Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Skin disease can have significance for the anesthesiologist due to the skin manifestations itself, the underlying medical condition, or the potential worsening by anesthetic interventions. Examples of skin diseases in which the anesthetic implications are mainly due to the skin lesion itself include Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), either of which can result in significant fluid losses through the skin and mucous membranes as well as in increased risk of systemic infection. Examples of skin diseases in which the anesthetic implications are mainly due to the underlying medical conditions rather than the skin manifestations themselves include acanthosis nigricans and atopic dermatitis. Examples of skin diseases in which the anesthetic implications are due to both the skin lesion and the underlying medical conditions include scleroderma and dermatomyositis. Finally, examples of skin diseases that can be worsened by anesthetic interventions include epidermolysis bullosa, pemphigus, mastocytosis, and various forms of urticaria.
Acanthosis nigricans refers to thickened, darkened, velvety skin that is usually a manifestation of an underlying medical condition. Based on the underlying medical condition, there are five types of acanthosis nigricans: familial, endocrine (diabetes mellitus), metabolic (obesity), chemical (drug related), and neoplastic. Skin manifestations of acanthosis nigricans are thought to be due to activation of insulin-like growth factor (IGF) receptors in the skin leading to proliferation of keratinocytes and fibroblasts, which produce the skin lesions, especially in skinfolds. The clinical significance of acanthosis nigricans lies mainly in determining its underlying cause and providing appropriate therapy. Some of the most common underlying conditions include insulin resistance and gastrointestinal (GI) cancers ( Figs. 24.1 and 24.2 ). Anesthetic implications of acanthosis nigricans are related to the underlying medical condition and associated therapies.


Atopic dermatitis, also known as atopic eczema, is the cutaneous manifestation of an atopic state (i.e., a type 1 hypersensitive allergic reaction), whose manifestations may include eczema, asthma, food allergies, or hay fever. Skin manifestations of atopic dermatitis vary according to age. Diagnostic criteria must include pruritus, typical morphology and distribution of skin lesions, onset in childhood, and chronicity. Atopic dermatitis is thought to be the result of interaction between genetic predisposition and exposure to allergens, including skin colonization with Staphylococcus aureus . Treatment is symptomatic with topical steroids and systemic antihistamines, plus lifestyle modifications to remove suspected allergens. Anesthetic implications consist of protecting the eczematous skin from trauma or infection, managing the systemic manifestations of the atopic state (asthma, hay fever, otitis media, sinusitis), and therapeutic adjustments based on the medications used in the treatment of atopic dermatitis (corticosteroids, antihistamines, and immunosuppressants).
Epidermolysis bullosa refers to a group of hereditary disorders, whose manifestations are apparent since birth or early childhood and are characterized by easy blistering of both the skin and mucous membranes, including the oropharynx and esophagus. The painful blisters are produced by minor friction or trauma and can lead to serious complications, including esophageal narrowing, skin cancer, digit amputation, or death. Epidermolysis bullosa has three different types that are divided into nonscarring (simplex and junctional) and scarring (dystrophic).
Epidermolysis bullosa simplex has an age of onset from birth to early childhood. It affects mainly the epidermis, has a relatively benign course, allows normal development of the affected person, but still may result in premature death.
Junctional epidermolysis bullosa has an age of onset at birth. Its lesions extend to the dermal-epidermal junction, producing a more severe form of the disease, and results in premature death in early childhood mostly due to sepsis but also due to metastatic squamous cell cancer. Features of junctional epidermolysis bullosa include early blistering since birth, absence of scar formation, and mucosal involvement of the GI, genitourinary, and respiratory tracts.
Dystrophic epidermolysis bullosa may appear at birth through recessive inheritance or during infancy through dominant inheritance. Its manifestations are varied in scope and severity and include dystrophic changes in the skin and mucous membranes, scarring and fusion of the digits, constriction of the oral aperture, esophageal stricture, dysplastic teeth, malnutrition, anemia, electrolyte derangements, hypoalbuminemia, chronic infection, general debilitation, renal dysfunction, and premature death in the second decade of life. Subtypes of dystrophic epidermolysis bullosa include epidermolysis bullosa pruriginosa and albopapuloid epidermolysis bullosa.
Other types of epidermolysis bullosa include epidermolysis bullosa acquisita and acral peeling. Systemic diseases that can be associated with epidermolysis bullosa include porphyria cutanea tarda, amyloidosis, multiple myeloma, diabetes mellitus, and hypercoagulable states. Treatment of epidermolysis bullosa includes symptomatic relief, skin protection, treatment of secondary infection, support of organ function, corticosteroids, intravenous granulocyte colony-stimulating factor (G-CSF), and transplanting skin derived from genetically modified stem cells.
Anesthetic implications of epidermolysis bullosa are related to the primary disease process affecting the skin and mucous membranes, the associated systemic complications, and ongoing therapies.
Throughout the perioperative period, protection of the skin and mucous membranes from even minor trauma is crucial. Blood pressure cuffs should be padded with a loose cotton dressing. Electrocardiogram (ECG) electrodes should have the adhesive portion removed and be held in place using petroleum jelly gauze. A nonadhesive pulse oximetry sensor should be used. Intravenous and intraarterial catheters should be either sutured or held in place with gauze wraps rather than tape. A soft foam, sheepskin, or gel pad should be placed under the patient. Linen creases should be removed. Anesthetic face mask should be gently applied against the face. Lubrication of the face and mask with cortisol ointment or another lubricant can be helpful.
Upper airway instrumentation should be minimized because the squamous epithelium lining the oropharynx and esophagus is very susceptible to trauma, bullae formation, and extensive hemorrhage. Hemorrhage from ruptured oral bullae can be treated by topical application of epinephrine-soaked gauze. In epidermolysis bullosa dystrophica, endotracheal intubation has not been associated with laryngeal or tracheal complications due to greater resistance of laryngotracheal columnar epithelium in comparison with oropharyngeal squamous epithelium. Still, generous lubrication of the laryngoscope blade with cortisol ointment or petroleum jelly and selection of a smaller-than-usual endotracheal tube are recommended. Video laryngoscopy intubation is recommended in cases of small mouth opening due to chronic scarring.
After intubation, the tube must be positioned so that it does not exert pressure at the corners of the mouth and should be immobilized with soft cloth bandages and not taped to the skin. Oropharyngeal suctioning should be avoided as it can lead to life-threatening bulla formation. Aspiration precautions should be implemented in the presence of esophageal stricture.
Epidermolysis bullosa is associated with increased occurrence of porphyria cutanea tarda, which is the type of porphyria that does not precipitate attacks of acute porphyria. Therefore commonly used anesthetic agents, including volatile anesthetics, can be safely used. Skeletal muscle dystrophy of epidermolysis bullosa dystrophica is not associated with excessive hyperkalemic response to succinylcholine. Regional anesthesia (spinal, epidural, brachial plexus block) is an acceptable technique in these patients. Epidermolysis bullosa patients who are on long-term therapy with corticosteroids should receive supplemental corticosteroids therapy to compensate for the needs of the perioperative surgical stress.
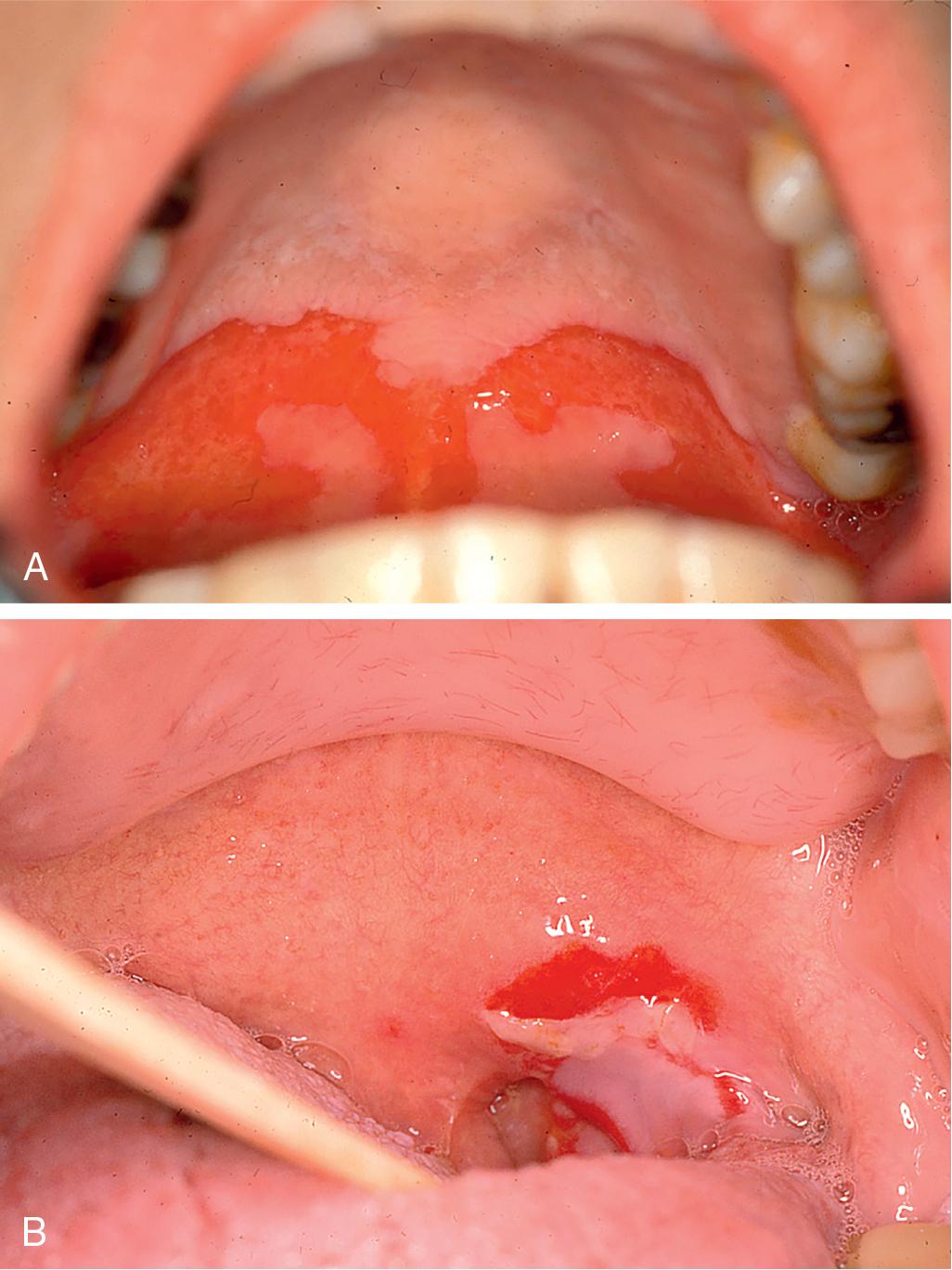
Pemphigus refers to autoimmune vesiculobullous lesions that involve the skin and mucous membranes. Pemphigus is caused by autoantibodies to adherence molecules in the skin called desmogleins, which results in frictional bulla formation in the skin and mucous membranes, leading to fluid and protein loss through the skin and increased risk of infection. The protein loss through the skin is compounded by decreased food intake by mouth due to painful oropharyngeal lesions, which are present in 50% of cases ( Fig. 24.3 ). There are a dozen subtypes of pemphigus, including a drug-induced form. Pemphigus vulgaris is the most common and most significant form of pemphigus because of its high incidence of oropharyngeal lesions. Paraneoplastic pemphigus is a complication of many forms of cancer, including non-Hodgkin lymphoma, chronic lymphocytic leukemia (CLL), thymoma, spindle cell tumors, and Waldenström macroglobulinemia.
Untreated pemphigus can be fatal due to secondary infection and hypoproteinemia. Immunosuppression therapy is the mainstay of treatment, in conjunction with symptomatic and supportive therapy. High-dose corticosteroid therapy is the first line of treatment and has decreased the associated mortality rates from 70% to 5%. Other immunosuppressive therapy includes mycophenolate mofetil, azathioprine, methotrexate, and cyclophosphamide. Resistant disease may respond well to rituximab, intravenous immunoglobulin (IVIG), or plasmapheresis.
Anesthetic considerations are similar to those of epidermolysis bullosa. Preoperative evaluation must include assessment for dehydration, electrolyte derangements, and current immunosuppression therapy. Supplemental stress-dose corticosteroids are often required. Airway management may be difficult and can result in bulla formation, airway obstruction, and bleeding. Regional anesthesia is an acceptable alternative with meticulous sterile and antiseptic conditions, and avoidance of skin infiltration with a local anesthetic solution.
Mastocytosis refers to the accumulation of defective mast cells (mastocytes) and mast cell precursors in body tissues, resulting in cutaneous and systemic manifestations. Cutaneous manifestations of mastocytosis include urticaria pigmentosa, which commonly starts at childhood and improves with aging. Urticaria pigmentosa manifests as pruritic rash with dermatographia on the trunk and extremities.
Systemic mastocytosis spares the central nervous system (CNS) and ranges in severity from indolent to aggressive. It may progress to myelodysplastic disorders, myeloproliferative disorders, or mast cell leukemia, with mast cell proliferation in parenchymal organs, especially bone marrow, which is usually biopsied to categorize the type of systemic mastocytosis. Many of the symptoms of systemic mastocytosis are the result of mast cell degranulation, which can be triggered spontaneously or by nonimmune factors, including temperature changes, exercise, psychological stimuli, alcohol, spicy foods, and histamine-releasing drugs.
Mast cell degranulation results in the release of many cell products, including histamine, leukotrienes, prostaglandins, proteases (tryptases, hydrolases), and proteoglycans (heparin and chondroitin sulfate). Clinical symptoms of mast cell degranulation include pruritus, urticaria, flushing, nausea and vomiting, abdominal cramping, diarrhea, bronchospasm, tachycardia, and hypotension, which may be life threatening.
Medications used for the prevention and treatment of systemic mastocytosis include histamine (H 1 and H 2 ) receptor blockers, mast cell stabilizers, leukotriene receptor–binding inhibitors, proton pump inhibitors (PPIs), adrenergic β 2 agonists, and corticosteroids. In most severe cases, cytoreductive therapy as well as allogenic stem cell transplantation have been used.
Anesthetic implications of mastocytosis include preoperative plan formulation through discussions with the patient, surgeon, and allergist; possible preoperative skin testing to determine the potential of commonly used anesthetic drugs to trigger mast cell degranulation; possible preoperative administration of H1- and H2-receptor antagonists and oral cromolyn sodium; and perioperative avoidance of triggers of mast cell degranulation, including temperature changes, histamine-releasing drugs, emotional distress, and unblocked surgical stress response.
Means for dealing with life-threatening anaphylactoid reactions should be made readily available. Measuring serum tryptase concentration, up to 3 hours after a suspected anaphylactoid reaction, may be useful for detecting mast cell degranulation, but it cannot differentiate between nonimmunologic mast cell degranulation or classic anaphylaxis. Similar precautions should be taken before procedures involving administration of radiocontrast, including pretreatment with H1- and H2-receptor antagonists and corticosteroids.
Urticaria refers to itchy, red, raised skin rash that is also known as hives. Urticaria is commonly categorized into acute, chronic, or physical. Acute urticaria can be encountered in 10% to 20% of the US population at one time or another. Most cases of acute urticaria have undefined cause and resolve within hours, either spontaneously or after administration of antihistamines.
Chronic urticaria is characterized by hives, localized edema, and intense pruritus that last less than 24 hours, whereas urticaria lasting longer than 24 hours raises the possibility of urticarial vasculitis. Chronic urticaria affects approximately twice as many women as men. It follows a remitting and relapsing course, with symptoms typically increasing at night. Its pathophysiology involves stimulation of mast cells and basophils either by nonimmunologic or by immunologic factors, which results in release of histamine and other vasoactive substances such as bradykinin, leading to localized vasodilation, edema, and pruritus. The trigger of chronic urticaria is often unidentified (idiopathic). Treatment aims at dealing with the underlying cause, when identified, and alleviation of symptoms through physical and chemical means, such as tepid showers, antihistamines (H1-receptor antagonists), terfenadine, systemic corticosteroids (≤21-day course), and omalizumab (Xolair), which is an antiimmunoglobulin E (anti-IgE) antibody that binds to IgE and lowers free IgE levels. Acute treatment of oropharyngeal edema includes topical spray with 2% ephedrine and, in severe cases, subcutaneous injection of epinephrine. Chronic urticaria patients should be advised to avoid angiotensin-converting enzyme (ACE) inhibitors, aspirin, and nonsteroidal antiinflammatory drugs (NSAIDs).
Physical urticaria is characterized by hives, itching, and possible angioedema in response to physical stimulation of the skin, such as by cold temperatures. Cold urticaria accounts for 3% to 5% of all physical urticarias and may be either familial or acquired in origin ( Table 24.1 ). It is characterized by development of urticaria and angioedema following exposure to cold air, rain, aquatic activities, snow, consumption of cold foods and beverages, and contact with cold objects. Severe cold urticaria may be life threatening due to laryngeal edema, bronchospasm, and hypotension. The diagnosis is based on skin stimulation at a temperature of 0°C to 4°C for a period of 1 to 5 minutes (cold stimulation test). In cold urticaria, cutaneous mast cells rather than intravascular basophils seem to be the target cells for degranulation, and serum IgE concentrations may be increased. Treatment consists of avoidance of known triggers and administration of systemic antihistamines and topical doxepin.
| Type of Urticaria | Age Range (yr) | Clinical Features | Angioedema | Diagnostic Test |
|---|---|---|---|---|
| Chronic idiopathic urticaria | 20–50 | Pink or pale edematous papules or wheals, wheals often annular; pruritus | Yes | |
| Symptomatic dermatographism | 20–50 | Linear wheals with a surrounding bright red flare at sites of stimulation; pruritus | No | Light stroking of skin causes wheal |
| Physical Urticarias | ||||
| Cold | 10–40 | Pale or red swelling at sites of contact with cold surfaces or fluids; pruritus | Yes | Application of ice pack causes wheal within 5 minutes of removing ice (cold stimulation test) |
| Pressure | 20–50 | Swelling at sites of pressure (soles, palms, waist) lasting ≥2–24 hr; pain, pruritus | No | Application of pressure perpendicular to skin produces persistent red swelling after a latent period of 1–4 hr |
| Solar | 20–50 | Pale or red swelling at site of exposure to ultraviolet or visible light; pruritus | Yes | Radiation by solar simulator for 30–120 seconds causes wheals in 30 min |
| Cholinergic | 10–50 | Monomorphic pale or pink wheals on trunk, neck, and limbs; pruritus | Yes | Exercise or hot shower elicits wheals |
Urticarial vasculitis may be a presenting symptom of immunologic disorders such as systemic lupus erythematosus (SLE) and Sjögren syndrome.
Management of anesthesia in patients with urticaria focuses on avoiding any known triggers, including histamine-releasing drugs, cold intravenous fluids and drugs, cold ambient temperature, as well as the preoperative prophylactic administration of H1- and H2-receptor antagonists and corticosteroids.
Patients with cold urticaria undergoing cardiac surgery have been managed in three ways: off-pump coronary artery bypass grafting (in patients with suitable coronary anatomy), use of cardiopulmonary bypass under normothermic conditions with isothermic cardioplegia, and cardiopulmonary bypass with systemic hypothermia and cold cardioplegia. If the patient is exposed to cold, clinical manifestations of cold urticaria typically become apparent during rewarming rather than during cooling.
Erythema multiforme is a recurrent disease of the skin and mucous membranes characterized by lesions ranging from edematous macules and papules to vesicles (≤0.5 cm) and bullae (>0.5 cm), which may ulcerate. Erythema multiforme attacks can be triggered by infection (especially herpes simplex, hemolytic streptococci), cancer, collagen vascular disease, and drug-induced hypersensitivity.
Stevens-Johnson syndrome and toxic epidermal necrolysis are severe manifestations of erythema multiforme that are associated with multisystem dysfunction, including fever, tachycardia, tachypnea, and skin sloughing ( Figs. 24.4 and 24.5 ). Skin surface area involved in SJS is typically less than 10% of total body surface area, in SJS/TEN overlap syndrome about 10% to 30%, and in TEN more than 30%. Mortality correlates with the surface area of skin involved and is less than 5% for SJS and up to 50% for TEN. Drug triggers of SJS and TEN include antibiotics, analgesics, and certain over-the-counter medications. Corticosteroids are used in the management of severe cases.


Anesthetic risks and precautions in patients with SJS or TEN are similar to those in patients with epidermolysis bullosa or pemphigus, including those related to airway management and tracheal intubation. Patients with moderate to severe SJS and TEN are best treated as a burn patient in a closed burn unit.
Scleroderma (also known as systemic sclerosis) is an autoimmune disorder that involves the skin in addition to other body tissues and organs. It is characterized by three interrelated processes: (1) inflammation and autoimmunity, (2) vascular injury with eventual vascular obliteration, and (3) fibrosis and accumulation of excess matrix in many organs and tissues. The etiology is unclear, but triggers may include exposure to toxins, drugs, and microbial pathogens. Pathophysiology consists of irreversible vascular endothelial cell injury that produces capillary loss, vascular obliteration, leakage of serum proteins into the interstitial space, tissue edema, lymphatic obstruction, and ultimately tissue fibrosis and organ sclerosis. In some patients the disease evolves into CREST syndrome (calcinosis, Raynaud phenomenon, esophageal hypomotility, sclerodactyly, telangiectasia).
The prognosis is poor and is related to the extent of visceral involvement. No drugs or treatments have proved safe and effective in altering the underlying disease process. The typical age at onset is 20 to 40 years, and women are most often affected. Pregnancy accelerates the progression of scleroderma in about half of patients. The incidence of spontaneous abortion, premature labor, and perinatal mortality is high. Manifestations of scleroderma occur in the skin, musculoskeletal system, nervous system, cardiovascular system, lungs, kidneys, and GI tract.
Skin manifestations include thickening, edema, and decreased elasticity to the point of producing flexion contractures, especially in the fingers. Muscular manifestations include myopathy, proximal weakness, and increased plasma creatine kinase concentration. Skeletal manifestations include mild inflammatory arthritis and avascular necrosis of the femoral head. Neuronal manifestations include autonomic, peripheral, and cranial neuropathy, including trigeminal neuralgia. Ocular manifestations include keratoconjunctivitis sicca and corneal abrasions. Cardiovascular manifestations include sclerosis in the small coronary arteries and the conduction system, fibrosis in the cardiac muscle, systemic and pulmonary hypertension, cardiac dysrhythmias, cardiac conduction abnormalities, congestive heart failure, cor pulmonale, pericarditis, pericardial effusion, cardiac tamponade, intermittent vasospasm in the small arteries of the digits, Raynaud phenomenon, and oral or nasal telangiectasias.
Pulmonary manifestations are a major cause of morbidity and mortality and include diffuse interstitial pulmonary fibrosis, with resulting arterial hypoxemia and decreased pulmonary compliance. Renal manifestations include renal artery stenosis, decreased renal blood flow and systemic hypertension, and irreversible renal failure, which used to be the most common cause of death in patients with scleroderma until the introduction of ACE inhibitors, which helped control the hypertension and improve the associated impaired renal function and effectively treat the 10% to 15% of patients who develop a scleroderma renal crisis. It should be noted that corticosteroids can precipitate a renal crisis in patients with scleroderma.
GI manifestations include dryness of the oral mucosa (xerostomia), dysphagia, hypomotility of the lower esophagus, decreased lower esophageal sphincter (which increases the risk of reflux of gastric fluid into the esophagus), and hypomotility of small intestine, which can lead to pseudoobstruction as well as bacterial-induced malabsorption syndrome, including malabsorption of vitamin K, which might lead to coagulation disorders. Broad-spectrum antibiotics are effective in treating bacterial-induced malabsorption syndrome. Somatostatin analogues such as octreotide are effective in improving small intestine hypomotility, whereas prokinetic drugs such as metoclopramide are not.
The only treatment that has been shown to alter the course of scleroderma is the use of ACE inhibitors to treat scleroderma renal crisis. Other aspects of therapy are aimed at monitoring disease activity, alleviating symptoms, and managing complications such as pulmonary hypertension.
Preoperative evaluation of patients with scleroderma is aimed at documenting the myriad systemic manifestations of the disease, any associated functional limitation, and ongoing therapy. Manifestations of scleroderma that could be detected during preoperative evaluation include decreased mandibular mobility, decreased oral aperture, oral or nasal telangiectasias, dermal thickening, Raynaud phenomenon, pulmonary hypertension, systemic hypertension, intravascular volume depletion, renal dysfunction, esophageal hypomotility and hypotonia of the lower esophagus, gastroesophageal reflux disease (GERD), and various forms of neuropathy. Ongoing therapy with H2-receptor antagonists or PPIs should be continued preoperatively or started de novo.
Pulmonary considerations are the main intraoperative anesthetic implications of scleroderma. These include providing prolonged periods of preoxygenation to compensate for the decreased pulmonary oxygen reserve and diffusion capacity, the possible need for higher driving pressures during mechanical ventilation to compensate for decreased pulmonary compliance, avoidance of hypercarbia and hypoxemia that both aggravate pulmonary hypertension, awareness of the increased sensitivity to the respiratory depressant effects of opioids, and preparations for possible need for postoperative ventilatory support in patients with significant pulmonary dysfunction. Drug selection and dosing should take into consideration the degree of renal dysfunction. Hypothermia-induced vasoconstriction should be minimized by active warming of the patient and intravenous fluids. Precautions should be undertaken to prevent corneal abrasions. Regional anesthesia is an attractive choice as it provides peripheral vasodilation and postoperative analgesia, but it might be technically difficult because of the skin and joint changes that accompany scleroderma.
Pseudoxanthoma elasticum is a rare hereditary disorder that causes mineralization of elastic fibers in the skin, eyes, and blood vessels, with the latter leading to premature arteriosclerosis. Cutaneous manifestations are among the earliest clinical features and include the appearance of leathery cobblestone-like skin in skinfolds such as the axilla, neck creases, and groin. Ocular manifestations, which are often the basis of diagnosis, include retinal angioid streaks and vitreous hemorrhage, resulting in loss of visual acuity. Vascular manifestations include hypertension, ischemic heart disease, occlusive peripheral arterial disease of radial and ulnar arteries, which leads to loss of pulses, and degenerative changes of gastrointestinal arteries, which leads to gastrointestinal hemorrhage in about 10% of patients. Cardiac manifestations include endocardial calcification, including the valves, conduction abnormalities, dysrhythmias, and sudden death. Interestingly, some tissues rich in elastic fibers (e.g., lungs, aorta, palms, soles) are not affected by this disease process.
Preoperative assessment and intraoperative management should focus on the increased risk of cardiovascular complications. ECG monitoring is particularly important in view of the potential for cardiac dysrhythmias and conduction abnormalities. There are no specific recommendations regarding the choice of anesthetic drugs or techniques in these patients, provided that adequate control of blood pressure is maintained. Instrumentation of the mouth and GI tract should take into consideration the increased risk of vascular injury of the GI tract.
Ehlers-Danlos syndrome refers to a group of inherited disorders that affect an estimated 1 in 5000 people and result in abnormal production of procollagen and collagen, which affects all body tissues, including the skin, musculoskeletal, vasculature, and smooth muscles. The most common symptoms are skin fragility and hyperelasticity, easy bruising and scarring, musculoskeletal discomfort, joint hypermobility, and susceptibility to osteoarthritis. There are about a dozen forms of Ehlers-Danlos syndrome, of which the vascular form is most markedly associated with increased risk of death due to increased risk of rupture of blood vessels, intestines, or uterus—structures that are rich with type III collagen. Arterial ruptures are notoriously difficult to repair due to marked fragility of the affected arterial wall. Pregnant Ehlers-Danlos syndrome patients are more prone to premature labor, rupture of uterus or large arteries, and excessive bleeding during delivery. Additional complications encountered in various forms of Ehlers-Danlos syndrome include tracheal dilation, spontaneous pneumothorax, mitral regurgitation, cardiac conduction abnormalities, and easy bruisability.
The most important perioperative consideration in patients with Ehlers-Danlos syndrome is the propensity for hemorrhage and tissue rupture. The benefit of any anesthetic intervention is to be weighed against the increased risks of bleeding and tissue rupture. Interventions that are best avoided include instrumentation of the nose or esophagus, intramuscular injections, arterial or central venous cannulation, and regional anesthesia. The least traumatic means of airway instrumentation should be selected. Intermittent inspection of intravenous cannulation sites should be maintained to detect any extravasation of intravenous fluids. During positive pressure ventilation, particular attention should be paid to maintain low peak and plateau airway pressures to minimize the risk of pneumothorax. Surgical complications to be particularly watched for include hemorrhage and wound dehiscence.
Marfan syndrome is an autosomal dominant genetic disorder that is caused by a mutation in the fibrillin-1 (FBN1) gene, which leads to production of defective large glycoprotein fibrillin-1 proteins, which leads to defective connective tissues. It affects about 1 of 20,000 live births. Clinical manifestations include increased length of tubular bones, high-arched palate, pectus excavatum or carinatum, kyphoscoliosis, joint hyperextensibility, emphysema, and increased risk of spontaneous pneumothorax. Ocular manifestations occur in 50% of patients and include myopia, lens dislocation, and retinal detachment. Cardiovascular abnormalities are responsible for nearly all premature deaths in patients with Marfan syndrome. They include dilation, dissection or rupture of the thoracic aorta, mitral valve prolapse or regurgitation, bacterial endocarditis, and conduction abnormalities. For patients with dilated thoracic aorta, prophylactic β blocker therapy is recommended throughout life as it slows the rate of aortic dilation and decreases the risk of aortic dissection. Surgical replacement of the aortic valve and ascending aorta is indicated in Marfan syndrome when the diameter of the ascending aorta exceeds 4.5 cm and substantial aortic regurgitation is present. Pregnancy increases the risk of aortic dissection and rupture.
Preoperative evaluation aims at detecting the variety of manifestations of Marfan syndrome, particularly the cardiovascular abnormalities. Airway management may be complicated by the presence of high-arched palate and propensity for temporomandibular joint dislocation. Video laryngoscopy may facilitate these challenges. The risk of aortic dissection should be minimized by avoiding increases in systemic blood pressure such as during direct laryngoscopy or painful instrumentation. Invasive hemodynamic monitoring, including transesophageal echocardiography (TEE), may be a consideration in selected patients to monitor aortic arch as well as cardiac structure and function. During positive pressure ventilation, the aim is to maintain low airway pressure and keep a high index of suspicion for development of pneumothorax.
Polymyositis and dermatomyositis are idiopathic inflammatory myopathies with multisystem manifestations. Dermatomyositis has characteristic skin changes in addition to muscle weakness that are the results of abnormal immune responses. Dermatomyositis can be considered a paraneoplastic syndrome as it is associated in up to 30% of cases with latent or occult cancer, including that of the breast, colon, or lung. Polymyositis may be associated with other connective tissue diseases, including SLE, scleroderma, rheumatoid arthritis, and mixed connective tissue disorder (MCTD).
Cutaneous manifestations include blue-purple periorbital heliotrope discoloration of the upper eyelids, periorbital edema, scaly erythematous malar rash, and symmetric erythematous raised papules overlying the metacarpal and interphalangeal joints (Gottron papules). The presence or absence of the characteristic skin rash differentiates between dermatomyositis and polymyositis, respectively.
Skeletal muscle manifestations include proximal muscle weakness, especially the flexors of the neck, shoulders, and hips, leading to difficulty in climbing stairs. Pharyngeal muscle weakness leads to dysphagia and increased risk of pulmonary aspiration and pneumonia. Diaphragmatic and intercostal muscle weakness may lead to ventilatory insufficiency. Cardiac manifestations include left ventricular dysfunction, myocarditis, myocardial fibrosis (which may lead to conduction abnormality), and heart block.
Laboratory findings include increase in serum creatine kinase concentrations, which parallel the extent and rapidity of skeletal muscle destruction. Electromyography (EMG) findings consist of a triad of spontaneous fibrillation potentials, decreased amplitude of voluntary contraction potentials, and repetitive potentials on needle insertion. Microscopic findings of muscle biopsy include muscle cell degeneration, regeneration, necrosis phagocytosis, and infiltration by mononuclear white blood cells.
Corticosteroids are the usual treatment for dermatomyositis and polymyositis. When the response to corticosteroids is inadequate, immunosuppressive therapy with methotrexate, azathioprine, cyclophosphamide, mycophenolate, or cyclosporine may be effective. Cyclophosphamide and tacrolimus may be particularly helpful if there is coexisting interstitial lung disease. IVIG may be useful in refractory cases. Biologic agents that have been approved to treat other immune diseases may be considered as experimental treatments if there has been an inadequate response to steroids, traditional immunosuppressive therapy, or immunoglobulins.
Anesthetic implications are related to muscle weakness in the skeletal, cardiac, respiratory, and GI tract muscles. These muscle weaknesses increase the risk of cardiopulmonary complications, including aspiration pneumonia. The pharmacologic responses to depolarizing and nondepolarizing muscle relaxants are normal. However, disease-induced muscle weakness can compound any residual pharmacologic muscle weakness upon emergence from anesthesia leading to difficulty in weaning from mechanical ventilation. In addition, there is an increased risk for aspiration pneumonia upon emergence from anesthesia due to inability to produce effective cough and clear pharyngeal secretions.
Muscular dystrophy refers to a hereditary muscular disorder characterized by degeneration of muscle fibers due to breakdown of the dystrophin-glycoprotein protein complex, which binds myofibrils to the matrix and stabilizes the sarcolemma during contraction and relaxation ( Box 24.1 ). Loss of this protein complex leads to myonecrosis, fibrosis, and increased skeletal muscle membrane permeability. The main clinical manifestation is progressive symmetric skeletal muscle weakness and wasting, with no abnormalities in motor or sensory innervation or deep tendon reflexes. In order of decreasing frequency, muscular dystrophy types include pseudohypertrophic muscular dystrophy (Duchenne muscular dystrophy), limb-girdle, facioscapulohumeral muscular dystrophy (Landouzy-Dejerine dystrophy), and oculopharyngeal muscular dystrophy.
Duchenne muscular dystrophy
Becker muscular dystrophy
Limb-girdle muscular dystrophy
Facioscapulohumeral muscular dystrophy
Emery-Dreifuss muscular dystrophy
Myotonic muscular dystrophy
Duchenne muscular dystrophy is the most common and most severe form of childhood progressive muscular dystrophies. It is caused by a mutation in the dystrophin gene located on the X chromosome and therefore it manifests clinically in boys only. Symptoms typically appear by age 2 to 5 years. Initial symptoms include waddling gait, frequent falls, and difficulty climbing stairs. Affected muscles increase in size due to fatty infiltration but remain weak, therefore this increase in muscle size is labeled pseudohypertrophy. Muscle weakness progresses in severity so that by age 8 to 10 years affected persons are wheelchair bound. Death is common by age 20 to 25 years due to cardiopulmonary complications, including congestive heart failure and pneumonia.
Additional manifestations include kyphoscoliosis, long bone fragility, intellectual disability, myocardial degeneration, mitral regurgitation, sinus tachycardia, ECG changes (tall R waves in V 1 , deep Q waves in the limb leads, a short PR interval), respiratory muscle weakness, recurrent pneumonia, sleep apnea, and pulmonary hypertension. Laboratory findings include increased creatine kinase concentrations by 20- to 100-fold due to increased skeletal muscle membrane permeability and skeletal muscle necrosis. Elevated serum creatine kinase concentrations are encountered in 70% of female carriers. Skeletal muscle biopsies demonstrate necrosis and phagocytosis of muscle fibers.
Use of succinylcholine is contraindicated in Duchenne muscular dystrophy because of the risk of rhabdomyolysis, hyperkalemia, ventricular fibrillation, cardiac arrest, and death. The occurrence of ventricular fibrillation in children receiving succinylcholine and who were later discovered to have Duchenne muscular dystrophy is the basis of including a black box warning against the use of succinylcholine in children below the age of 8 years due to the possibility of the presence of latent Duchenne muscular dystrophy or other forms of muscular dystrophy. Malignant hyperthermia has been observed in Duchenne muscular dystrophy patients even after brief exposure to halothane, although most malignant hyperthermia cases in Duchenne muscular dystrophy have been triggered by succinylcholine or prolonged inhalation of halothane. Therefore a nontriggering technique should be used in patients with Duchenne muscular dystrophy despite the lack of definite genetic association between malignant hyperthermia and Duchenne muscular dystrophy. In addition to using a nontrigger technique, a malignant hyperthermia cart containing dantrolene should be available in anesthetic locations because malignant hyperthermia can be triggered by stressors other than anesthetic agents. Besides the concern about triggering malignant hyperthermia, volatile anesthetics, even in the absence of succinylcholine, have been observed to trigger rhabdomyolysis in patients with Duchenne muscular dystrophy. Other anesthetic considerations in Duchenne muscular dystrophy are related to skeletal muscle weakness, decreased cardiopulmonary reserve, and increased risk of aspiration pneumonia. The pharmacologic response to nondepolarizing muscle relaxants is normal in Duchenne muscular dystrophy. However, disease-induced muscle weakness may obviate the need for their use and may compound any pharmacologic residual muscle weakness during emergence from anesthesia. Pharyngeal and respiratory muscle weakness as well as GI hypomotility decrease the ability to clear airway secretions and increase the risk of pulmonary aspiration of gastric contents during both induction and emergence from general anesthesia. Delayed pulmonary insufficiency may occur up to 36 hours postoperatively even when skeletal muscle strength has apparently returned to its preoperative level. Myocardial depression, cardiac arrhythmias, and conduction abnormalities can be triggered by anesthetic agents or perioperative stress. Regional anesthesia is an attractive choice in Duchenne muscular dystrophy, as it avoids the many risks of general anesthesia, provides postoperative analgesia, and facilitates chest physiotherapy. Monitoring should take into consideration the unique risks of malignant hyperthermia and cardiopulmonary complications.
Becker muscular dystrophy is a milder form of Duchenne muscular dystrophy. Like Duchenne muscular dystrophy, it is an X-linked recessive inherited dystrophinopathy caused by mutation in the dystrophin gene, which encodes the protein dystrophin. The age of onset is later than that of Duchenne muscular dystrophy, with a range of 5 years up to adulthood. The severity of muscle weakness and pseudohypertrophy is less than that of Duchenne muscular dystrophy. The milder severity allows some patients to have a normal life span, but others die prematurely due to cardiopulmonary complications. Anesthetic implications are similar to those of Duchenne muscular dystrophy.
Limb-girdle muscular dystrophy (LGMD) refers to a group of muscular dystrophies rather than a single disease. It has an autosomal pattern of inheritance, so it can affect both males and females. It has a later onset (second to fifth decade), slower progression, and more benign course than Duchenne muscular dystrophy or Becker muscular dystrophy. It affects mostly the shoulder and hip girdle muscles. Anesthetic considerations are similar to those of Becker muscular dystrophy and Duchenne muscular dystrophy.
Facioscapulohumeral muscular dystrophy is the third most common muscular dystrophy after Duchenne muscular dystrophy and myotonic muscular dystrophy, with an incidence of about 1:15,000. It is characterized by a slowly progressive wasting of facial, scapular, and humeral muscles during adolescence but eventually extends into lower limbs also. Symptoms include difficulty raising the arms above the head and difficulty smiling or whistling, with no involvement of cardiac muscle and no increase in serum levels of creatine kinase. Most patients have a normal life span. Anesthetic considerations are similar to other muscular dystrophies.
Oculopharyngeal dystrophy is a rare autosomal inherited muscular dystrophy with late onset of symptoms during the fourth to sixth decade of life. The main symptoms consist of ptosis and dysphagia, with increased risk of aspiration during the perioperative period. There is also increased sensitivity to muscle relaxants. Anesthetic considerations are similar to other muscular dystrophies.
Emery-Dreifuss muscular dystrophy is an X-linked recessive disorder characterized by development of skeletal muscle contractures that precede the onset of skeletal muscle weakness. These contractures are typically in a scapuloperoneal distribution. Respiratory function is usually maintained. Cardiac involvement may be life threatening and present as congestive heart failure, thromboembolism, or a cardiac conduction disorder such as bradycardia. Female carriers of this disorder may experience weakness and cardiac disease. Anesthetic considerations are similar to other muscular dystrophies, with the additional risk of cardiopulmonary complications.
Myotonic dystrophy refers to a group of autosomal dominant hereditary disorders whose clinical muscular manifestations consist of the triad of muscle weakness, muscle wasting, and the occurrence of myotonic contractures after muscle contraction or electrical stimulation. These disorders are the second most common inherited muscle diseases. Clinical manifestations of myotonia include inability to relax the fingers after a firm handshake or grip, inability to relax a muscle after it is tapped with a reflex hammer, and inability to open the eyelids after forcible closure. EMG findings are diagnostic and consist of prolonged discharges of repetitive muscle action potentials.
This inability of skeletal muscle to relax after voluntary contraction or stimulation results from the inability of intracellular adenosine triphosphatase (ATPase) to return calcium to the sarcoplasmic reticulum after contraction. Because the pathophysiology does not involve neural conduction or neuromuscular junction, general anesthesia, regional anesthesia, or neuromuscular blockade is not able to prevent or relieve the skeletal muscle contractions of myotonia, whereas direct infiltration of contracted skeletal muscles with local anesthetic or intravenous administration of quinine (300–600 mg) may induce relaxation.
Cold temperatures and shivering can precipitate myotonia, whereas warm ambient temperature can decrease the incidence of shivering and the severity of myotonia. Most patients with myotonic dystrophy survive to adulthood with little impairment and no apparent symptoms, so they may come for surgery without the underlying myotonia being recognized.
is the most common and most serious form of myotonic dystrophy affecting adults. It is inherited as an autosomal dominant trait, with the onset of symptoms during the second or third decade of life. Unlike other myotonic syndromes, myotonia dystrophica is a multisystem disease, although skeletal muscles are affected the most. Death from pneumonia or heart failure often occurs by the sixth decade of life. This reflects progressive involvement of skeletal, cardiac, and smooth muscles. Cardiac conduction system defects are common and could lead to sudden death. Perioperative morbidity and mortality rates are high and are principally due to cardiopulmonary complications.
Treatment is symptomatic and may include use of mexiletine to improve muscle relaxation. Quinine and procainamide also have antimyotonic properties but can worsen cardiac conduction abnormalities. These three drugs depress sodium influx into skeletal muscle cells and delay the return of membrane excitability.
Muscular manifestations of myotonia dystrophica typically consist of facial weakness (expressionless facies), wasting and weakness of sternocleidomastoid muscles, ptosis, dysarthria, dysphagia, and inability to relax the hand grip (myotonia). Other typical features include the triad of intellectual disability, frontal baldness, and cataracts. Endocrine gland involvement may be indicated by gonadal atrophy, diabetes mellitus, hypothyroidism, and adrenal insufficiency. Delayed gastric emptying and intestinal pseudoobstruction may be present. Central sleep apnea may occur and contribute to hypersomnolence. There is an increased incidence of cholelithiasis, especially in men. Exacerbation of symptoms during pregnancy is common, and uterine atony and retained placenta often complicate vaginal delivery. Cardiac dysrhythmias and conduction abnormalities presumably reflect myocardial involvement by the myotonic process. First-degree atrioventricular heart block is common and is often present before the clinical onset of the disease. Up to 20% of patients have asymptomatic mitral valve prolapse. Reports of sudden death may reflect development of complete heart block. Pharyngeal and thoracic muscle weaknesses make these patients vulnerable to pulmonary aspiration.
Preoperative evaluation and management of anesthesia in patients with myotonia dystrophica must consider the likelihood of cardiomyopathy, respiratory muscle weakness, and the potential for abnormal responses to anesthetic drugs. Succinylcholine should be avoided because it can trigger prolonged myotonia that cannot be reversed with either general anesthesia or nondepolarizing neuromuscular blocking agents. Other pharmacologic triggers of myotonia include methohexital, etomidate, and neostigmine. Physical triggers of myotonia include hypothermia, mechanical stimulation, or electrical stimulation. The pharmacologic response to neuromuscular blocking agents is normal; however, the underlying muscle weakness may obviate the need for their use, which would also obviate the need for the use of neostigmine, which is a myotonia trigger. There is no reported association between myotonic dystrophy and malignant hyperthermia; however, in a group of 44 patients who had in vitro contraction testing (IVCT) for malignant hyperthermia, 4 patients tested positive, 10 patients tested equivocal, and 30 patients tested negative. In addition, volatile anesthetic drugs can aggravate both cardiomyopathy and cardiac conduction problems by direct myocardial depression and by increasing vagal tone. Therefore total intravenous anesthetic (TIVA) technique may be preferable over an inhalation anesthetic technique, while keeping in mind the increased sensitivity of these patients to the respiratory depressant effects of opioids, benzodiazepines, and propofol. This is most likely due to drug-induced central respiratory depression acting in tandem with weak respiratory muscles. In addition, hypersomnolence and central sleep apnea compound increased sensitivity to respiratory depressant drugs. Myotonic contraction during surgical manipulation or use of electrocautery may interfere with surgical access. Drugs such as phenytoin, quinine, and procainamide, which stabilize skeletal muscle membranes, may alleviate this problem. High concentrations of volatile anesthetics can also abolish myotonic contractions but at the expense of myocardial depression. Maintenance of normothermia and avoidance of shivering are very important, since both cold and shivering may induce myotonia. Epidural anesthesia is considered safe in patients with myotonic dystrophy.
Congenital myopathies are primarily muscle disorders that are characterized by structural abnormalities of muscle fibers and accumulation of abnormal proteins in the sarcoplasm ( Box 24.2 ). In contrast to congenital muscular dystrophies, these disorders do not show muscle necrosis or fibrosis on muscle biopsy. Some of these muscle disorders involve abnormal chloride, sodium, and calcium channel genes.
Nemaline rod myopathy
Myotonia congenita
Paramyotonia congenita
Periodic paralysis
Central core disease
Multicore myopathy
Centronuclear myopathy
Nemaline rod myopathy refers to a congenital myopathy in which muscle biopsy shows threadlike ( nema is Latin for thread) rods between normal myofibrils. It is an autosomal dominant myopathy affecting skeletal and smooth muscle of the face, neck, chest, and arms, with clinical manifestations, including muscle weakness, hypoventilation, swallowing dysfunction, and impaired speech. Some forms of nemaline rod myopathy are associated with an abnormal ryanodine receptor 1 (RYR1) gene, which is the main site of genetic mutation resulting in malignant hyperthermia susceptibility. Nemaline rod myopathy is usually a progressive myopathy manifesting as delayed motor development, generalized skeletal muscle weakness, decreased muscle mass and tone, abnormal gait, and loss of deep tendon reflexes. Affected infants may present with hypotonia, dysphagia, respiratory distress, and cyanosis. Additional findings include micrognathia, dental malocclusion, kyphoscoliosis, pectus excavatum, restrictive lung disease, cardiomyopathy, and cardiac failure.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here