Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The diagnosis of a finger devascularization, single or multiple, should be made upon admission of the patient because it defines the degree of urgency.
Revascularization consists of restoring arterial inflow and venous return. It is undertaken once the skeleton has been stabilized. Osteosynthesis, by restoring the length, defines the need for and length of potential grafts.
The reconstruction strategy, however, must be fully defined before the start of the intervention. There is no point in using long vein grafts to restore arterial flow if a solution has not been found to ensure the skin coverage of these grafts.
The signs of devascularization (pallor, cold, delayed capillary return) are sometimes hard to detect in an emergency. This is because of pain and the presence of blood or clots that mask skin color. When these conditions are present, pulp refill is a reliable sign. Pinched between the thumb and index finger of the examiner, the pulp of a devascularized finger only reexpands very slowly. This phenomenon reflects the emptying of the pulp venular capacitance system, a system whose filling is no longer guaranteed because of the interruption of arterial supply.
The presence and significance of visible hemorrhage is indirect and insufficient evidence. In the case of a complete laceration of a digital artery, spasm occurs quickly, which interrupts blood flow. In the case of a palmar wound of a finger with devascularization, division of both digital arteries is always accompanied by division of the two palmar digital nerves because of the close anatomic relationship of these structures in the neurovascular bundles. In this case, pulpal anesthesia is always present. For the same reason these palmar digital injuries with devascularization are always accompanied by a laceration of the flexor tendon. In the case of more proximal trauma in the wrist, devascularization implies a simultaneous laceration of the radial and ulnar arteries. Associated tendon and nerve injuries are usually also present there.
In the case of subtotal amputation of a finger the persistence of a narrow skin bridge is often enough to ensure venous return. It must be preserved because it includes one or two superficial veins. In more proximal lesions it is rare that such a skin bridge is sufficient for venous return. It should also be preserved, but venous repair is still required. Clinically, venous congestion is only evident if the arterial flow has been preserved. These circumstances (preserved arterial flow, interruption of venous return) occur only rarely. The most classic case is represented by ring avulsion injuries. In stage IIA of Nissenbaum's classification, modified by Urbaniak, the injuries are mostly dorsal, but the superficial venous network is interrupted circumferentially. The finger in question appears blue and turgid and demonstrates rapid capillary return.
Paradoxically the urgency here is greater than for a total amputation. The devascularized part is delivered in “warm” conditions of ischemia because it is difficult to refrigerate in practice.
In fact, cold preservation is discouraged because however it is done, it also carries the risk of cooling the proximal stump, which sometimes causes prolonged spasms. In these conditions of warm ischemia it is preferable for revascularization to be done before the sixth hour. The presence or absence of skeletal muscle tissue in the devascularized part is one of the major factors determining tolerance to ischemia. Digital devascularization therefore accommodates prolonged ischemia better than more proximal injuries to the wrist, which carry the risk of intrinsic muscle necrosis.
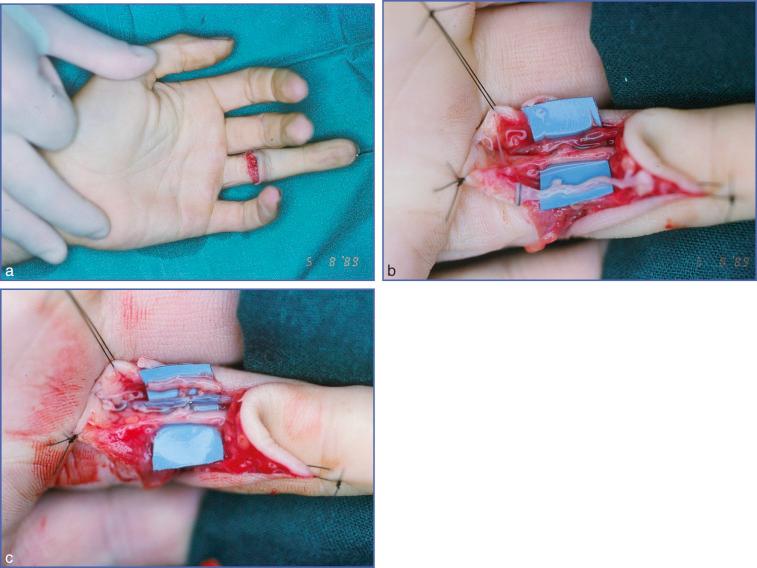
When faced with complex trauma, combining skin, pedicle and tendon injuries, revascularization follows osteosynthesis. It is easier to proceed to microsurgery after the skeleton has been stabilized. This rule applies to the common situation where devascularization arises from a palmar wound. The initial wound is extended, and we first repair the pedicle elements before proceeding to suturing the flexor tendons. It is recommended to place the finger in full extension before any tendon repair. The length of any potential graft is then measured in this position.
Where local conditions allow it, end-to-end arterial repair is performed. Both arteries must be examined in turn under the microscope. A perpendicular section of the vessel is performed using microscissors, eliminating the contused segment. At the end of this debridement and after circumferential adventicectomy (see Chapter 15 ), inspection of the vessel end should show a healthy wall of normal tone without parietal delamination. When resection is limited, which is the case in clean lacerations, the restoration of arterial flow is provided by a single end-to-end suture. Dissection of both proximal and distal vascular ends makes this suture possible without excessive tension.
When both palmar digital axes can be repaired by direct end-to-end suture, we anastomose both arteries. It is rare that the two arteries remain patent in the long term.
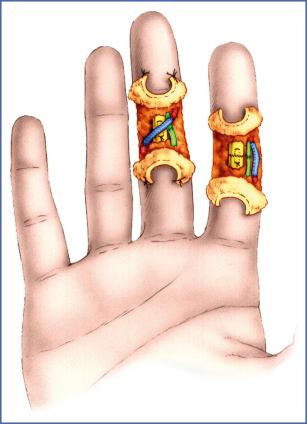
Most often only one of the two anastomoses ensures survival of the finger. Local observations (vessel size, quality of anastomosis) do not predict with certainty which side takes on this role. When only one of the two digital arteries is accessible to a direct repair, this one alone is responsible for the arterial supply to the injured finger. Indeed, it is unusual to combine a repair on one side and a graft on the other for the same finger. This would only be considered if the suture involves a minor digital artery of a smaller size than that of the contralateral digital artery. Finally, when a direct suture is not possible on either of the two digital arteries, the possibility of a crossed repair should be considered. This becomes possible when laceration of both pedicles occurs at different levels.
The digital artery with the most distal interruption can be dissected so as to enable it to be diverted, crossing the median line of the finger to then be anastomosed to the proximal stump of the other digital artery. This technique avoids the hazards of a graft. However, it is only advised if no further palmar procedure (tenolysis, nerve grafts, etc.) is expected in the future, because the risks of an accidental injury to this artery would be high.
In cases when a direct or, more rarely, a crossed repair is not possible, revascularization requires a vein graft. It is the superficial veins of the anterior aspect of the forearm that provide the graft. One of these longitudinal veins is selected. Dissection involves careful hemostasis of all of the transverse branches by clip or ligature. A heparinized saline wash verifies the patency of the graft. This is reversed 180 degrees to take the presence of the valves into account. It is then cut again on demand. The length of the graft to be used must be carefully measured. If it is too long, a kinking effect will result that is responsible for thrombosis. If it is too short, it will put the sutures under tension, which will cause leakage and thrombosis. These superficial veins shrink considerably once they have been released from the donor site. The ideal scenario is to accurately measure their length before removal, then restore this length by axial tension before proceeding to the final recut. The end-to-end sutures on both sides, which restore the continuity of the arterial axis, must “manage” the size incongruence ( Figs. 8.1–8.3 ).
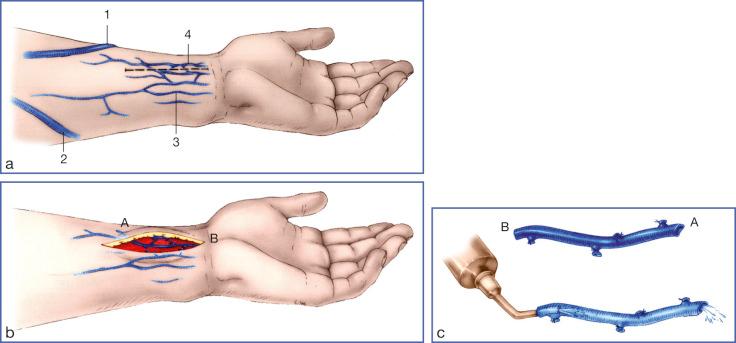

This incongruence is especially manifest at the distal anastomosis because of the reversal of the vein graft. The distribution of sutures is of utmost importance here (see Chapter 15 ). There is no steadfast rule dictating the order in which the sutures must be placed. We usually start with the distal suture, which is the most technically demanding. The graft, which is still free, can then be manipulated to facilitate placement of this first suture. After completion of this graft, the other digital artery is clipped or ligated at each of its two ends.
In the same way that a “crossed” repair is sometimes the only option, some cases may require a “crossed” graft to be performed ( Fig. 8.4 ). This is the case when the most favorable proximal and distal vascular ends are located on different sides of the finger. The same caution should be exercised when a secondary surgical procedure is envisaged.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here