fractures developed arthritis.
In recent years, there has been a greater emphasis on functional outcome. Although there is no disagreement that anatomic reduction is desirable, the impact of anatomic reduction on overall outcome is less clear. An analysis of the effect of severity of injury and fracture reduction on clinical outcome found no correlation with clinical ankle score. In addition, no correlation has been found between radiographic arthrosis and clinical results. Williams et al. found that although radiographic arthrosis was related to injury severity and quality of reduction, there was no significant relationship between these variables and the 36-Item Short Form Health Survey (SF-36) score, clinical ankle score, or return to work. Functional outcome was more closely related to socioeconomic factors. Patients with a higher level of education were more likely to return to work and had higher ankle scores. The predictors of clinical outcome seem to be multifactorial and are not fully understood.
Other studies have found pilon fractures to have a negative long-term effect on general health as measured by the SF-36. Stiffness, swelling, persistent pain, and the use of an ambulatory aid were some of the reasons. Forty-three percent of previously employed patients were no longer employed, and of this subgroup, 68% attributed their inability to work to the pilon fracture. Poorer results were correlated with having two or more comorbidities and treatment with external fixation. Fractures treated with external fixation had more impairment of range of motion and worse pain scores than fractures treated with ORIF. External fixation tended to be used in more severe injuries (AO type C).
Factors to consider in the formulation of a treatment plan include the fracture pattern, soft-tissue injury, patient comorbidities, fixation resources, and surgical experience. The degree of articular comminution, talar damage, and soft-tissue injury is dictated by the injury; however, the surgeon does have some influence over other prognostic factors. The goal should be to obtain the best possible articular reduction and axial alignment while respecting the soft tissues. If the articular surface does not reduce by ligamentotaxis, some form of open reduction usually is indicated after the soft tissues have recovered. Fracture union can be enhanced by bone grafting areas of impaction, bone loss, or extensive metaphyseal comminution. The frequency of wound healing problems and infection can be decreased by recognizing open and closed soft-tissue injury and not operating through compromised soft tissue. In some cases, the surgeon must achieve a balance between the goals of anatomic reduction and prevention of wound complications. Anatomic reduction often is more difficult to achieve after a delay of 2 to 3 weeks; however, surgical incisions through swollen, contused soft tissues can lead to disastrous results, which may require free tissue transfer or even amputation.
Nondisplaced fractures, such as AO types A1, B1, and C1, have been treated successfully with operative and nonoperative methods. These are the only fracture types in which cast immobilization alone may be suitable. If casting is chosen, the patient should be observed closely for displacement, and weight bearing should be restricted for at least 8 to 12 weeks if the joint is nonarthritic. Calcaneal traction alone often is helpful in temporarily stabilizing severe fractures associated with soft-tissue swelling, but it seldom is used for definitive treatment. External fixation accomplishes the same goal of fracture reduction through ligamentotaxis and allows the patient to be mobilized. Limited fixation with 3.5- or 4.0-mm screws, inserted after either percutaneous or limited open reduction, combined with external fixation or minimally invasive plating techniques may be adequate treatment for AO types B1, B2, and stable C1 fractures.
For displaced fractures, operative treatment has been found to be superior to nonoperative treatment. Rüedi and Allgöwer popularized the technique of ORIF with plates and screws for tibial pilon fractures in the 1960s. This technique follows the AO principles of anatomic reduction, rigid stabilization, and early motion. The fibula is reduced first and stabilized with a plate. Then the articular surface of the tibia is reduced and provisionally fixed with Kirschner wires through an anteromedial incision. Metaphyseal defects are filled with bone graft, and the fracture is stabilized with a medial buttress plate. Rüedi and Allgöwer reported 70 good or excellent results in 75 fractures treated with this method. Only three fractures were open, and almost half were low-energy, sport-related injuries.
In the 1980s to the mid-1990s, series involving larger percentages of open and high-energy injuries reported far fewer successful results and a high incidence of complications with this technique, especially in Rüedi and Allgöwer type III (AO type C3) fractures. When complications occur, they can be devastating. Free tissue transfer often is necessary to salvage the extremity, and the final result in some cases is amputation. Satisfactory results in Rüedi and Allgöwer types I and II fractures have been reported to be between 60% and 82% and 37% and 40% in type III fractures treated with ORIF, respectively. Infection rates after type III fractures have been reported to be 12.5% to 37%.
Plate and screw fixation has been associated with more frequent wound breakdown and infection than in similar fractures treated with external fixation. Watson et al. reported more excellent and good results at 5-year follow-up with external fixation (81%) than with open plating (75%) in 94 pilon fractures. They based their treatment choices on the severity of the soft-tissue injury: Tscherne grade 0 and grade I were treated with plating, and grade II and grade III and open fractures were treated with external fixation.
The high incidence of wound complications after ORIF of pilon fractures reported in the 1980s and in the early to mid-1990s is attributable to operating through a poor soft-tissue envelope. In an effort to improve overall results, protocols for staged ORIF were developed, and these have decreased the frequency of wound complications and infections associated with plating of pilon fractures. Initially, the fibula is plated and an external fixator is placed, spanning the ankle. Preoperatively, the proposed incision for tibial reduction is planned and the fibular incision is placed so that the skin bridge between the two incisions is at least 7 cm, although smaller soft-tissue bridges have been shown to be tolerable. If the soft tissue overlying the fibula is compromised, fibular plating should be delayed. External fixation pins should be placed well away from planned incisions and out of the zone of injury and potential plate fixation.
Watson et al. described a two-pin “traveling traction” type of external fixator that is useful in this situation. An AO delta frame spanning the ankle or a medial half-pin fixator consisting of one half-pin in the talus, one half-pin in the calcaneus, and two half-pins in the tibial shaft have been recommended; however, the use of a talar pin may compromise certain surgical approaches. Tibial pilon open reduction is done after the soft tissues have improved and swelling has decreased (usually between 10 and 21 days). Skin wrinkling and healing of fracture blisters are clinical indicators of improved soft-tissue condition. Careful soft-tissue handling and low-profile plates are recommended. When the soft-tissue swelling has significantly diminished, anatomic reduction and internal fixation can be done with fewer wound complications than with early ORIF.
Several authors have recommended staged protocols for treatment of complex pilon fractures with severe soft-tissue injuries. Patterson and Cole described immediate fibular fixation and placement of a medial spanning external fixator, followed at an average 24 days later by removal of the fixator and ORIF. Of 22 type C3 pilon fractures, 21 healed within an average of 4.2 months with no infections or soft-tissue complications. These authors cited as advantages of this protocol (1) better soft-tissue management, because the first stage aims to obtain anatomic fibular realignment and restore anatomic length of the distal tibia with little disruption of the soft tissues, and (2) the ability to obtain anatomic realignment of the articular surface under direct vision in the second stage. Disadvantages include the need for a large soft-tissue dissection initially and the difficulty of reduction techniques and maneuvers in a fracture 3 weeks or more after injury. Patterson and Cole also cautioned against creating large soft-tissue dissections and bone stripping.
Blauth et al. compared three different treatment methods in 51 patients with predominantly AO type C pilon fractures. They found no significant difference among the methods in regard to soft-tissue infection. There was no statistical correlation between arthritis and soft-tissue injury or treatment group. There was a trend toward better range of motion, less pain, more frequent return to previous occupation, and increased ability to return to leisure activities in the staged treatment group; however, it was not statistically significant. Based on these results, the authors stated a preference for the staged procedure in patients with severe soft-tissue compromise that involved limited screw fixation of the articular surface through stab incisions and spanning external fixation followed by a less invasive plating technique after soft-tissue healing.
Most pilon injuries are treated in staged fashion owing to the reported decrease in associated complications. However, investigation continues to further our understanding of these difficult fractures in an effort to minimize soft-tissue complications and maximize treatment results. Graves et al. revealed that the larger soft-tissue envelope associated with obesity resulted in a trend toward increased wound complications. White et al. evaluated 95 OTA 43.C-type tibial pilon fractures, 88% of which were managed within 48 hours of injury, and found results comparable to those previously reported for other treatment modalities. The lateral approach has been advocated for treating certain fracture patterns in a staged fashion, as have combined posteromedial and posterolateral approaches. Boraiah et al. reported outcomes of open pilon fractures treated with ORIF in a staged fashion. Despite a 3% and 5% deep and superficial infection rate, respectively, functional outcome scoring for most patients was poor. Harris et al. determined that patients sustaining a type C3 fracture developed more complications, required secondary interventions, and had worse functional scoring at a mean follow-up of 98 months.
Open anatomic reduction and rigid fixation with plate and screw devices can be used effectively to treat tibial pilon fractures if strict attention is paid to fracture reduction and soft-tissue management. This technique is suitable for low-energy fractures with large displaced fragments, little comminution, and no diaphyseal extension ( Fig. 54.15 ). An extremity with minimal swelling and a good soft-tissue envelope is of paramount importance if complications are to be prevented. Skin wrinkling is a good indication that edema has subsided. Soft-tissue handling must be meticulous, and strict “no-touch” techniques have been advocated. The most prudent course is temporization with placement of an external fixator until the soft tissues can be definitively treated. Formal open plating techniques should be used cautiously in open fractures and Rüedi and Allgöwer type III fractures (AO type C3) because of the high reported incidences of poor results and complications.

In an effort to decrease the wound complications associated with traditional open plating techniques, less invasive methods of plating have been developed. The fracture is primarily reduced by ligamentotaxis, and further reduction and plating are performed through limited incisions. Open medial plating has been found to disrupt the blood supply of the distal tibia to a greater extent than percutaneous plating, which might predispose to delayed union or nonunion.
Borens et al. reported their results in 17 patients treated with minimally invasive plating of selected tibial pilon fractures with a low-profile medial plate. All fractures healed. Results were rated as excellent in eight patients (47%), fair in seven patients (41%), and poor in two patients (12%). The authors concluded that this technique was effective and reduced soft-tissue complications associated with open plating of pilon fractures. They advocated the use of this technique in a staged protocol.
Minimally invasive plating techniques have been further enhanced with the widespread development of precontoured locking-plate technology, particularly those with outriggers to target proximal fixation. We do not routinely perform open reduction of the fibular component during the initial setting and prefer to maintain length through application of an external fixator alone, particularly if the fibular fracture is highly comminuted. Alternatively, a small anterolateral surgical approach can be used for articular reduction and then fixation can be done in submuscular fashion and proximal fixation percutaneously positioned. This can be done with a medially based large distractor for facilitation of reduction. The anterolateral approach is described in Chapter 1 . Care must be taken to ensure adequate soft-tissue bridging if a separate incision is necessary to treat the fibula. When the anterolateral approach is used, a separate incision occasionally is needed to place a percutaneous small medial plate if the fracture pattern demands.
Understanding the typical morphology of tibial pilon fractures is paramount to devising an appropriate reduction strategy, whether the fibula is fixed acutely or not. Mapping of tibial pilon fractures has revealed characteristic fracture fragments that can be identified in most fractures. These consist of anterolateral, medial, and posterolateral fragments, with a central component that may be significantly comminuted. As with many ankle fractures, reduction of the fibular component can improve the reduction of the posterior fragment. These fragments must be recognized whether a formal open or a limited technique is used. With open approaches, the reduction sequence (after fixation of the fibula in many cases) begins posteriorly and then progresses medially, followed by central reduction, and finally the anterolateral fragment.
Stage 1
Place the patient supine on a radiolucent operating table and place a tourniquet.
For ORIF, make a standard posterolateral incision.
Reduce the fracture, and fix the fibula with a one third tubular plate.
Close the wound with 3-0 nylon.
Place a triangular external fixator spanning the ankle joint.
Place two pins proximally in the anteromedial aspect of the tibia and place one threaded pin through the calcaneus.
Using ligamentotaxis and the reestablished lateral column, the pilon fracture is temporarily reduced and secured ( Fig. 54.16 ).

Definitive reconstruction can be done as soon as healing of the soft tissues permits, typically as judged by the return of skin wrinkling.
Place the patient supine on a radiolucent table with a tourniquet. If preoperative planning has shown that percutaneous plating is impossible, reduce articular surfaces through a limited anterior arthrotomy, chosen by the location of primary fracture lines, which can also allow bone grafting or application of a small anterior plate or both.
If percutaneous plating is possible, estimate the length of the plate based on preoperative films. Place the plate on the skin while checking the position with fluoroscopy.
Contour the plate to fit on the anteromedial aspect of the distal tibia. After bending and twisting the plate using plate benders, check the anticipated position using fluoroscopy.
Make one anteromedial incision at the proximal end of the anticipated plate position and one at the distal end.
Make a tunnel connecting these two incisions in an extraperiosteal fashion by advancing a clamp from distal to proximal or from proximal to distal.
Tie a strong suture (e.g., Ethibond No. 5) through the first hole in the plate. Use the Kelly clamp to help pull the plate through the subcutaneous tunnel under radiographic control. Through small stab incisions, fix the plate with 3.5-mm cortical low-profile screws. Locking screws may be used if a bridge plate construct is deemed necessary.
If necessary, place a cortical screw through the midportion of the plate. Because the plate is flexible, good bone-plate contact can be achieved ( Fig. 54.17 ).

When final radiographic control shows adequate reduction and fixation, remove the external fixator.
Deflate the tourniquet and obtain hemostasis. Close the wound over drains in standard layered fashion.
Place a bulky cotton dressing with a posterior plaster splint to maintain the ankle in neutral position.
Postoperatively, the limb is immobilized with the use of a splint. Closed suction drains are typically removed on postoperative day 1 or 2. Depending on the rigidity of fixation, splint immobilization is discontinued as wound healing permits. Passive and active range-of-motion exercises are then initiated. Sutures are removed between 2 and 3 weeks postoperatively. Full weight bearing is not permitted until full bony healing is confirmed radiographically, usually by 12 weeks.
If minimally invasive techniques are not deemed appropriate for the fracture pattern, open techniques should be used. Similar to the technique above, once the soft-tissue envelope is appropriate after staged external fixation, the surgeon can embark on definitive fixation. The selected surgical approach should take into account the primary fracture lines or “lines of access” to effect the reduction with the most direct access to minimize soft-tissue undermining. This may consist of multiple smaller surgical incisions. Multiple surgical approaches have been described for definitive fixation, the most common being anterolateral and anteromedial.
Alternatives to the traditional anteromedial approach for ORIF of pilon fractures have been advocated in an attempt to reduce the incidence of soft-tissue complications. The interval is between the peroneal tendons and the flexor hallucis longus. A thicker soft-tissue envelope overlying the plate (flexor hallucis longus muscle) was thought to potentially decrease problems with wound healing and deep infection. A disadvantage of this approach is poor exposure of the ankle joint, which limits its utility in fractures with anterior comminution. Some authors suggest the posterolateral approach should be considered as an alternative surgical approach in fractures that can be effectively reduced posteriorly.
Bhattacharyya examined the complications associated with the use of the posterolateral approach for pilon fractures in 19 patients. Complications occurred in nine of the 19 patients. Six patients (31%) had wound problems (three superficial infections, three deep infections). Four patients (21%) had nonunions (two aseptic, two infected), three patients required ankle arthrodesis, and one patient had a 3-mm step-off. The authors concluded that the posterolateral approach did not reduce the incidence of wound complications compared with other approaches. They recommended this surgical approach only for pilon fractures in which the articular displacement and comminution are predominantly located posteriorly or when an anterior approach is not recommended because of the condition of the soft tissues.
The posterolateral approach is rarely indicated as the sole approach for management of pilon injuries. Instead, it can be a component of an overall strategy to treat these injuries. Some have advocated its use early in the treatment of the fibula and posterior fragment. Definitive ORIF of the plafond from a staged anterior-based approach has the benefit of a stable posterior column to serve as the base for reconstruction.
With the patient under general anesthesia, remove the temporary external fixator that was previously placed. Administer antibiotics preoperatively.
Place the patient prone and exsanguinate the extremity and inflate the tourniquet.
Make a posterolateral incision into the distal tibia between the peroneal tendons and flexor hallucis longus, adjacent to the Achilles tendon. The approach can be carried proximally if needed.
Identify and protect the sural nerve.
Apply a femoral distractor if necessary to gain length or view the joint. Apply the distractor through new pins in the tibia to the calcaneus ( Fig. 54.18 ).

If necessary, plate the fibula through the same incision and fix with a 3.5-mm one third tubular plate.
Obtain articular reduction by direct manipulation of the fracture fragments through the fracture sites under direct exposure. Confirm reduction with fluoroscopy.
Fix the articular fragments with 3.5-mm lag screws or 4.0-mm cancellous screws.
For the metaphyseal component of the injury, apply an appropriate plate for the injury type. C-type injuries typically require a 3.5-mm plate. B-type injuries can be treated with lower-profile implants placed in an antiglide fashion.
For large bone defects caused by comminution, consider using iliac crest bone grafting or appropriate bone graft substitutes.
Perform wound closure in standard layered fashion and consider insertion of a subfascial closed suction drain.
The leg is splinted and elevated for 48 hours. We routinely place a closed suction drain postoperatively for posterolateral approaches. Early ankle motion is encouraged with physical therapy once the wound permits and sutures have been removed. Weight bearing begins at 12 weeks when radiographs permit.
In response to reports of unacceptable results with plating of high-energy tibial pilon fractures with traditional techniques, external fixation combined with limited internal fixation of the fibula and articular surface of the tibia has been advocated as an alternative approach. Reports of external fixation combined with limited internal fixation for tibial pilon fractures have shown a decreased incidence of infection compared with similar fractures treated with plate and screw devices. However, a 20% incidence of pin complications and wound healing problems over the fibular incision were noted in one study.
In a long-term follow-up study (5 to 12 years) by Marsh et al., of 35 pilon fractures treated with monolateral spanning external fixation, reduction was rated as good in 14, fair in 15, and poor in 6. Osteoarthrosis was grade 0 in 3, grade 1 in 6, grade 2 in 20, and grade 3 in 6. Arthrosis was correlated with severity of injury and quality of reduction but did not correlate with clinical result (15 excellent, 10 good, and 7 poor). Fifteen patients rated their outcome as excellent, 10 as good, 7 as fair, and 1 as poor. Most patients (27 of 31) were unable to run.
Another study by Dickson et al. of 37 high-energy tibial pilon fractures (AO B3 and C3) treated by spanning external fixation and a second-stage open reduction of the articular surface at 10 to 21 days reported 81% good and excellent results. Complications included infection in 8%, loss of reduction in 11%, secondary arthrosis in 8%, and one (3%) amputation in a diabetic patient with a failed arthrodesis.
Studies have shown good to excellent results with the use of hybrid external fixation in 67% to 69% of intraarticular or Rüedi-Allgöwer type II fractures and 75% to 97% good results. Complications have been reported in 23% to 66% of patients and include deep and superficial infections and malunion.
Although an integral part of the AO principles for ORIF of tibial pilon fractures, the role of fibular plating is controversial when external fixation is used as the definitive treatment. Potential advantages of fibular plating include increasing mechanical stability, assisting in reduction of the anterolateral articular fragment, and restoring the length and alignment of the tibia. Potential disadvantages include increased operative time, possible wound complications, and potential malreduction resulting in inability to accurately reduce the plafond. In addition, fibular plating restricts the ability of the fixator to be dynamized and may lead to delayed union or varus malunion if metaphyseal defects are not bone grafted. Fibular reduction may be difficult in some fractures, and malreduction impairs the ability to reduce the tibia.
In a study by Williams et al. of patients treated with fibular plating, complications included fibular wound infections (23%), fibular nonunions (9%), and angular malalignment (4.5%). Complications in patients without fibular plating included angular malunions (19%) and tibial wound infection (3%). An increased frequency of delayed union or varus malunion in the fractures with fibular plating was not found; however, the authors concluded that plating of the fibula in tibial pilon fractures treated with external fixation spanning the ankle is associated with significant complications and that good results can be obtained without fibular fixation. Limitations of the study included the small number of patients.
Watson et al. analyzed 39 tibial pilon fractures that were treated with a variety of external fixation devices and were considered treatment failures. They found that 64% of the failures consisted of malunion or nonunion of the diaphyseal-metaphyseal junction in fractures with plated or intact fibulas and unrecognized bone loss or comminution of the tibia that was never bone grafted. The authors contended that this complication may be avoided by early recognition and bone grafting of tibial bone loss or comminution before frame dynamization. Alternatively, bone grafting potentially can be avoided by not plating the fibula and by using a screw or wire to maintain fibular reduction at the ankle mortise. There currently is no definitive evidence to support or condemn fibular fixation in tibial pilon fractures treated with external fixation. The risks and benefits of fibular fixation must be weighed for each individual fracture. We do not routinely stabilize the fibular fracture at the time of initial external fixator application, particularly if the definitive management will be with external fixation. However, we do in select patients treat the fibular fracture early if a posterolateral approach is used to treat a posterior plafond fragment and then return in a staged fashion once the soft-tissue envelope allows for fixation of the remaining components of the injury.
Although external fixation techniques have been shown to reduce the incidence of wound complications and deep infection compared with open reduction and plating, malunions and pin site infections remain problematic. Comparative series have shown that articular reduction was better in the open reduction group than in the external fixation group, although external fixation was used more commonly for more severe fractures.
Traditional half-pin external fixation that spans the ankle joint has the advantages of requiring less soft-tissue dissection and of leaving no large implants in a subcutaneous position, which theoretically should lead to fewer wound complications and infections, especially in open fractures or fractures with severe closed soft-tissue injury. Limited open reduction may be necessary, however, if the fracture does not reduce by ligamentotaxis. External fixation can be used to stabilize almost any fracture of the distal tibia, regardless of comminution, and is especially useful in fractures with diaphyseal extension. Half-pin external fixators are relatively easy to apply, and most surgeons are familiar with this technique. Potential disadvantages include pin track infection and pin loosening, which are common with any type of external fixator; loss of reduction, which can occur if the fixation is removed before the fracture heals; and ankle stiffness, which may occur because half-pin fixators span the ankle and subtalar joints. At least one half-pin usually is inserted into the calcaneus, which makes this technique more difficult if an ipsilateral calcaneal fracture is involved. Half-pins in the hindfoot loosen with time, and bone grafting may be needed in comminuted fractures to promote fracture union before fixator removal.
The articulated half-pin fixator, with a hinge to allow ankle motion, was developed to prevent immobilization of the tibiotalar joint. The axis of the hinge is aligned as closely as possible to the true axis of the ankle, and the articulated hinge can be loosened to allow ankle motion. It has not been proved, however, that the articulating feature improves overall functional results.
Marsh et al. compared 19 patients with pilon fractures treated in a spanning external fixator without ankle motion with 22 patients treated with an articulated spanning external fixator and early ankle range of motion (within 2 weeks of surgery). Patients were placed in a short leg cast or walking boot for 4 to 6 weeks after fixator removal. The authors found no significant differences between the groups in range of motion, pain, or functional scores. The authors cautioned that follow-up was short and that numbers may have been too small to detect differences.
Half-pins are placed in the calcaneus and talus and connected to half-pins in the diaphysis. The fracture is reduced by distraction and ligamentotaxis. The fibula can be plated if the overlying soft tissues have not been damaged. The articular surface is reduced further percutaneously, under fluoroscopic guidance, or through limited incisions made directly over fracture lines. The articular reduction is fixed with 3.5- or 4.0-mm screws ( Fig. 54.19 ). Bone grafting of metaphyseal defects is necessary in 25% to 60% of fractures; it can be done acutely if soft-tissue coverage is good, or it can be delayed 4 to 6 weeks until the soft tissues have healed.

(BONAR AND MARSH)
Fix a hinged, articulated fixator to two screws distally, one in the calcaneus and one in the talus, and to two screws proximally in the tibia. Insert all screws after predrilling. To protect the soft tissues, perform all drilling and screw insertion through sleeves.
Place the calcaneal and talar screws as indicated in Fig. 54.20A to straddle the neurovascular bundle.

Using fluoroscopy, place the talar screw first without using the fixator template. Locate the starting point of the talar screw on the distal medial neck of the talus (see Fig. 54.20A ); place the screw parallel to the dome of the talus, as seen fluoroscopically on an anteroposterior view of the ankle ( Fig. 54.20B ), and roughly perpendicular to the long axis of the foot ( Fig. 54.20C ). The placement and direction of this screw are important because they align the template used to insert the rest of the screws.
Ensure bicortical purchase by making sure that two threads penetrate the lateral neck of the talus on an anteroposterior fluoroscopic view.
Place the calcaneal and tibial screws through the template based on the talar screw. The calcaneal screw can be placed high or low in the tuberosity of the calcaneus by rotating the articulated hinge. The high position allows more postoperative dorsiflexion and is recommended.
Confirm bicortical purchase of the calcaneal screw on an axial fluoroscopic view of the hindfoot. The center of the hinge of the articulated fixator should be near the middle of the talus.
After the screws have been placed, remove the template, apply the fixator, and lock the proximal ball joint. Use a compression distraction apparatus to distract the ankle joint and evaluate the reduction fluoroscopically.
Based on preoperative planning and the intraoperative appearance after distraction, make limited incisions to aid in exact reduction of the articular surface and obtain fixation with small fragment screws. Choose incision locations that coincide directly with the major fracture lines to provide a view of the articular surface, using the fracture as a window. Large tenaculum reduction forceps may help reduce the major fragments.
Use screw fixation for the articular fragments only; do not attempt to obtain screw fixation across the metaphyseal fracture. Tibial plates are not used. Use cannulated screws for percutaneous insertion and keep periosteal stripping to a minimum.
Apply bone graft to the metaphyseal defect through the same incision or through a separate incision if needed.
The limb is kept elevated until soft-tissue healing allows mobilization. Most patients are kept non–weight bearing and are not allowed to bear more than 20 kg of weight during the first 6 weeks. The external fixator is dynamized (the locking nut is released to allow sliding of the telescoping body) at 4 to 12 weeks, at which time weight bearing is increased. The fixator is removed when healing of the fracture is evident on radiographs and the patient can walk without pain when the fixator body is removed. Ankle joint motion is begun when soft-tissue conditions permit, usually at 1 to 2 weeks. An Orthoplast (Johnson & Johnson, New Brunswick, NJ) splint is worn to maintain the ankle in neutral except during range-of-motion exercises.
Hybrid external fixators consist of tensioned wires in the epiphyseal fragment of the tibia connected to half-pins placed in the diaphysis. Similar to half-pin fixators, these devices provide greater preservation of the soft tissues and greater ease in spanning diaphyseal fracture lines than do plating devices. The tensioned wires, which can be used in a manner similar to lag screws, can aid in the reduction and fixation of articular fragments. Confining the fixation to above the ankle joint has potential advantages and disadvantages. The tibiotalar and subtalar joints are not immobilized, which theoretically should diminish stiffness in these areas.
The surgeon must be familiar with the biomechanics of these fixators to ensure a stable construct. In a biomechanical study, Yang et al. found that a bar-ring hybrid fixator consisting of a unilateral fixator body connected to a ring/wire assembly was too flexible. The addition of diagonally placed struts significantly improved the stability of this construct. A two-ring hybrid fixator seemed to have the best mechanical performance. In fractures with extreme articular comminution, the wires may not provide adequate fixation, however. Fixation wires may need to be placed intracapsularly for adequate fixation, and although septic arthritis caused by pin track infection is a potential complication, this has not been a problem in the ankle as it has been in the knee. Neurologic, vascular, or tendinous impalement can occur if safe corridors for wire placement are not recognized. Fractures associated with tibiotalar instability also are not adequately stabilized with this method. Many surgeons do not have experience with tensioned wire techniques. Hybrid fixators are most appropriate for AO type A, type C1, and type C2 fractures.
Early ligamentotaxis reduction is important to close large fracture gaps and to reduce fracture hemorrhage and tension on the tenuous soft-tissue envelope. A delay of more than a few days may make it impossible to disimpact the metaphyseal fragments and makes realignment of any shaft extension and comminution difficult; it also makes indirect reduction difficult and may require a larger or more extensile incision. Calcaneal traction can be applied immediately after evaluation in the emergency department or, for open fractures, in the operating room during emergency irrigation and debridement. Watson et al. described the use of a “traveling traction” device consisting of a 6-mm, centrally threaded Steinmann pin through the calcaneal tuberosity and a similar pin through the proximal tibia at the level of the fibular head. A simple quadrilateral external fixator frame is constructed by applying medial and lateral radiolucent external fixation bars, and manual distraction is done to obtain a ligamentotaxis reduction. A CT scan of the extremity in traction allows formulation of an operative plan. If ligamentotaxis has obtained a relative reduction, percutaneous olive wires can be used, with or without cannulated screws. If the joint is not reduced, a limited open approach is indicated.
Based on review of more than 150 CT scans of these injuries, Watson developed a four-quadrant approach to wire insertion ( Fig. 54.21 ). Incisions are made to correspond with the anatomically “safe” corridors for transfixation wire placement to stabilize the metaphyseal fragments. The only region inaccessible to tension wire fixation is a fracture line that is exactly transverse in the coronal plane. Because of anatomic restraints, olive wires cannot be placed from directly anterior to posterior, and fracture lines in this orientation are best stabilized with small cannulated screws.

(WATSON)
Place the patient on a radiolucent table on a beanbag patient-positioning device. Bolster the beanbag to elevate the entire lower extremity and to allow placement of a circular fixator without its impinging on the table. Maintain calcaneal traction through a table extension with a sterile traction bow. If a two-pin external fixator is in place, use it to maintain traction.
Stabilize the fibula first. If the condition of the soft tissues allows, use a limited open reduction technique to apply a four-hole or six-hole plate. If the soft tissues along the lateral aspect of the fibula are compromised, use percutaneous tenaculum forceps to pull the fibula out to length and pin it temporarily to the lateral tibia with a percutaneous Kirschner wire, which later is replaced with a tensioned olive wire.
The external fixation frame usually consists of three or four rings. Begin the frame with a distally based ring located at the level of the ankle joint. Locate the second ring just proximal to any shaft extension. If there is a wide zone of diaphyseal-metaphyseal extension, an additional middle ring is necessary. Connect the proximal two or three rings above the fracture by long, threaded rods. Leave the distal ring free.
Open the proximal ring construct in a “clamshell” fashion and place it over the tibial shaft. Place a transverse reference wire parallel to the knee joint and level with the fibular head, and attach the proximal ring to this wire. Obtain appropriate soft-tissue clearance and position the proximal ring on the limb to ensure that it is parallel to the knee joint and collinear with the intact proximal shaft of the tibia.
Place a Schanz pin into the proximal tibial shaft and attach it to the most proximal ring. At this point, the proximal ring construct is firmly attached to the tibia above the fracture. Place additional transfixation wires or Schanz pins on the additional proximal rings to obtain two levels of fixation on each ring of the intact proximal shaft. Do not yet place olive wires through any area of comminution.
Articular fixation is performed next. If ligamentotaxis was successful, stabilize the fracture by placing percutaneous olive wires across the major fragments in accordance with the preoperative CT data ( Fig. 54.22A ). This approach differs from techniques in which a standardized pattern of transfixation wire placement is used; in this technique, the transfixation wires are placed where the fracture patterns dictate. For coronal plane fractures, use cannulated screws to facilitate fixation of the wires.

If ligamentotaxis was unsuccessful, an open approach is indicated.
Based on the CT data, select an appropriate corridor and make a 4- to 6-cm incision, avoiding undermining any large cutaneous flaps. If the placement of the incision has been selected carefully, it should lead directly to the major fracture line.
Minimal periosteal stripping is necessary, and the fracture line is opened like a book to reveal the joint. The impacted articular fragments also are visible because the joint is distracted.
Use a small elevator to disimpact the articular surface and reduce it under direct vision.
Use Kirschner wires to hold the fragments temporarily and apply any bone graft necessary to maintain the segment in position and fill any cancellous defects. Reduce the metaphyseal fragments and hold them with temporary Kirschner wire fixation. Use screws for de finitive articular fixation of any coronal fracture lines. Alternatively, for most fracture lines, place olive wires percutaneously or directly through the incision to fix the fragments.
At least three or four olive wires are necessary to obtain adequate fixation of the articular surfaces. If the distal tibial-fibular joint has been disrupted, use an olive wire to reduce the diastasis by passing the wire from the fibula across the tibia. If the fibula has not been plated, ensure that it is pulled out to its full length and that appropriate rotation is maintained before placing the tibia-fibula transfixation wire. Place the final wire, a transverse reference wire, just anterior to the fibula. Pass the wire only through the tibia to ensure that it is parallel to the joint, approximately 1 cm proximal to the ankle joint. Then “clamshell” the distal ring and place it around the wires, positioning the ring on the reference wire ( Fig. 54.22B ). This ensures that the knee and ankle joints are parallel when the distal and proximal rings have been connected.
Attach the remainder of the wires to the free ring. Because the wires may not lie directly in apposition to the ring, build up to the ring by using various posts of different heights ( Fig. 54.22C ).
Tension the opposing olive wires symmetrically using two-wire tensioners. Perform this tensioning under fluoroscopic control to prevent asymmetric compression of the fracture lines.
Attach the distal ring to the proximal rings with threaded rods with conical washers, allowing some variability in reducing and maintaining the overall mechanical axis.
Use the ring at the level of proximal shaft extension to reduce proximal shaft comminution. Use olive or smooth wires to manipulate and maintain shaft alignment and to reduce any large fracture lines in this area. Attach these wires to the mid-distal ring and tension them under fluoroscopy so that the reduction can be observed.
For AO type C injuries with extensive joint involvement and large areas of metaphyseal comminution, it is helpful to preconstruct a four-ring frame with an attached foot frame to maintain distraction at the ankle joint. The distraction construct can be as simple as a calcaneal pin or wire attached to a distal calcaneal ring or as extensive as a full foot frame attached to the distal tibial ring.
Use a distraction frame similar to that described earlier and attach the proximal tibial rings first, providing appropriate soft-tissue clearance.
Attach the foot frame or calcaneal pin and perform distraction ligamentotaxis across the ankle joint by adjusting the threaded rods.
If ligamentotaxis reduction is inadequate, do an open procedure as described previously.
When reduction is satisfactory, position the distal tibial ring at the level of the fracture; pass the fixation wires across the fracture fragments, attach them to the ring, and tension them as described earlier. The only difference in this technique is that the distal tibial ring is already attached to the frame and it is not necessary to “clamshell” the ring to place it around the wires.
In fractures with significant periarticular comminution or fragments with minimal soft-tissue attachment, Watson recommended maintaining distraction across the ankle for 6 weeks. When tentative healing has occurred at the joint line, the foot frame or calcaneal pin is removed in an outpatient procedure. Physical therapy is begun to increase range of motion and general strength. Total non–weight bearing is maintained in patients with severely comminuted (AO type C3) fractures. In fractures with shaft extension, tentative weight bearing is begun when early callus and some signs of healing are seen on radiographs, usually at 8 to 10 weeks. Progressive weight bearing is begun, and by 12 to 14 weeks the patient usually is ambulatory with the aid of one crutch or a cane.
Primary arthrodesis has been suggested as a method of treating severely comminuted tibial pilon fractures. Several investigators have noted, however, that severe skeletal injury and nonanatomic reduction do not preclude a satisfactory clinical result. We recommend stabilization of these fractures with an external fixator to maintain alignment and allow bony consolidation. Arthrodesis can be done later if the patient is sufficiently symptomatic. Primary arthrodesis may be considered for severe open injuries with extensive loss of cartilage from the tibial and talar articular surfaces ( Fig. 54.23 ). The wound is debrided, and the remaining cartilage is removed from the talus and tibia. An external fixator can be used to stabilize the fracture. Bone grafting may be necessary when the soft tissues have healed.

Fractures of the shaft of the tibia cannot be treated by following a simple set of rules. Because of its location, the tibia is exposed to frequent injury; it is the most commonly fractured long bone. Because one third of the tibial surface is subcutaneous throughout most of its length, open fractures are more common in the tibia than in any other major long bone. The blood supply to the tibia is more precarious than that of bones enclosed by heavy muscles. High-energy tibial fractures may be associated with compartment syndrome or neural or vascular injury. The presence of hinge joints at the knee and the ankle allows no adjustment for rotary deformity after fracture, and special care is necessary during reduction to correct such deformity. Delayed union, nonunion, and infection are relatively common complications of tibial shaft fractures.
Evaluation of tibial fractures should include a detailed history and physical examination. The limb is inspected for open wounds and soft-tissue crush or contusion, and a thorough neurovascular examination is performed. A pulse deficit or neurologic deficit may be a sign of compartment syndrome or vascular injury, which must be identified and treated immediately. The ipsilateral femur, knee, ankle, and foot also must be examined. When the examination is completed, the limb is realigned gently and splinted. Appropriate tetanus and antibiotic prophylaxes are administered. Plain anteroposterior and lateral radiographs that include the knee and ankle are obtained. Oblique radiographic views at 45 degrees sometimes are required to detect a nondisplaced spiral fracture. Radiographs of the contralateral tibia sometimes are necessary to evaluate length in fractures with severe comminution or bone loss.
The indications for operative and nonoperative treatment of tibial shaft fractures continue to be refined. Although commonly advocated in the past, nonoperative treatment now is generally reserved for closed, stable, isolated, minimally displaced fractures caused by low-energy trauma and some stable low-velocity gunshot fractures. Operative treatment is indicated for most tibial fractures caused by high-energy trauma. These fractures usually are unstable, comminuted, and associated with varying degrees of soft-tissue trauma. Operative treatment allows early motion, provides soft-tissue access, and avoids complications associated with immobilization. The goals of treatment are to obtain a healed, well-aligned fracture; pain-free weight bearing; and functional range of motion of the knee and ankle joints. The optimal treatment method should assist in meeting these goals while minimizing complications, especially infection. These goals may not be attainable in severely injured limbs.
Sarmiento, Nicoll, and others found that closed treatment with casting or functional bracing is an effective method of treatment for many tibial shaft fractures that avoids the potential complications of surgical intervention. For closed treatment to succeed, the cast or brace must maintain acceptable fracture alignment and the fracture pattern must allow early weight bearing to prevent delayed union or nonunion. Repeated attempts at manipulation should be avoided. If the fracture cannot be well aligned, an alternative method of treatment should be chosen. Axial or rotational malalignment and shortening cause cosmetic deformities and alter the loading characteristics in adjacent joints, which may hasten the development of posttraumatic arthritis.
The amount of malalignment and shortening considered acceptable also is controversial. Distal tibial malalignment may be more poorly tolerated than more proximal malalignment. The recommendations in the literature vary widely: 4 to 10 degrees of varus-valgus malalignment, 5 to 20 degrees of anteroposterior malalignment, 5 to 20 degrees of rotatory malalignment, and 10 to 20 mm of shortening. In general, we strive to achieve less than 5 degrees of varus-valgus angulation, less than 10 degrees of anteroposterior angulation, less than 10 degrees of rotation, and less than 15 mm of shortening. Maintaining fracture alignment is difficult in certain fracture types, and if repeated attempts at realignment have been unsuccessful, operative fixation is indicated.
The important factors in prognosis are (1) the amount of initial displacement, (2) the degree of comminution, (3) whether infection has developed, and (4) the severity of the soft-tissue injury excluding infection. Torsional fractures with or without simple comminution have been found to have a better prognosis than high-energy patterns, such as short oblique or transverse fractures, with or without comminution. Torsional fractures tend to create a longitudinal tear of the periosteum and may not disrupt endosteal vessels, whereas transverse fractures usually tear the periosteum circumferentially and completely disrupt the endosteal circulation. Reduction is difficult in displaced spiral fractures of the distal third of the tibia.
Hoaglund and States classified fractures of the tibia as being caused by either high-energy or low-energy trauma and found this classification useful in prognosis. Fractures in the high-energy group resulted from accidents such as motor vehicle collisions and crush injuries. This group included more than half the total fractures and 90% of the open fractures; fractures in this group healed in an average of 6 months. Fractures in the low-energy group resulted from accidents such as falls on ice and while skiing; these healed in an average of about 4 months. These researchers found that the level of fracture was not significant in the prognosis but that the amount of bony contact was. Fractures in which contact between the fragments after reduction was 50% to 90% of normal healed significantly faster than fractures in which contact was less.
Displacement of more than 50% of the width of the tibia at the fracture site has been noted to be a significant cause of delayed union or nonunion. Fractures with more than 50% comminution are considered unstable and usually are associated with high-energy trauma and significant open or closed soft-tissue injury. The presence or absence of a fibular fracture does not influence the prognosis, although inhibited fracture healing of closed tibial fractures associated with intact fibulas treated with cast immobilization has been reported.
Patient characteristics also can influence the success of closed treatment of tibial shaft fractures. Alignment can be difficult to maintain with casts or braces in patients with edematous or obese extremities. Loss of reduction may occur in noncompliant patients with closed treatment, whereas delayed union and nonunion are common in patients in whom weight bearing must be restricted for a prolonged time. An individual’s functional demands also must be considered when planning treatment.
In comparative studies of intramedullary nailing and casting for the treatment of isolated closed tibial shaft fractures, intramedullary nailing has been found to achieve higher union rates and better functional scores. Although these studies show the superiority of intramedullary nailing over casting for closed unstable tibial shaft fractures, further comparative studies are necessary to confirm these results and establish more rigid treatment guidelines.
Nicoll, an advocate of closed treatment, listed the following indications for internal fixation: (1) open fracture requiring complicated plastic surgery, (2) associated fracture of the femur and other major injuries, (3) paraplegia with sensory loss, (4) segmental fracture with displaced central fragments, and (5) gaps resulting from missing bone fragments. Internal fixation has been recommended for unstable, comminuted, or segmental fractures; bilateral tibial fractures; and ipsilateral femoral fractures. Operative treatment also currently is favored for open fractures, fractures with severe closed soft-tissue injury, fractures associated with compartment syndrome, fractures involving vascular injury, and fractures in patients with multiple trauma.
Fractures in which closed treatment is inappropriate can be treated with plate and screw fixation, intramedullary fixation (interlocking intramedullary nails), and external fixation. Locked intramedullary nailing currently is the preferred treatment for most tibial shaft fractures requiring operative fixation. Plating is used primarily for fractures at or proximal to the metaphyseal-diaphyseal junction. External fixation is useful for fractures with periarticular extension and for severe open fractures. In severely mangled extremities, amputation should be considered.
For open high-energy tibial fractures, results of treatment have improved significantly because of important contributions made by large trauma services. Several factors are important for a good outcome in these fractures. Aggressive and repeated debridements of all devitalized tissue, including large fragments of bone, are essential. Because vascular soft tissue and bone are essential for resisting infection and providing a bed for reconstruction, Gustilo and others stressed the importance of leaving the wound open and repeating debridement every 24 to 48 hours until closure at 5 to 7 days by delayed primary closure, skin grafting, or skin flaps. Our protocol is repeat debridement and irrigation at 48 to 72 hours if there is evidence of continuing demarcation of the zone of injury. All Gustilo type III fractures routinely have repeat debridement. Antibiotics should be used routinely with open fractures. Aminoglycosides are added to cephalosporins for type III open fractures, and penicillin is included for fractures with severe contamination. Soft-tissue coverage by 5 to 7 days should be obtained by delayed closure, skin grafting, or flap coverage.
Although there is no dispute that soft-tissue management is the most important factor in determining the outcome of open tibial fractures, the optimal method of fixation is debated. Sufficient stability of the fracture fragments and soft tissues usually can be obtained only by locked intramedullary nails or external fixation. Plate fixation has been associated with an unacceptably high incidence of infection. For Gustilo type I, type II, and type IIIA open fractures, most orthopaedic traumatologists prefer intramedullary nailing.
Studies comparing unreamed nailing with external fixation have shown that tibial fractures treated with unreamed nailing required fewer additional operations and achieved better functional outcomes with fewer superficial infections than fractures treated with external fixation. Comparisons of reamed with unreamed nailing (two studies with 132 patients) have shown a reduced risk of reoperation with a reamed technique.
Type IIIB open tibial fractures have been associated with a relatively high incidence of infection when treated with external fixation and with unreamed nailing. There are, however, specific open fractures for which acute intramedullary nailing is almost certainly not the best treatment option. Open fractures secondary to war injuries; fractures with severe contamination, especially involving the medullary canal; and type IIIC open tibial fractures, especially those in which limb salvage is questionable, all are potentially better treated with external fixation.
The time to debridement for open tibial fractures has not been found to be predictive of infection; however, fracture severity has. Negative-pressure wound therapy is being used more frequently for open wound management, although similar infection and nonunion rates with negative-pressure wound therapy compared with historical controls have been reported.
We prefer intramedullary nailing for most open tibial fractures. Our protocol ( Fig. 54.24 ) includes planning of postoperative management to decrease the frequency of delayed union and implant failure. With this protocol, union was obtained in 48 (96%) of 50 open tibial fractures. Additional procedures to promote union were done in 18 patients at an average of 4 months after injury.

Mangled extremities are severe open fractures often associated with vascular injury or nerve disruption. Surgeons treating these injuries face the difficult decision of whether to attempt limb salvage or perform early amputation. Salvage often is technically possible but may result in disastrous medical, social, psychologic, and financial consequences for the patient.
Complete anatomic disruption of the tibial nerve in adults and crush injuries with a warm ischemia time of more than 6 hours have been suggested as absolute indications for primary amputation; suggested relative indications include serious associated polytrauma, severe ipsilateral foot trauma, and a projected long course to full recovery. Other factors are the patient’s age, occupation, and medical condition; the mechanism of injury; fracture comminution; bone loss; the extent and location of neurologic and vascular injury; and the severity and duration of shock. Various authors have attempted to formulate scores predicting the likelihood of salvage or amputation, but none has proved entirely accurate. In a long-term study of functional results and quality of life in patients with severe open tibial fractures treated with either salvage or amputation, recovery time and long-term disability were reduced with early below-knee amputation, while another study reported a high rate of preservation of a functional weight-bearing limb in patients with type IIIB open tibial fractures treated with aggressive wound management and early soft-tissue coverage.
In an effort to resolve questions about the indications for limb salvage or amputation in a mangled extremity, the Lower Extremity Assessment Project (LEAP) study group was formed. In a multicenter, prospective, longitudinal study, the investigators identified risk factors that predisposed patients to poor outcomes in the salvage and amputee groups. Poor prognostic indicators were attributable to low educational level, income below poverty level, nonwhite racial background, lack of insurance, poor social support network, smoking, and pending legal action. Patients with salvaged limbs without risk factors for poor outcomes had results equivalent to the results of amputees at 2 and 7 years but required more surgical procedures and more rehospitalizations. Patients with tibial nerve injury and insensate feet had substantial impairment at 12 and 24 months; however, outcomes were no different in patients with amputated or salvaged limbs. The LEAP study group also found that muscle injury, absence of sensation, arterial injury, and vein injury were factors that had the greatest impact on the surgeon’s decision to amputate or salvage the extremity. However, the group of patients with insensate limbs recovered intact sensation in 67%, questioning insensibility as an absolute indication for amputation.
The use of a short cast or functional brace for treatment of a tibial shaft fracture resulted in a 97% union rate in a study by Sarmiento et al. The incidence of nonunion ranged from 0% to 13%. Sarmiento narrowed his indications for bracing to closed fractures and low-energy open fractures. Other studies all resulted in recommendations for some type of closed treatment.
Although good functional results without deformity have been reported in more than 95% of patients, the immobilization required with closed treatment may adversely affect ankle motion. Ankle stiffness has been reported in 20% to 30% of patients who had closed treatment. Angular deformity of more than 5 degrees occurs in 10% to 55% of fractures treated with a cast or brace, and shortening of at least 12 to 14 mm occurs in 5% to 27% of patients. Sarmiento’s series of carefully selected fractures had the best results, whereas series with more unstable fractures reported poorer results. Loss of reduction requiring operative treatment has been reported in 2.4% to 9.3% of patients in several larger series. Anatomic reduction and rigid immobilization are highly advantageous to the healing of a fracture, but not at the risk of infection and delayed union. The closed, early weight-bearing method of treatment often concedes minor complications in favor of a predictably high union rate and no major complications. It is a method applicable to many types of tibial shaft fractures, but it requires a good deal of patience and time from the physician and a cooperative patient. We prefer casting for minimally displaced, stable, low-energy tibial fractures.
Plate fixation has been recommended for treatment of tibial fractures that are unsuitable for nonoperative management historically. Open reduction and plating provide stable fixation, allow early motion of the knee and ankle, and maintain length and alignment. The greatest disadvantage of plating is that it requires soft-tissue stripping, which can lead to wound complications and infection. Before the 1960s, plating of open and closed tibial fractures often was complicated by delayed union, nonunion, implant failure, soft-tissue sloughing, and infection, especially if performed within the first week after injury.
The AO group subsequently developed compression plating techniques and implants that remain in use today. Good functional results were reported in 98% of closed fractures with a 6% complication rate, and 90% good results in open fractures; these had, however, a 30% complication rate. A significant increase in complications was noted in progressively higher-energy fractures that were treated by ORIF, and complications increased from 9.5% for torsional fractures to 48.3% for comminuted fractures. Likewise, increased infection rates from 2.1% for torsional fractures to 10.3% for comminuted fractures were noted. Also, nonunion was twice as common and infection five times more likely when open fractures were treated with plating.
Other investigators also have reported increased complications when plating open tibial fractures (infections 1.9% in closed fractures and 7.1% in open fractures; implant failure 0.6% in closed fractures and 10.3% in open fractures). Most authors now recommend plating for tibial shaft fractures associated with displaced intraarticular fractures of the knee and ankle. Refinements in plating and indirect reduction should be used when plating extended shaft fractures, and soft-tissue handling should be meticulous.
In an effort to decrease the frequency of delayed union, nonunion, and infection after tibial shaft fractures, “percutaneous” plating was developed to obtain stable fixation while preserving the fracture environment. This technique involves plating of any associated fibular fracture, prebending a 3.5-mm dynamic compression plate to match the tibial anatomy, and placing the plate and screws through small incisions. Current indications for percutaneous plating are (1) a tibial shaft fracture with periarticular metaphyseal comminution that precludes locked intramedullary nailing and (2) a tibial fracture that cannot be treated with intramedullary fixation because of a preexisting implant, such as a tibial base plate from a total knee arthroplasty. Percutaneous plating is technically challenging, and malalignment is more frequent than with other methods of fixation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here