Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
| American College of Obstetricians and Gynecologists | ACOG |
| Cephalopelvic disproportion | CPD |
| Cesarean delivery | CD |
| Computed tomography | CT |
| Delayed cord clamping | DCC |
| Deep venous thrombosis | DVT |
| Fetal heart rate | FHR |
| Hypoxic-ischemic encephalopathy | HIE |
| National Institutes of Health | NIH |
| Pulmonary embolism | PE |
| Randomized controlled trial | RCT |
| Relative risk | RR |
| Trial of labor after cesarean | TOLAC |
| Vaginal birth after cesarean | VBAC |
| Venous thromboembolism | VTE |
Cesarean delivery (CD) is defined as birth of a fetus from the uterus through an abdominal incision. The terms cesarean delivery or cesarean birth are preferred as opposed to cesarean section . Primary cesarean refers to a CD in a woman without a prior cesarean birth, whereas repeat cesarean refers to a CD in a woman who had a cesarean birth in a previous pregnancy. This chapter reviews the history, incidence, indications, techniques, and complications of CD as well as tubal sterilization.
CD has been described since ancient times, and evidence exists from both early Western and non-Western societies of this surgical procedure being performed. The evolution of the term cesarean has been debated over time. Although originally believed to have been derived from the birth of Julius Caesar, it is unlikely that his mother, Aurelia, would have survived the operation; her knowledge of her son's invasion of Europe many years later indicates that she survived childbirth. In Caesar's time, surgical delivery was reserved for when the mother was dead or dying. Roman law under Numa Pompilius I (“Lex Regia”), then renamed after Caesar (“Lex Cesarea”), specified surgical removal of the fetus before burial of the deceased pregnant woman; religious edicts required separate burial for the infant and mother. The term cesarean may also refer to patients being cut open, because the Latin verb caedare means to cut. Cesarean operation was the preferred term before the 1598 publication of Guillimeau, who introduced the term section .
Although sporadic reports of heroic life-saving efforts through cesarean childbirth existed for hundreds of years, it was not until the latter part of the 19th century that the operation became established as part of obstetric practice. This coincided with the gradual transition of childbirth as primarily a midwife-attended event, often in rural settings, to an urban maternity hospital experience. The wide emergence of maternity hospitals in Europe during the 18th and 19th centuries laid the foundation for establishing obstetrics as a hospital-based specialty.
As new methods for pain relief such as laudanum syrup and chloroform anesthesia emerged, CD for obstructed labor gained popularity over destructive procedures, such as craniotomy, or high forceps delivery, which were often associated with significant fetal injury, deep maternal pelvic lacerations and permanent damage to the maternal bladder and anal sphincter. However, mortality rates for CD remained very high, with sepsis and hemorrhage as leading causes of postoperative deaths. Primitive surgical techniques and lack of antisepsis clearly contributed to morbidity. Surgeons attempted to complete the operation without closing the uterus, fearing that the suture material itself would promote infection and that the uterus would best heal by secondary intention.
Lebas first advocated suturing the uterus after CD in 1769. Traditionally, sutures were not used inside the abdomen or pelvis because they were considered impossible to remove once the cavity was closed. In 1876, Eduardo Porro advocated for supracervical hysterectomy and bilateral salpingo-oopherectomy during CD to control bleeding and to prevent postoperative infection. Shortly thereafter, surgeons gained experience with internal suturing using the silver-wire stitches developed by the gynecologist J. Marion Sims, who had perfected the use of these sutures in the treatment of vesicovaginal fistulae resulting from obstructed labors. In the early 1880s, two German obstetricians, Ferdinand Adolf Kehrer (1837–1914) and Max Sänger (1853–1903), both independently proposed a transverse incision of the lower segment of the uterus, just above the level of the internal cervical os, and developed two-layer uterine closure methods. Another pivotal contribution was made in 1900 by Hermann Johannes Pfannenstiel (1862–1909), a German gynecologist who described a transverse suprapubic incision, or pelvic skin incision.
As gynecologic surgeons performed more CDs and outcomes improved, greater attention was placed on technique, including the site of the uterine incision. Between 1890 and 1925, more and more surgeons began using transverse incisions of the uterus. John Martin Munro Kerr (1868–1960), a professor of midwifery at the University of Glasgow, popularized the Pfannenstiel skin incision and lower segment uterine incision and is considered the “father” of the modern CD. It was noted that such incisions reduced the rate of infection and the risks of incisional hernia and uterine rupture with subsequent pregnancies compared with the vertical incisions. However, before the advent of antibiotics, owing to the risk of peritonitis, extraperitoneal cesarean was advocated by Frank (1907), Veit and Fromme (1907), and Latzko (1909), and was popularized by Beck (1919) in the United States. Interestingly, the vertical opening of the abdomen was still the principal technique used in the 1970s, although it was known from the beginning of the 20th century to be associated with higher rates of long-term postoperative complications, such as wound dehiscence and abdominal incision hernia, and it is also cosmetically inferior.
The introduction of penicillin in the 1940s dramatically reduced the risk of peripartum infections. As antibiotic therapy emerged, the need for extraperitoneal dissection diminished. As technology developed, including improved anesthesia, use of uterotonics, and access to blood transfusion, CD became more commonplace in obstetrics. Given its current safety and effectiveness, a liberalized approach to using cesarean childbirth has emerged in developed countries over the past 40 years.
The CD rate describes the proportion (prevalence) of women undergoing CD of all women giving birth during a specific time period. The CD rate may be further subdivided into primary and repeat CD rates, both as a proportion of the entire obstetric population. CD rates have risen in the United States in a dramatic fashion from less than 5% in the 1960s to 32% by 2017, with stable rates around 31% to 33% in the last 10 years or so. CD accounts for more than 1 million major operations performed annually in the United States. It is the most common major surgical procedure undertaken today in the United States and around the world. Among the reasons for this increase are (1) a continued increase in primary CDs for dystocia, failed induction, reduced operative vaginal delivery, and malpresentation (e.g., breech); (2) an increase in the proportion of women with obesity, diabetes mellitus, and multifetal gestation; (3) increased practice of CD on maternal request; and (4) limited use of a trial of labor after cesarean (TOLAC) delivery due to both safety and medicolegal concerns. Factors responsible for increased cesarean rates are shown in Box 19.1 .
Increased primary CD rate
Failed induction called too early, for example, before at least 18 h of rupture of membranes and oxytocin
Decreased use of operative vaginal delivery
Increased fetal weight
Decline in vaginal breech delivery
Increased repeat CD rate
Decreased use of vaginal birth after CD
Increased proportion of women >35 years
Increased proportion of NP women
Increased primary CDs on maternal request
Malpractice litigation concerns
CD, Cesarean delivery; NP, nulliparous.
A recent increase in international CD rates has also been documented. Rates of about 25% to 30% are reported in some European countries, such as the United Kingdom; they are over 40% in Italy, between 40% and 50% in China (which has seen a recent decrease), and over 50% in countries like Brazil, Mexico, Turkey, and Egypt. The rise in CD rates has prompted increased interest in the indications, complications, and techniques involved with this procedure.
The World Health Organization (WHO) has proposed a population incidence of CD between 10% and 15% as a target to optimize maternal and perinatal health. However, it is not possible to determine an optimal CD rate because any ideal rate must be a function of multiple clinical factors, for example, maternal age, maternal obesity and other comorbidities, and artificial reproductive technology, all of which vary in and within each population, and are influenced by medicolegal issues, practice style, and access to different levels of obstetric care. Further complicating this issue is the absence of complete and accurate data that focus on both maternal and infant outcomes. Hence, although CD rates can be considered a measure of a specific healthcare process (mode of delivery), these rates are not appropriate outcome measures because they do not indicate whether cesarean or vaginal birth results in optimal perinatal outcomes. Maternal and perinatal morbidity and mortality should be the outcomes monitored to ensure best quality of care. Higher CD rates (e.g., 15% to 20% compared with <5% to 10%) have been associated with better perinatal outcomes in several studies. Thus, instead of setting goals or limits for overall CD rates, it is most important to monitor maternal and perinatal health outcomes. The optimal CD rate in the early 21st century depends on the population. For example, Robson has suggested a helpful classification of different populations to compare cesarean rates. Class I is the most common class in most centers and includes singleton term vertex gestations admitted in spontaneous labor. Only by comparing data for similar Robson classes, or at least a similar case mix, can data regarding CD rates be objectively evaluated. Moreover, institutions involved in tertiary obstetric care that manage a large number of preterm deliveries and maternal complications of pregnancy should have higher cesarean rates than primary care facilities. Two populations often targeted for comparison include nulliparous women with a singleton vertex gestation at 37 weeks or greater without other complications and women with one prior low transverse CD delivering a single vertex fetus at 37 weeks or greater without other complications. The use of these simple case-mix adjusted rates makes comparative evaluation of CD rates and their comparison to maternal and perinatal outcomes more meaningful.
In 2014, the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) published an obstetric care consensus document on the safe prevention of primary CD in which several interventions were suggested to prevent unnecessary CDs ( Box 19.2 ). Institutions can indeed safely reduce cesarean birth rates through quality-improvement initiatives.
A prolonged latent phase (>20 h in NP women and >14 h in MP women) should not be an indication for CD. (Grade 1B)
Slow but progressive labor in the first stage should not be an indication for CD. (Grade 1B)
As long as fetal and maternal status are reassuring, cervical dilation of 6 cm should be considered the threshold for the active phase in most laboring women. Thus before 6 cm of dilation is achieved, standards of active-phase progress should not be applied, and CD is not indicated for dystocia. (Grade 1B)
CD for active-phase arrest in the first stage of labor should be reserved for women at or beyond 6 cm of dilation with ruptured membranes who fail to progress despite 4 h of adequate uterine activity or at least 6 h of oxytocin administration with inadequate uterine activity and no cervical change. (Grade 1B)
A specific absolute maximum length of the second stage of labor above which all women should be delivered operatively has not been identified. (Grade 1C)
Before diagnosing arrest of labor in the second stage, if the maternal and fetal conditions permit, allow for the following:
At least 2 h of pushing and 3 h in the second stage in MP women (Grade 1B)
At least 3 h of pushing and 4 h in the second stage in NP women (Grade 1B)
Longer durations may be appropriate on an individualized basis (e.g., with the use of epidural analgesia or with fetal malposition) as long as progress is being documented. (Grade 1B)
Operative vaginal delivery in the second stage of labor should be considered an acceptable alternative to CD. Training in, and ongoing maintenance of, practical skills related to operative vaginal delivery should be encouraged. (Grade 1B)
Manual rotation of the fetal occiput in the setting of fetal malposition in the second stage of labor is a reasonable alternative to operative vaginal delivery or CD. To safely prevent CD in the setting of malposition, it is important to assess fetal position throughout the second stage of labor. (Grade 1B)
Amnioinfusion for repetitive variable fetal heart rate decelerations may safely reduce the CD rate. (Grade 1A)
Scalp stimulation can be used as a means of assessing fetal acid-base status when abnormal or indeterminate ( nonreassuring ) fetal heart patterns (e.g., minimal variability) are present. (Grade 1C)
Induction of labor generally should be performed based on maternal and fetal medical indications and after informed consent is obtained and documented. Inductions at 39 0/7 –39 4/7 weeks of gestation can be offered to reduce the risk of CD and the risk of hypertensive disorders and neonatal respiratory issues. (Grade 1A)
Cervical ripening methods should be used when labor is induced in women with an unfavorable cervix. (Grade 1B)
If the maternal and fetal status allow, CDs for failed induction of labor in the latent phase can be avoided by allowing longer durations of the latent phase (up to 24 h or longer) and requiring that oxytocin be administered for at least 18 h after membrane rupture before deeming the induction a failure. (Grade 1B)
Fetal presentation should be assessed and documented around 36 0/7 weeks of gestation to allow for external cephalic version to be offered. (Grade 1C)
CD to avoid potential birth trauma should be limited to estimated fetal weights of at least 5000 g in women without diabetes and at least 4500 g in women with diabetes. The prevalence of birthweight of 5000 g or more is rare, and patients should be counseled that estimates of fetal weight, particularly late in gestation, are imprecise. (Grade 2C)
Women should be counseled about the IOM maternal weight guidelines in an attempt to avoid excessive weight gain. (Grade 1B)
Perinatal outcomes for twin gestations in which the first twin is in cephalic presentation are not improved by CD. Thus women with either cephalic/cephalic–presenting twins or cephalic/noncephalic-presenting twins should be counseled to attempt vaginal delivery. (Grade 1B)
Individuals, organizations, and governing bodies should work to ensure that research is conducted to provide a better knowledge base to guide decisions regarding CD and to encourage policy changes that safely lower the rate of primary CD. (Grade 1C)
CD, Cesarean delivery; IOM, Institute of Medicine; MP, multiparous; NP, nulliparous.
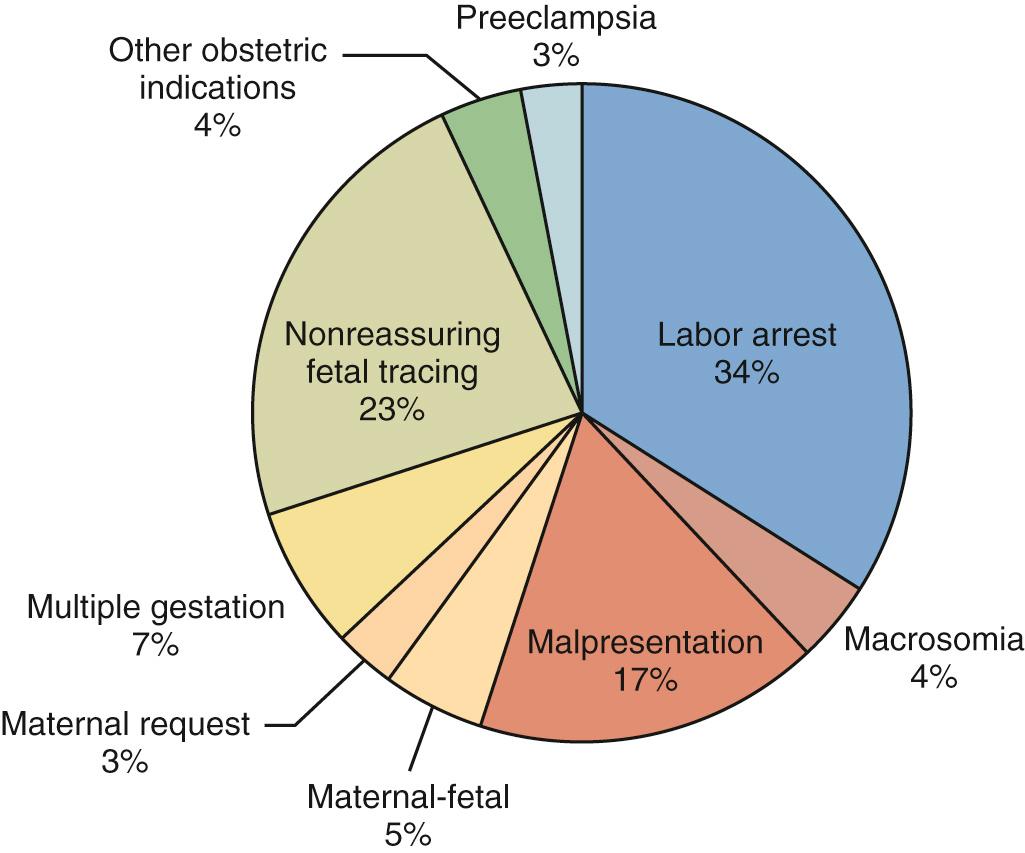
CD can be performed for maternal-fetal, fetal, and maternal indications. The most common current indications are, in order of frequency, (1) failure to progress, also called cephalopelvic disproportion (CPD) or dystocia (about 30%); (2) prior cesarean (30%); (3) nonreassuring fetal heart rate (FHR) patterns (10% to 20%); and (4) fetal malpresentation (5% to 10%). Indications are listed by category in Box 19.3 . Considering just the first CD, the common indications are shown in percentages in Fig. 19.1 .
Failure to progress
Placental abruption
Placenta previa
Repeat cesarean delivery
Cesarean delivery on maternal request
Specific cardiac disease (e.g., Marfan syndrome with dilated aortic root)
Nonreassuring fetal status
Breech or transverse lie
Active maternal genital herpes
Most CDs are performed for conditions that might pose a threat to both mother and fetus if vaginal delivery occurred. Complete placenta previa and placental abruption with the potential for hemorrhage are clear examples. Dystocia presents a risk for both direct fetal and maternal trauma, and it may also compromise fetal oxygenation and metabolic status. The suggestions for definitions of arrest of labor in the first and second stage and failed induction, shown in Box 19.2 , should be followed for management as long as maternal and fetal conditions are reassuring.
Fetal indications are primarily recognized by nonreassuring FHR monitoring with the potential for long-term consequences of metabolic acidosis. Continuous FHR monitoring is associated with a significant reduction in neonatal seizures and remains the most commonly used modality for fetal monitoring in labor. Scalp stimulation can be used to ameliorate the high false-positive rate of continuous FHR monitoring (see Box 19.2 ). Unfortunately, pulse oximetry, ST-segment monitoring, and other modalities have not been consistently shown to affect neonatal outcomes or CD rates (see Chapter 15 ).
Other fetal indications for CD include malpresentation, such as a breech, and more than 90% of these fetuses in singleton gestations are delivered by cesarean. Active maternal genital herpes infection is an indication for CD to reduce the risk for transmission of infection. Suspected macrosomia or the potential for fetal trauma are indications for CD only in rare circumstances (see Box 19.2 ). Fetuses with certain birth defects, such as hydrocephalus with macrocephaly have traditionally undergone CD; however, insufficient data exist to make this an absolute indication. Fetuses with neural tube defects, or abdominal wall defects, such as omphalocele and gastroschisis, can safely be delivered vaginally, if there are no other obstetric indications for cesarean. Fetuses with congenital anomalies with high risk of airway compression, such as neck teratoma or cystic adenomatoid malformation, are now delivered using an ex utero treatment (EXIT) procedure which involves a classical (midline) CD and partial delivery of the fetus (head and upper chest) to allow the pediatric team to establish an airway before the fetus is fully delivered and the umbilical cord is clamped.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here