Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Varicose veins are extremely common and part of a spectrum of chronic venous disorders. The management of venous disease is a major cause of healthcare expense in the UK National Health Service (NHS) and worldwide. , The enormous impact of venous disease, including varicose veins on patient quality of life is widely acknowledged. , As venous disease may present in many different ways, a variety of clinical teams may be involved in the management of patients with chronic venous disorders and associated complications, including vascular surgeons, dermatologists, plastic surgeons, primary care teams, tissue viability staff and other specialists. A widespread appreciation of the growing prevalence and importance of chronic venous disease has driven a wave of research and innovation in venous diagnostics and treatment modalities.
Optimal patient management involves a detailed holistic patient assessment, evaluation of patient expectations and minimally invasive, multimodal therapy to address underlying haemodynamic abnormalities and reduce venous hypertension.
The venous system of the legs returns deoxygenated blood from the capillary beds to the right atrium via low-pressure, high-capacity venous channels. Muscle pumps located in the calf and foot promote venous flow towards the heart, which is maintained by unidirectional valves throughout, predominantly the peripheral venous system. Retrograde flow (away from the heart) is termed venous incompetence or reflux and is usually secondary to damage to the venous valves.
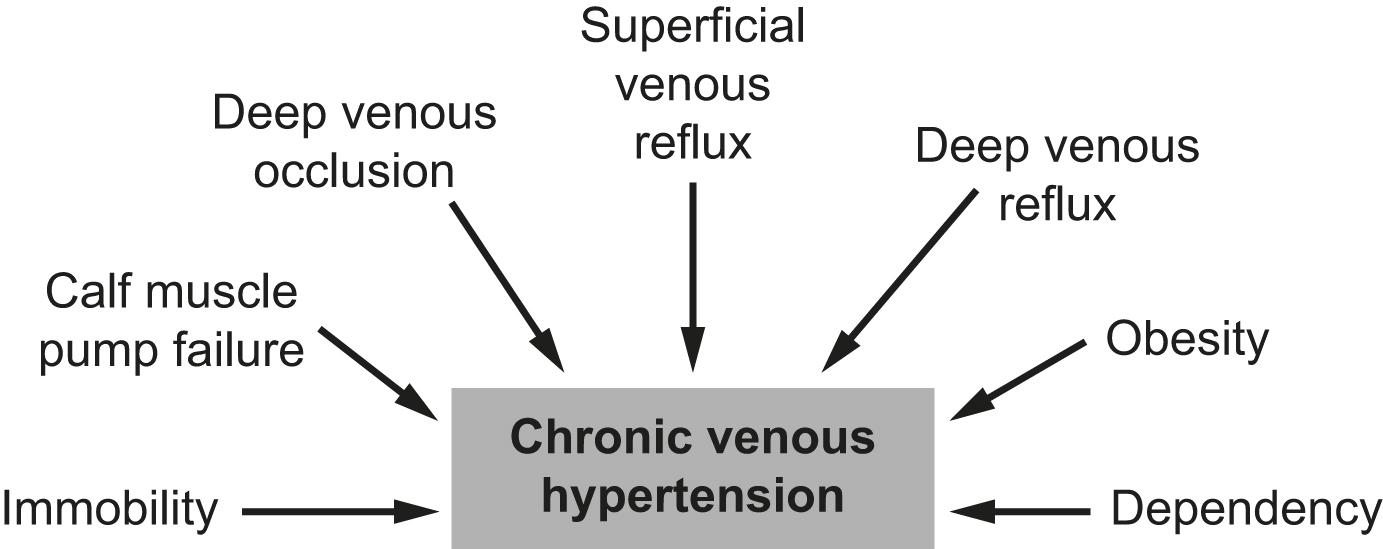
The underlying cause of venous disease is chronic venous hypertension. Persistent high venous pressure causes pathophysiological changes leading to the clinical manifestations of chronic venous disease. A common cause is superficial venous reflux secondary to vein valve incompetence, but other factors contributing to chronic venous hypertension may include deep venous reflux, venous outflow obstruction (post-thrombotic, non-thrombotic or extrinsic compression), calf muscle pump failure (usually because of ankle stiffness or poor calf muscle bulk), leg dependency or patient obesity. The clinical consequences of venous reflux depend not only on the severity of reflux, but also on other factors contributing to venous hypertension ( Fig. 17.1 ) and the effectiveness of measures that reduce venous hypertension (elevation, compression, calf muscle pump activity). The dogma that venous skin changes and ulceration are caused by deep venous disease, whereas superficial venous reflux causes varicose veins has been disproved in recent years; anatomical studies have clearly demonstrated that patients with chronic venous ulceration often have superficial reflux only.
Varicose veins are usually caused by superficial venous reflux affecting the great saphenous vein (GSV) ( Fig. 17.2 ), small saphenous vein (SSV), accessory saphenous or non-truncal veins. Whether the valve failure is a primary phenomenon or secondary to vein wall dilatation is debatable. Two theories have been proposed to explain the development of superficial venous reflux leading to varicose veins. The ‘descending theory’ was popularised by Trendelenburg in the 19th century and suggests that superficial venous incompetence begins at the saphenous junctions and progresses distally, with sequential failure of valves. The ‘ascending theory’ advocates the proximal progression of distal venous incompetence and is supported by the observation that superficial venous incompetence often occurs with a competent saphenous junction. Although both explanations have merits and proponents, the development of varicose veins is likely to be multifactorial. Tortuous, dilated veins seen in patients with deep venous obstruction are often important collateral vessels and should not be confused with varicose veins.

The incidence of venous disease in the population has been evaluated by several large European population studies. These observational studies demonstrated that most adults have reticular or thread veins (CEAP C1), whereas varicose veins or more severe stages of venous disease (CEAP C2–C6, see Box 17.1 ) are present in 25–40% of the population. Venous disease is more common in more industrialised countries, possibly because of higher life expectancies and differences in lifestyle and activity. Interestingly, deep reflux was more common in men, whereas superficial reflux had a higher incidence in women. , Overall, the incidence of venous disease was similar in males and females, which is contrary to most clinical studies, where a female preponderance of 3–4:1 is commonly reported. This discrepancy may reflect gender differences in symptoms experienced, or in the threshold to seek medical advice. The prevalence of chronic venous ulceration (CEAP C6) is 0.3–1.0% in the adult population and venous skin changes (CEAP C4–C5) were present in 5–10%. Although the progression of venous disease is poorly understood, between 3% and 7% of patients with venous skin changes (CEAP C4) are thought to progress to venous ulceration per annum. In general, the greater the patient age, the higher the prevalence and the more advanced the chronic venous disease.
C0: no visible or palpable signs of venous disease
C1: telangiectasias or reticular veins
C2: varicose veins
C3: oedema
C4a: pigmentation or eczema
C4b: lipodermatosclerosis or atrophie blanche
C5: healed venous ulcer
C6: active venous ulcer s: symptomatic, including ache, pain, tightness, skin irritation, heaviness and muscle cramps, and other complaints attributable to venous dysfunction
a: asymptomatic
r: recurrent
Ec: congenital
Ep: primary
Es: secondary (post-thrombotic)
En: no venous cause identified
As: superficial veins
Ap: perforator veins
Ad: deep veins
An: no venous location identified
Pr: reflux
Po: obstruction
Pr,o: reflux and obstruction
Pn: no venous pathophysiology identifiable
Patients with venous disease may seek medical help for a variety of reasons. In the Edinburgh Vein Study, patients reported an inconsistent and gender-dependent association between lower limb ‘venous’ symptoms (heaviness/tension, feeling of swelling, aching, restless leg, cramps, itching, tingling) and the presence and severity of thread, reticular or varicose veins. Although there may be considerable discordance, venous symptoms correlate with severity of venous reflux on duplex imaging. , The CEAP classification was devised in 1994, revised most recently in 2020. It offers a useful classification tool to describe a patient using Clinical, aEtiological, Anatomical and Pathophysiological criteria (see Box 17.1 ). The clinical component of the CEAP classification is often used in isolation. It should be noted that the CEAP classification is a descriptive tool and is not intended for monitoring progression of disease or response to treatment. Other recognised scoring systems include the venous clinical severity score (VCSS) and venous disability score (VDS). In recent years, there has also been a growing interest in patient reported outcomes and quality-of-life scores, which are likely to be most useful for evaluating success after venous interventions.
These small, superficial veins may be highly visible and can cause cosmetic concern ( Fig. 17.3 ) or symptoms. Thread veins (also known as spider veins , telangiectasia , venous flare ) are <1 mm, whereas veins of 1–3 mm are termed reticular veins . Superficial, tortuous veins >3 mm are considered varicose veins. Although not usually funded by state healthcare systems, these veins can be effectively treated using injection sclerotherapy or laser techniques. In general, significant underlying superficial reflux should be addressed before treating thread veins.

Varicose veins are superficial, dilated and tortuous veins usually caused by superficial venous reflux (see Fig. 17.2 ). They are usually seen below the knee, but are also common in the thigh, with the precise location depending on the anatomical distribution of the underlying venous reflux. Most varicose veins are caused by an incompetent GSV, although SSV reflux is the cause in around 20% of patients. Up to a quarter of patients have had previous varicose vein intervention, with the new veins either truly recurrent veins, residual veins not treated in the previous intervention or de novo varicose veins arising in a new distribution. Some patients may have varicose veins because of an incompetent perforating vein, refluxing pelvic/abdominal or other, unnamed, veins. It should be noted that in thin patients, or those with an athletic physique, superficial veins may be very prominent. However, these veins are usually straight and physiological, rather than abnormal.
Venous oedema occurs secondary to increased hydrostatic pressure from chronic venous hypertension. The lymphatic system is unable to adequately drain the increased volume of interstitial fluid. This usually occurs around the ankle but may involve the foot and leg. Swelling is often worse after prolonged standing and towards the end of the day. Isolated oedema because of venous disease is unusual, in the absence of other signs of venous disease. Non-venous causes of oedema, including lymphoedema and cardiac failure, should be considered and may co-exist with venous disease.
Chronic venous hypertension is associated with a number of skin changes ( Fig. 17.4 ), including:
Venous eczema (also known as ‘ venous stasis dermatitis ’). Itchy, dry and scaly skin is a common early skin change caused by venous hypertension. As with most venous skin changes, eczema often occurs on the medial aspect of the lower leg (the ‘medial gaiter area’). While symptoms may be improved with topical creams, eczema is likely to persist or deteriorate unless the underlying causes of venous hypertension are addressed.
Haemosiderinosis and skin pigmentation. Chronic venous hypertension may lead to extravasation of red blood cells, resulting in pigmentation because of haemosiderin deposition in the subcutaneous tissues. There may be an associated inflammatory response, which can mimic cellulitis (see section on Lipodermatosclerosis later). Once the inflammation has settled, pigmentation is usually permanent, despite subsequent venous treatment.
Lipodermatosclerosis. Chronic venous hypertension and inflammation may result in fibrosis and thickening of the skin and subcutaneous fat in the lower leg, with the classic ‘inverted champagne bottle’ appearance. Acute inflammation caused by venous hypertension may be referred to as ‘ acute lipodermatosclerosis ’. As with haemosiderinosis, chronic skin and subcutaneous changes are generally considered irreversible. The primary aim of venous treatment is usually to reduce symptoms, improve patient quality of life and prevent disease progression.
Corona phlebectatica. Also referred to as ‘ malleolar flare ’ or ‘ ankle flare ’, this refers to a leash of prominent intra-dermal veins, located around the medial malleolus. The skin is often fragile, and patients may progress to venous ulceration.
Atrophie blanche. Literally translated as ‘white atrophy’, this refers to a pale, smooth scarring, often associated with telangiectasia that may occur at the site of previous ulceration. Patients with atrophie blanche have a high risk of developing venous ulceration.

Venous ulceration is the commonest cause of leg ulceration and is considered the worst extreme in the spectrum of chronic venous disorders. Venous ulcers are distressing for patients, expensive to manage and challenging to treat. The estimated prevalence is 0.3–1% of the adult population in Western countries, with an increased prevalence in patients >65 years. , A chronic venous ulcer may be defined as a full-thickness defect of the skin, occurring primarily because of chronic venous hypertension, of >4 weeks’ duration, but where there are clear signs of venous hypertension, treatment should be commenced as soon as a wound is present. The medial aspect of the lower leg (the medial gaiter area) is the most common location and other signs of chronic venous hypertension are frequently present, helping to differentiate chronic venous ulcers from other causes of leg ulceration. Ulcers are usually superficial and although a healthy granulating base is commonly seen, healing times are generally protracted, with the median healing duration of 4–6 months. As venous ulcers often affect elderly and frail patients, other factors contributing to poor wound healing (medication, comorbidity, poor nutrition) are frequently present in addition to chronic venous hypertension.
![]() Varicose veins are part of a spectrum of venous disease caused by chronic venous hypertension.
Varicose veins are part of a spectrum of venous disease caused by chronic venous hypertension.
![]() The CEAP classification is an important descriptive tool for patients with venous disease.
The CEAP classification is an important descriptive tool for patients with venous disease.
In addition to the clinical manifestations described earlier, there are specific complications of varicose veins that are important to recognise.
Superficial varicosities may be a cause of significant bleeding either spontaneously or after minimal trauma. Initial care should consist of first aid measures such as elevation and direct pressure. However, fatalities caused by haemorrhage from varicose veins have been reported, often in elderly and vulnerable patients with poor mobility who are unable to bend down to apply direct pressure to the bleeding point. Bleeding varicose veins should be considered an emergency and intervention should be planned urgently. A localised sclerotherapy procedure may be useful as a primary procedure.
Patients may present with pain, redness and hard swelling over varicosities or truncal superficial veins. Traditionally, superficial vein thrombosis (SVT, previously referred to as ‘ phlebitis’ or ‘ thrombophlebitis’ ) has been considered a benign pathology and managed in primary care with analgesia or antibiotics. However, in recent years, it has become clear that the natural history of SVT is much more aggressive than previously appreciated. At the time of diagnosis, around a quarter of patients with SVT have deep vein thrombosis (DVT) or pulmonary embolism (PE, often remote from the site of SVT) and recurrent venous thromboembolism (VTE) events are common. It is clear that the presence of SVT probably signifies a more prothrombotic tendency. Recent guidelines have focussed specifically on the diagnosis and management of SVT and anticoagulation (either prophylactic dose or therapeutic dose, depending on the extent of the SVT) if often indicated. Residual superficial venous reflux should be treated (see treatment section) once the acute inflammation has resolved, after 3 months.
When assessing patients with venous disease, a detailed history of the presenting symptoms should be recorded and potential non-vascular causes should be excluded (particularly orthopaedic, spinal and arterial disorders). It is important to describe the impact of symptoms on patient quality of life as the decision to treat, choice of treatment modality and funding approval may all be guided by these considerations. Cosmetic appearance is a common concern and should always be a consideration when planning intervention, although this is rarely enough for treatment to be approved in state-funded healthcare systems. Other common symptoms include heaviness, aching, burning, itching, swelling, restless legs, cramping or ‘tingling’. The correlation between the size of veins and the severity of symptoms reported by the patient is often poor. This patient group accounts for a significant proportion of medicolegal claims in surgical specialties. Unhappiness after treatment is often caused by recurrent/residual varicose veins or neurological symptoms.
Patients should be asked specifically about the following:
history of DVT;
history of thrombophilia or major risk factors for previous DVT;
use of oestrogen-containing medications (combined oral contraceptive pill, hormone replacement therapy or tamoxifen);
details of previous venous interventions (open or endovenous).
Patients should be evaluated in the standing position to allow filling of varicosities. Most of the required clinical information can be elucidated from inspection alone. Both legs should be examined, in addition to the groins and lower abdomen. The following features should be specifically assessed and documented:
distribution and extent of varicosities (the examiner should specifically document the presence of a saphenovarix and other particularly large or troublesome varicosities);
presence of skin changes of chronic venous disease (oedema, pigmentation, lipodermatosclerosis, ulceration);
arterial status (presence of pulses, ankle–brachial pressure index or toe pressures);
scars and evidence of previous venous interventions;
other factors potentially contributing to venous hypertension (immobility, obesity, ankle stiffness, poor calf muscle bulk);
general patient status and suitability for an intervention (fitness, mobility);
Chronic venous skin changes and ulceration may be present without visible varicose veins, but where chronic venous hypertension is evident, appropriate venous investigations should be performed to detect potentially treatable superficial or deep venous disease.
The accuracy and widespread availability of colour venous duplex scanning has meant that hand-held Doppler assessment of veins should not be used to guide venous interventions and are rarely used in modern practice. Other bedside tests, such as the Trendelenburg test or tourniquet test, are well described in clinical textbooks, but rarely used in routine practice.
The primary goal of venous investigations is to identify treatable superficial and deep venous disease, although in some atypical cases, investigations may help to make the diagnosis of venous disease. A wide range of tests are available, but clinicians should adopt a pragmatic, stepwise approach starting with cheap, non-invasive investigations and avoiding radiation where possible.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here