Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
In the initial edition of this text, we approached teaching shoulder arthroscopy from the vantage point that a minority of the current surgeons in practice had trained in shoulder arthroscopy. We therefore titled the first chapter “Making the Transition.” However, at present, most young orthopedic surgeons have already learned the basic skills of shoulder arthroscopy during their residency or fellowship. Despite this shift, it is still necessary for any surgeon who is learning how to do arthroscopic shoulder surgery to develop a plan or framework. The two basic types of skills to achieve this are the same as in the previous text: technical and intellectual. Even though orthopedic surgeons may learn the basic skills of shoulder arthroscopy during residency or fellowship, this experience varies widely among training programs.
The fundamental decision is whether to perform shoulder arthroscopy or to use open repair techniques. If surgeons are more comfortable with open procedures and if they are satisfied with their patient outcomes, they may see no reason to adopt shoulder arthroscopy. However, surgeons have various reasons for deciding to acquire or advance their arthroscopic skills (e.g., the belief that arthroscopic techniques produce better results, peer pressure, a desire to learn new concepts and techniques, and patient demand).
Various publications and presentations have documented equal or superior results with arthroscopic techniques compared with open techniques for the performance of subacromial decompression for stage 2 impingement, resection of the acromioclavicular joint for arthritis, repair of the rotator cuff, and the treatment of glenohumeral instability.
Orthopedic surgeons are subject to peer pressure. When they talk among themselves about various shoulder conditions and their treatment, surgeons who perform only open operations may feel that they are behind the times. Orthopedic surgeons are also conditioned to consider new approaches to patient care, and although many surgeons obtain good results with open repair, they are ready and willing to try something new.
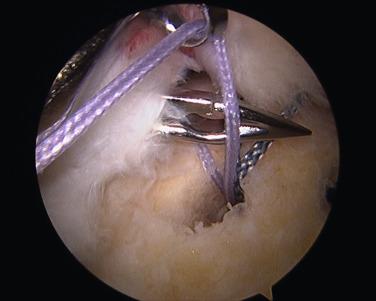
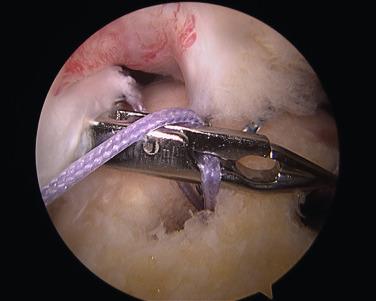
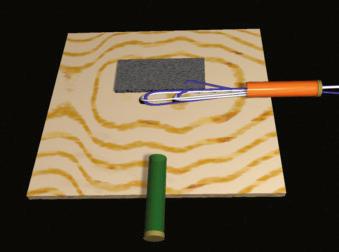
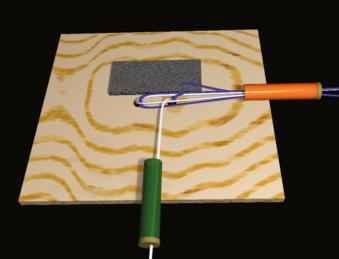
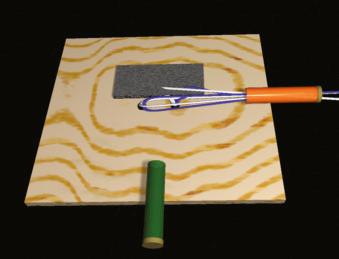
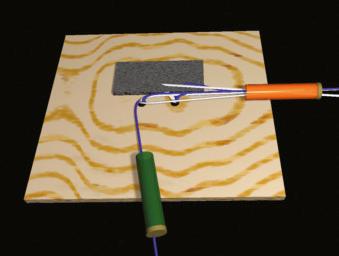
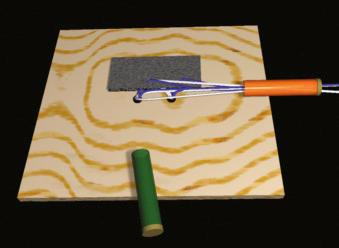
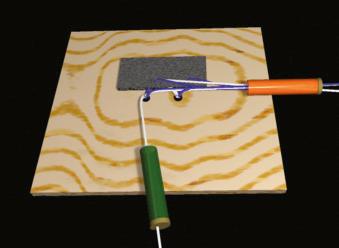
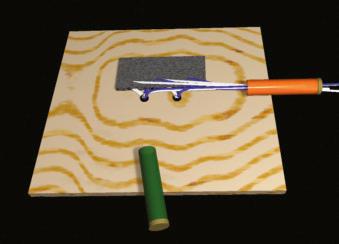
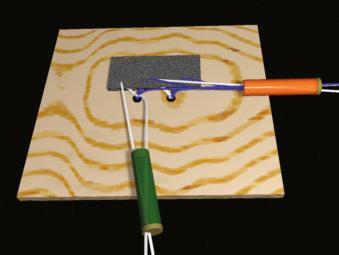
Owing to the dramatic increase in available knowledge, many patients are aware of arthroscopic techniques and inquire whether the surgeon performs a certain procedure arthroscopically or with an open technique. Patients have the perception that arthroscopic procedures result in less pain, smaller scars, and more rapid rehabilitation, although strong arguments can be made to refute all of these assertions. Nonetheless, patients are increasingly insistent on finding surgeons who will perform their operations arthroscopically, viewing the arthroscope as a magical tool capable of miraculous cures. Some surgeons see the arthroscope as a wonderful addition to the surgical toolbox, whereas others, based on their experience, see only its negatives. It is the surgeon's skill that achieves the proper balance ( Figs. 1.1–1.4 ).




Before embarking on a mission to acquire arthroscopic skills, each orthopedic surgeon must evaluate his or her practice patterns and answer some questions: Do you perform a sufficient number of shoulder operations to justify learning a new skill? All orthopedic surgeons should be comfortable with diagnostic glenohumeral joint arthroscopy, but not everyone needs to learn more advanced techniques. If you perform fewer than 20 to 30 shoulder procedures a year and are comfortable with the open technique, we would not advise you to invest the time and effort required to perform these few procedures arthroscopically. Do you have the emotional stability to handle the inevitable frustration when learning to perform procedures arthroscopically? Remember, you will be making a transition from the familiar and comfortable to the new and awkward. Do you have the necessary technical skills? If you cannot perform routine arthroscopic subacromial decompression in 30 minutes or less, you do not have the skills required to perform more complicated reconstructive arthroscopic procedures. Improve your basic skills and speed before taking on a bigger challenge. How do you acquire the necessary skills? Each surgeon must develop a learning plan that focuses on two central issues: technical skills and intellectual skills. In reality, it is hard to separate the two. Learning how to pass a suture through the anterior inferior glenohumeral ligament is of little use if you do not know when this step is necessary.
Most orthopedic surgeons learn the basics of shoulder arthroscopy during residency or fellowship, but for those who did not, other resources are available. The Orthopaedic Learning Center, developed and administered by the American Academy of Orthopaedic Surgeons and the Arthroscopy Association of North America, hosts numerous courses that cover both basic and advanced shoulder arthroscopy. Didactic lectures, panel discussions, and video demonstrations are presented in state-of-the-art lecture halls. The center, located in Rosemont, Illinois, also houses a wet cadaveric laboratory with 48 workstations so that participants can practice with cadaver specimens and arthroscopic instruments.
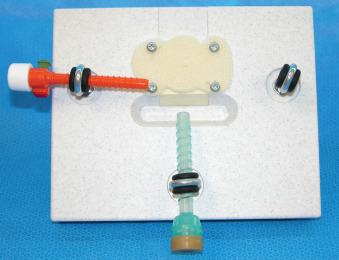
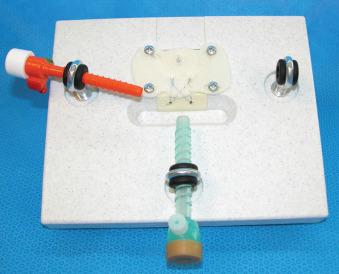
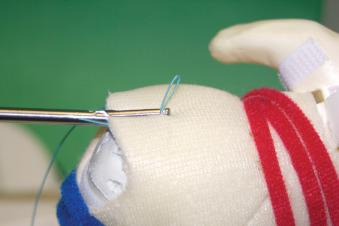
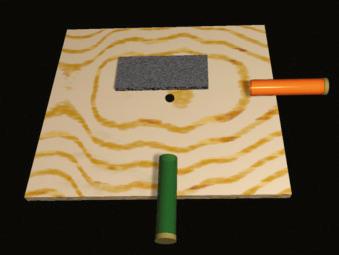
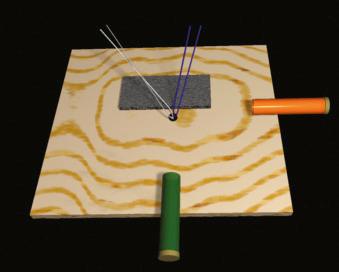
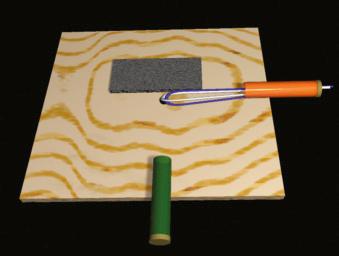
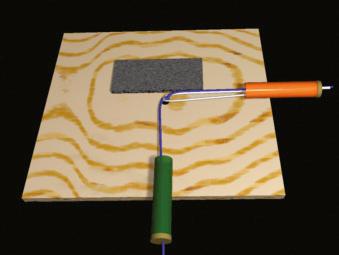
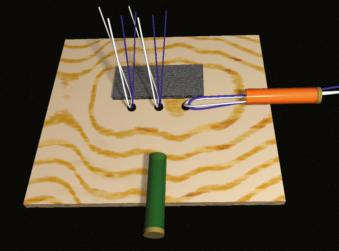
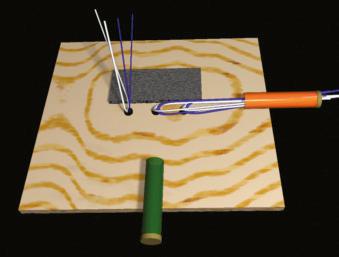
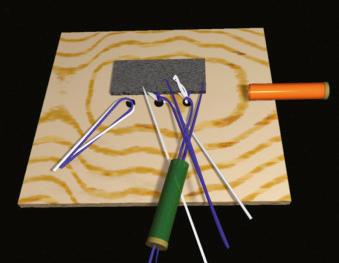
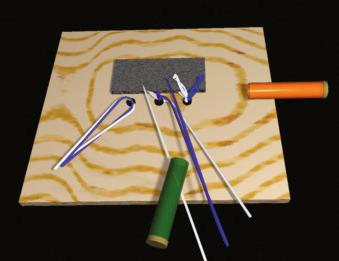
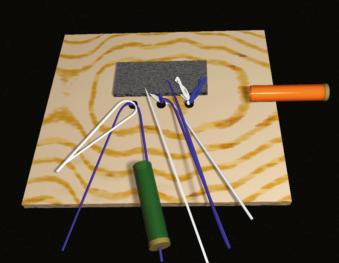
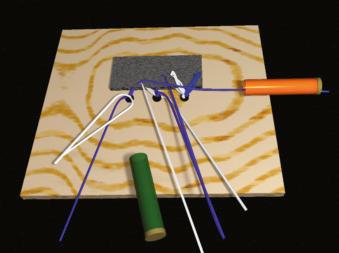
The only true way to master the technical skills of arthroscopy is through practice and repetition. There are several courses that use cadavers to allow the participants to hone their skills. However, many surgeons find this inadequate because a typical course might include lectures and cadaver instruction on arthroscopic subacromial decompression, distal clavicle excision, open and arthroscopic rotator cuff repair, and open and arthroscopic glenohumeral reconstruction. There is insufficient time for participants to become comfortable with all procedures. Other options are to practice on models or simulators ( Figs. 1.5–1.9 ). This is not unreasonable and can improve technical skills to a point. We used to offer a small course limited to 12 registrants that focused solely on one topic—either arthroscopic rotator cuff repair or arthroscopic glenohumeral joint instability. Over a 2-day period, techniques using arthroscopic instruments and video arthroscopy were gradually introduced as participants performed repairs on anatomically detailed plastic shoulder models. This allowed everyone ample opportunity to master the requisite intellectual and technical skills ( Fig. 1.10 ). We have since discontinued this course.




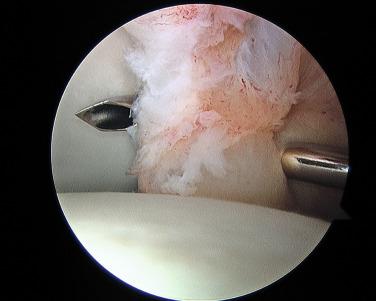
The best way to advance your arthroscopic skills is by focusing on the details of your open repairs. First, take the opportunity to view arthroscopically all rotator cuff tears and unstable glenohumeral joints before performing the open repair or reconstruction. Learn what the typical glenohumeral joint looks like in a 63-year-old patient with a full-thickness rotator cuff tear. From the glenohumeral joint, try to identify the tear. Move the arthroscope into the subacromial space, identify the rotator cuff tear, and estimate its size and shape. Ask the circulating nurse to write down these measurements. Next, open the shoulder and record the size and shape of the tear. With practice, you will find that you can accurately assess the size and shape of tears arthroscopically. Before performing an open Bankart procedure, use the arthroscope to identify the Bankart lesion and estimate its size, then compare that with your impression during the open repair.
As your experience increases, make your observations more precise. When you are viewing a rotator cuff tear from the subacromial space, insert a probe and use it to measure the length and width of the tear. Insert a grasper and try to determine the tear's reparability. Grasp different portions of the tear edge and advance them to different locations near the greater tuberosity. This will help you learn to appreciate tear geometry and repair geometry as viewed through the arthroscope. Make note of the tendon quality. After you perform the open repair and close the skin, reinsert the arthroscope into the subacromial space to see how a completed repair should appear.
As you can appreciate from the preceding description, we believe that the transition from open to arthroscopic repair should proceed slowly as the surgeon makes incremental improvements in his or her technical skills and adds to his or her knowledge base. It is extremely difficult for any surgeon to learn about arthroscopic rotator cuff repair on one day and perform the procedure from beginning to end the next day. It may take up to 1 year to make the transition using the approach described later.
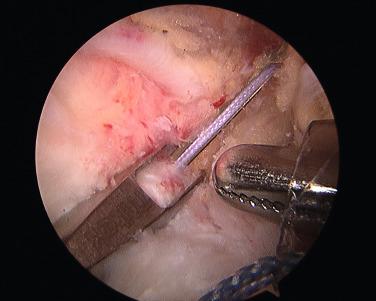
While you hone your basic arthroscopic skills and add to your knowledge, learn the principles of and technical steps required for an arthroscopic repair. For instance, an arthroscopic rotator cuff repair starts with all of the following elements: glenohumeral joint arthroscopy, subacromial bursectomy, coracoacromial ligament management, and possible acromioplasty. You must be expert in these aspects of the procedure. After you are able to evaluate tear size, geometry, and reparability, you must then learn to insert suture anchors, pass sutures through the tendon, manage sutures, and tie secure knots. Fortunately, you can master these techniques before you enter the operating room.
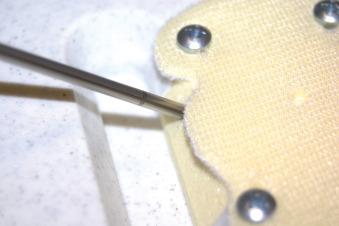
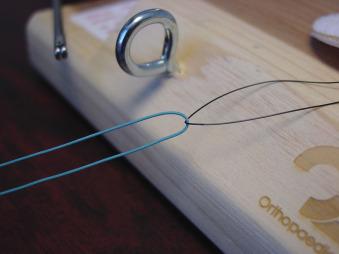
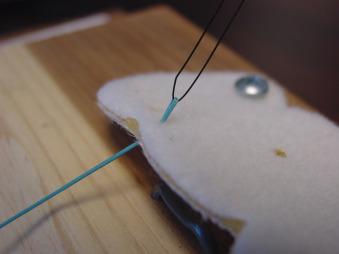
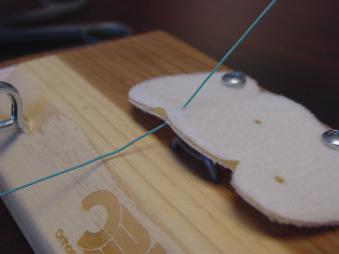
Since the first two editions of this text, suture anchor technology has changed significantly. Anchors in the past were made exclusively of metal. Now we have polyetheretherketone (PEEK), bioabsorbable, suture-based, and biocomposite anchors. These anchors can be preloaded with one, two, or three sutures, or they can have no suture at all. Important characteristics for metal anchors in the past, such as eyelet orientation, are no longer pertinent because many of the nonmetal anchors have the suture loaded into the central core of the anchor. Surgeons should ask their local manufacturer's representative for a spare suture anchor and familiarize themselves with its characteristics. Practice inserting the anchor into a board, and learn how much force is required. Most of these anchors need to have a pilot hole created prior to placement. The traditional metal anchors do not. If you are using the most basic metal anchor, learn how to orient the eyelet so that the sutures slide easily. In addition, most, if not all anchors, have a laser line that indicates the appropriate depth of penetration, and the metal anchors often have a line that orients the eyelet ( Figs. 1.11–1.13 ).


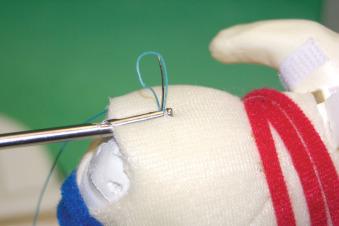
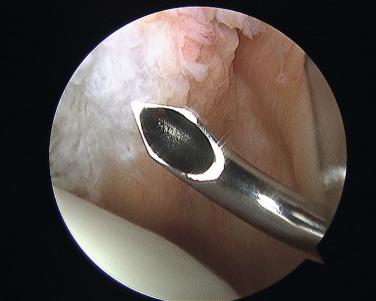
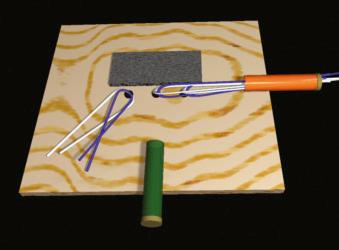
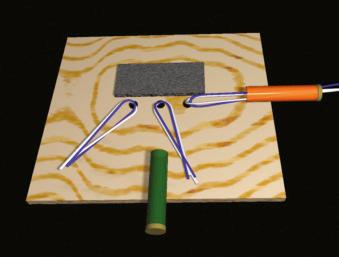
There are two basic methods of passing a braided suture through a tendon or ligament, and you should be familiar with both ( Figs. 1.14–1.31 ). The direct method involves using an instrument to pierce the ligament or tendon and pulling or pushing the suture through it. The indirect method requires that you use some sort of monofilament suture passed through the tendon. This monofilament suture is then used to pull the braided suture through the soft tissue.


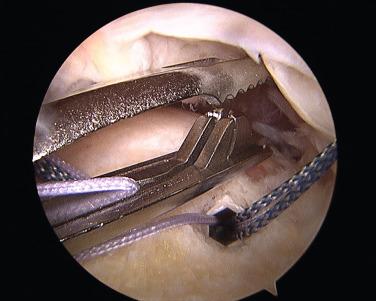

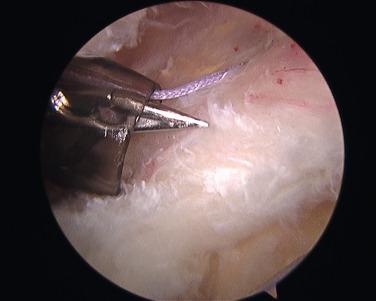


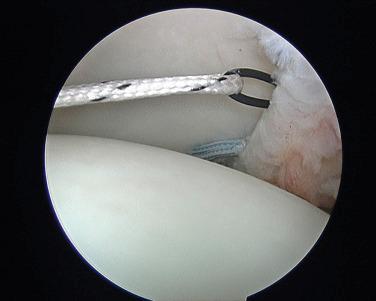
Suture management is critical to arthroscopic shoulder reconstruction. Whether the surgeon is in the subacromial space for a rotator cuff repair or in the glenohumeral joint for a glenohumeral reconstruction, the fundamental problem is too many sutures in too little space. There are two basic solutions: tie the sutures as you insert them, or move the sutures out of the way through cannulas or percutaneous incisions. Experiment with both techniques to determine which one is better for you. Even if you tie the sutures after you insert each one, suture management is important. To avoid nicking the suture (risking suture breakage) when inserting sharp instruments through cannulas, the basic principle is to keep the working cannula free from sutures. Percutaneous anchor insertion is an option in the subacromial space but is not as easy in the glenohumeral joint, owing to the mass of soft tissue the anchor must penetrate.
To practice suture management, write out in detail each step of the operation and decide when you must move sutures. When you write out the operative steps in detail, it gives you an accurate impression of how many suture manipulations are needed. Reviewing these steps with members of your operative team gives them a much better idea of what needs to be accomplished, as well as an appreciation of the operation's complexity.
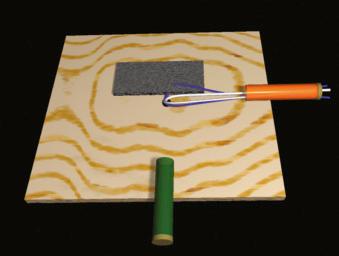
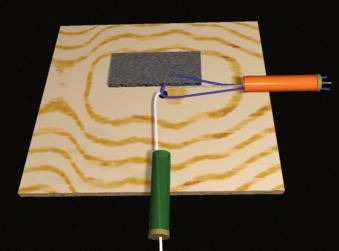
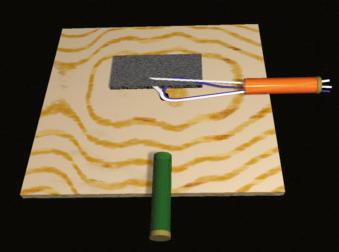
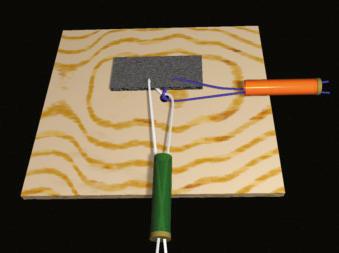
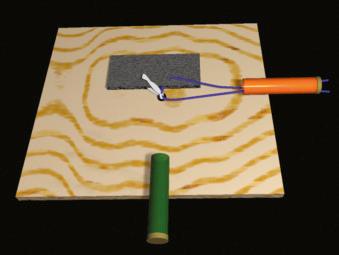
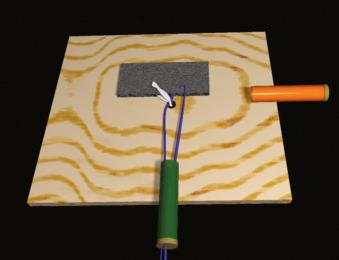
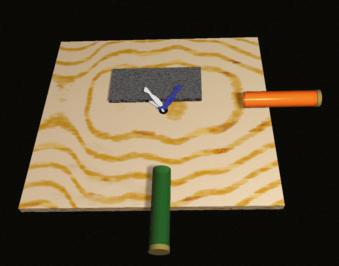
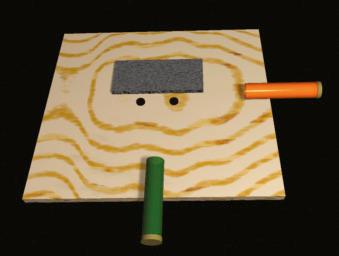
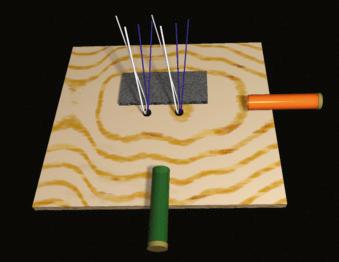
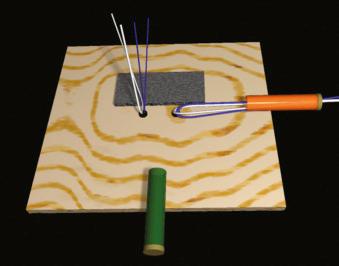
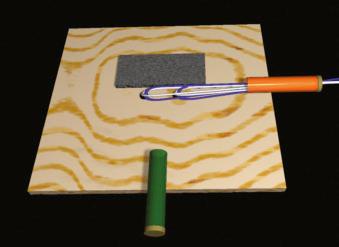
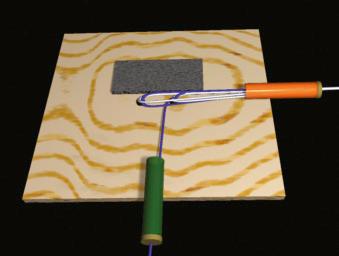
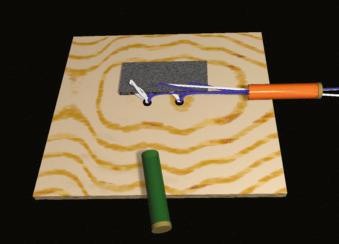
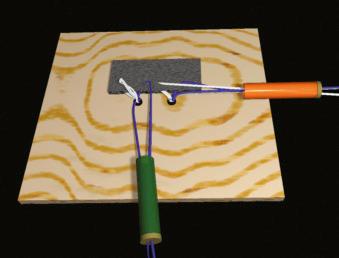
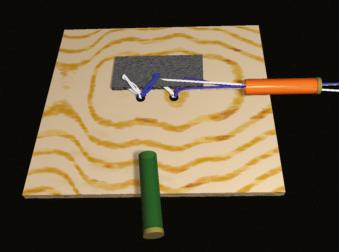
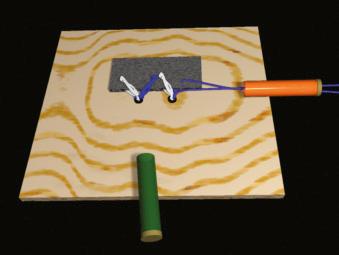
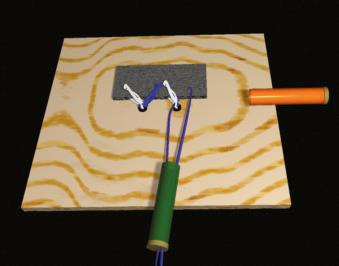
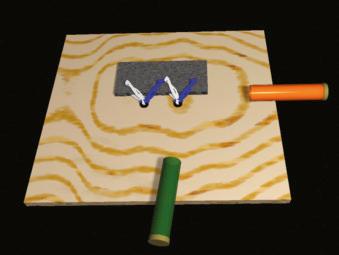
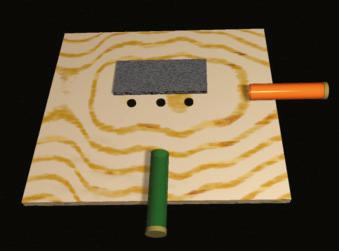
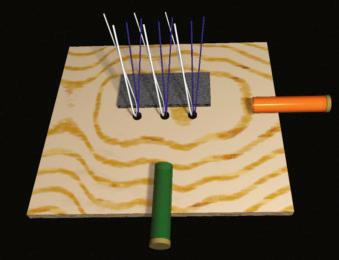
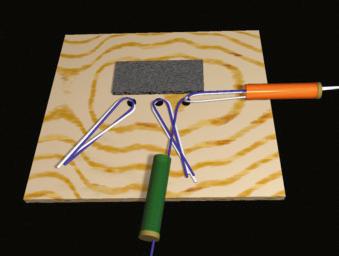
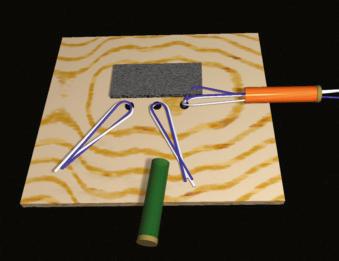
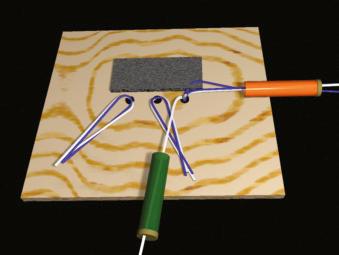
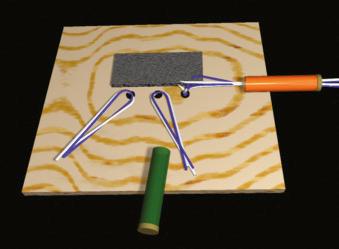
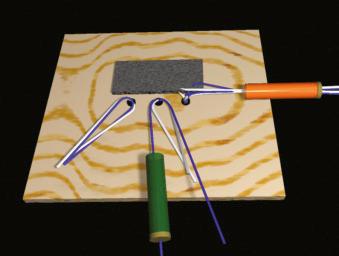
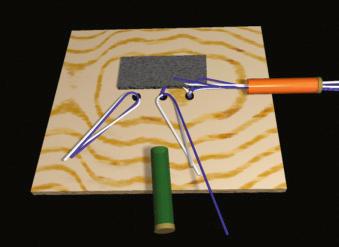
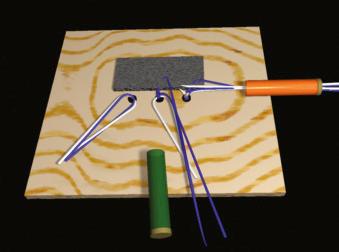
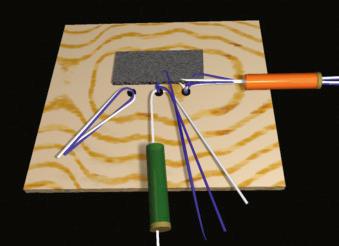
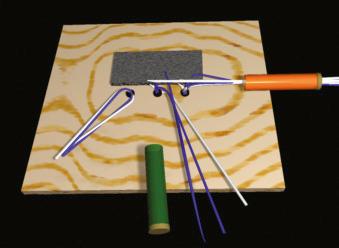
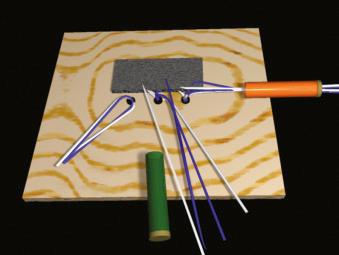
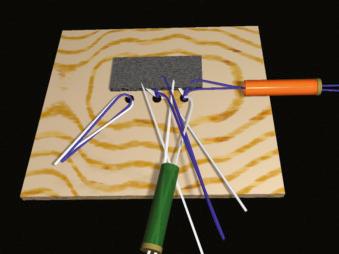
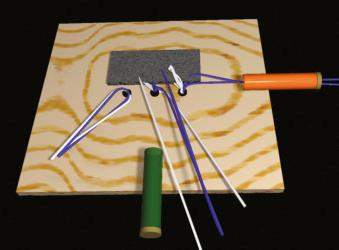
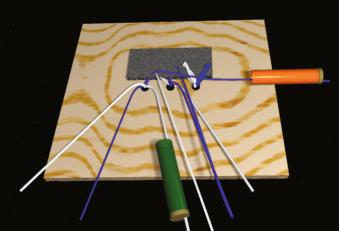
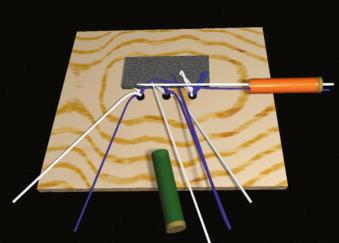
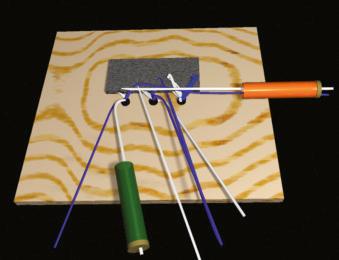
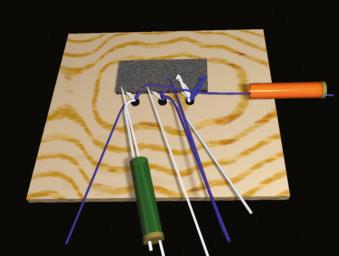
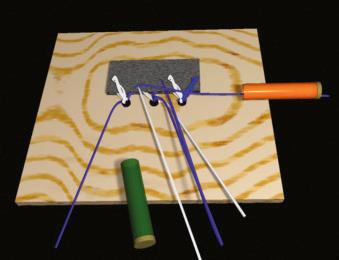
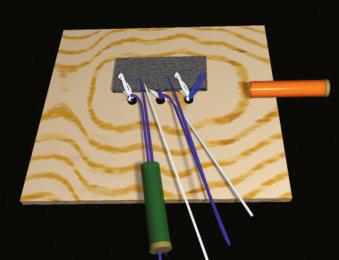
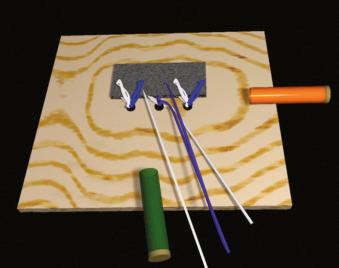
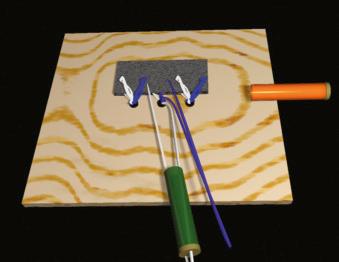
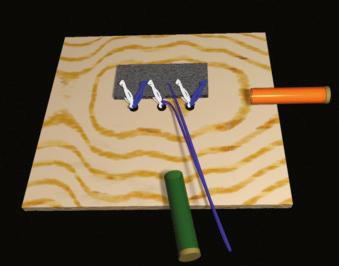
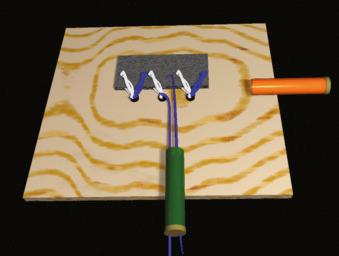
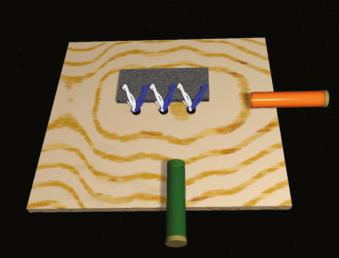
You can practice these steps before you get to the operating room. Simple models can be created with plywood, felt, and picture eyelets to simulate portal locations. Place cannulas through the eyelets and insert an anchor in the center. Practice moving the sutures from cannula to cannula until the motions become automatic (see Figs. 1.24–1.27 and 1.37–1.99 ). Lanny Johnson is fond of saying that when professional golfers finish playing golf, they practice golf; when surgeons finish performing surgery, they practice golf. Perhaps we could learn a lesson from professional golfers. It is amazing to see the progress students make after they practice an operation 20 times.
It is difficult to teach operations of this complexity with only a lecture and a video. Each step (holding the instruments, passing the sutures, suture management, and so forth) must be taught and mastered as an individual event ( Figs. 1.32–1.36 ). These individual events must then be performed in the correct sequence. After the sequence is mastered, the fluidity of the steps must be improved until they become routine. All this should be done under the constant supervision of an experienced arthroscopist so that bad habits are corrected immediately before they become ingrained. Practice does not make perfect, but practice does make permanent, and it is of no benefit to practice an operation either incorrectly or inefficiently.





When I was learning to perform arthroscopic procedures, I drew out the essential steps of the operation on a piece of paper; borrowed a suture passer, knot pusher, crochet hook, loop grasper, sutures, and hemostats from the operating room; and practiced the required maneuvers until I felt comfortable. I have included here the exercises I used and encourage you to rehearse the procedure with your assistant until both of you are familiar with your roles and the necessary steps. Although this may seem time consuming, this level of preparation yields great dividends during the actual operation. Exercise 1 (see Figs. 1.37–1.47 ) simulates a one-anchor, two-suture rotator cuff repair. The steps are written out later in the blue boxes as if it were done with a needle-passing type of device passing the suture. Exercise 2 (see Figs. 1.48–1.66 ) simulates a two-anchor, four-suture rotator cuff repair. Exercise 3 (see Figs. 1.67–1.99 ) simulates a three-anchor, six-suture complex rotator cuff repair. One scenario of clinical steps is described in the blue box for double-loaded suture anchors used for a Bankart repair.
Insert the anchor in the anterior position through the lateral cannula.
Use a crochet hook to pull the blue and white sutures out through the anterior cannula.
Use a crochet hook to pull one blue suture strand from the anterior to the lateral cannula.
Load the blue suture on the needle-passing instrument.
Insert the needle-passing instrument through the lateral cannula.
Grasp the tendon.
Advance the needle and push the blue suture through the tendon.
Withdraw the needle.
Insert a grasper through the anterior cannula and grasp the blue suture exiting the tendon.
Remove the needle-passing instrument from the lateral cannula.
Use a grasper to pull the suture out through the anterior cannula.
Apply a hemostat to the two blue sutures.
Use a crochet hook to pull one white suture strand from the anterior to the lateral cannula.
Load the white suture on the needle-passing instrument.
Insert the needle-passing instrument through the lateral cannula.
Grasp the tendon.
Advance the needle, and push the white suture through the tendon.
Withdraw the needle.
Insert a grasper through the anterior cannula, and grasp the white suture strand exiting the tendon.
Remove the needle-passing instrument from the lateral cannula.
Use a grasper to pull the suture out through the anterior cannula.
Remove the hemostat from the white sutures.
Use the crochet hook from the lateral cannula to retrieve both white sutures from the anterior cannula.
Use a loop grasper to untangle the sutures.
Tie the white sutures.
Remove the hemostat from the blue sutures.
Move the blue sutures from the anterior cannula to the lateral cannula.
Use the loop grasper to untangle the sutures.
Tie the blue sutures.
Insert the arthroscope posteriorly.
Use a spinal needle to identify the anteroinferior portal immediately superior to the subscapularis tendon.
Insert an 8-mm cannula.
Use a spinal needle to identify the anterior-superior portal near where the biceps exits from the rotator interval.
Insert a metal cannula and move the arthroscope anteriorly to view the posterior joint.
Return the arthroscope posteriorly and place a 5.5 mm working cannula anteriorly.
Insert a probe through the anterior-superior cannula to determine the extent of the Bankart lesion.
Insert a shaver through the anterosuperior cannula to débride soft tissue from the anterior scapular neck.
Insert a bur to decorticate the anterior scapular neck.
Remove the anterosuperior cannula.
Insert a metal cannula and trocar into the anterosuperior portal.
Observe the anterior scapular neck decortication.
Move arthroscope to posterior cannula.
Determine how many anchors are required to repair the Bankart lesion.
Mark the anchor locations with a punch or bur.
Insert a drill through the anterosuperior cannula to drill anchor holes.
Insert an anchor through the anterosuperior cannula, and place it in the most inferior drill hole.
Remove the inserter.
Four suture strands from the inferior anchor should be exiting the anterosuperior cannula.
Insert the suture shuttle passing device through the anteroinferior cannula, and pierce the capsule and labrum.
Advance the looped end of the nylon or wire loop passer into the joint.
Retrieve the looped end with a crochet hook placed in the anterosuperior cannula.
Remove the suture shuttle passing device from the anteroinferior cannula, and place a hemostat on the free end that exits the anteroinferior cannula.
The nylon or wire loop should be outside the anterosuperior cannula.
Through the anteroinferior cannula, use a crochet hook to grasp one strand of anchor suture, taking care not to unload the suture from the anchor.
Through the anterosuperior cannula, insert a loop grasper, and encircle the looped end of the nylon passing suture or the wire loop and the other end of the suture that was pulled out the anteroinferior cannula.
Place 6 cm of this designated suture through the nylon or wire loop (anterosuperior cannula).
Apply traction to a hemostat, and pull the designated anchor suture from the anterosuperior cannula into the joint, through the labrum, and out the anteroinferior cannula.
Two sister limbs of the same suture are now through the anteroinferior cannula.
Tie the two limbs together.
Repeat for the second set of sutures from the most inferior anchor.
Repeat these steps from additional anchors as needed.
Because reconstructive arthroscopic shoulder surgery involves soft tissue repair, knot tying is a critical skill. Surgeons' reluctance to tie arthroscopic knots has created a booming industry in pretied knots or “knotless” devices. Each of these devices requires a number of steps that may be as tedious as tying a knot. Furthermore, these devices are not always available and have an associated cost that may make them less appealing. Learning to tie an arthroscopic knot can be difficult, but with instruction and practice, it can be mastered. Surgeons tie knots in open surgery on a daily basis. Arthroscopic knots are similar, with the exception that the knot pusher replaces the surgeon's index finger. The knots can lie flat as square knots or they can be a series of half hitches with alternating configurations. If done correctly, arthroscopic knots are as strong as knots tied in the open technique. Knotless anchors certainly have their place and can offer features that make them superior to traditional knot tying in specific scenarios, but it is always useful to have the skill to tie a knot in those situations when something goes awry and you need to use your knot-tying skills.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here