Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Only a few skin disorders are surgically important, including unsightly lesions, lumps and potentially malignant lesions. These are often referred to surgeons for excision or for definitive management following biopsy. Lower limb ulcers in the West are usually venous, arterial or diabetic neural and/or ischaemic in origin (see Chapter 41, Chapter 43 ). Leg ulcers in the tropics often have a bacterial origin. Ulceration is also a characteristic of malignant skin lesions.
Surgical skin disorders are often referred to a dermatologist, but still comprise about 15% of new general surgical outpatient referrals. Many require only excision biopsy under local anaesthesia. Others are referred for advice after a lesion has been excised by a family practitioner.
Most skin malignancies are ideally managed by a multidisciplinary team (MDT) of surgeons, dermatologists, oncologists, pathologists and sometimes radiologists and specialist nurses.
A small proportion of skin lesions have a potentially sinister course, notably malignant melanoma (MM). These comprise around 5% of skin cancers in the United Kingdom but account for most skin cancer deaths (75%). The incidence of all skin cancers (melanoma, basal cell carcinoma [BCC] and squamous cell carcinomas [SCCs]) and their premalignant stages increases with sun exposure and is highest in fair skinned people. The frequency of all skin cancers is rising in the West with increasing foreign travel, and in sunny countries like Australia, they have reached epidemic proportions.
Finally, the nails, which are specialised skin appendages, pose surgical problems in the form of infected ingrowing toenails and onychogryphosis . The rare subungual melanoma is an important diagnosis, which must not be missed.
The skin is the largest organ in the body and its main functions are protection, regulation and sensation . The skin protects against mechanical forces, such as pressure and abrasion; ultraviolet light and heat; and acts as a barrier against pathogens. Regulation functions include temperature (via vasodilatation and constriction, and sweating), metabolism of vitamin D and preventing fluid losses, whilst sensation include touch, pressure, itch and pain.
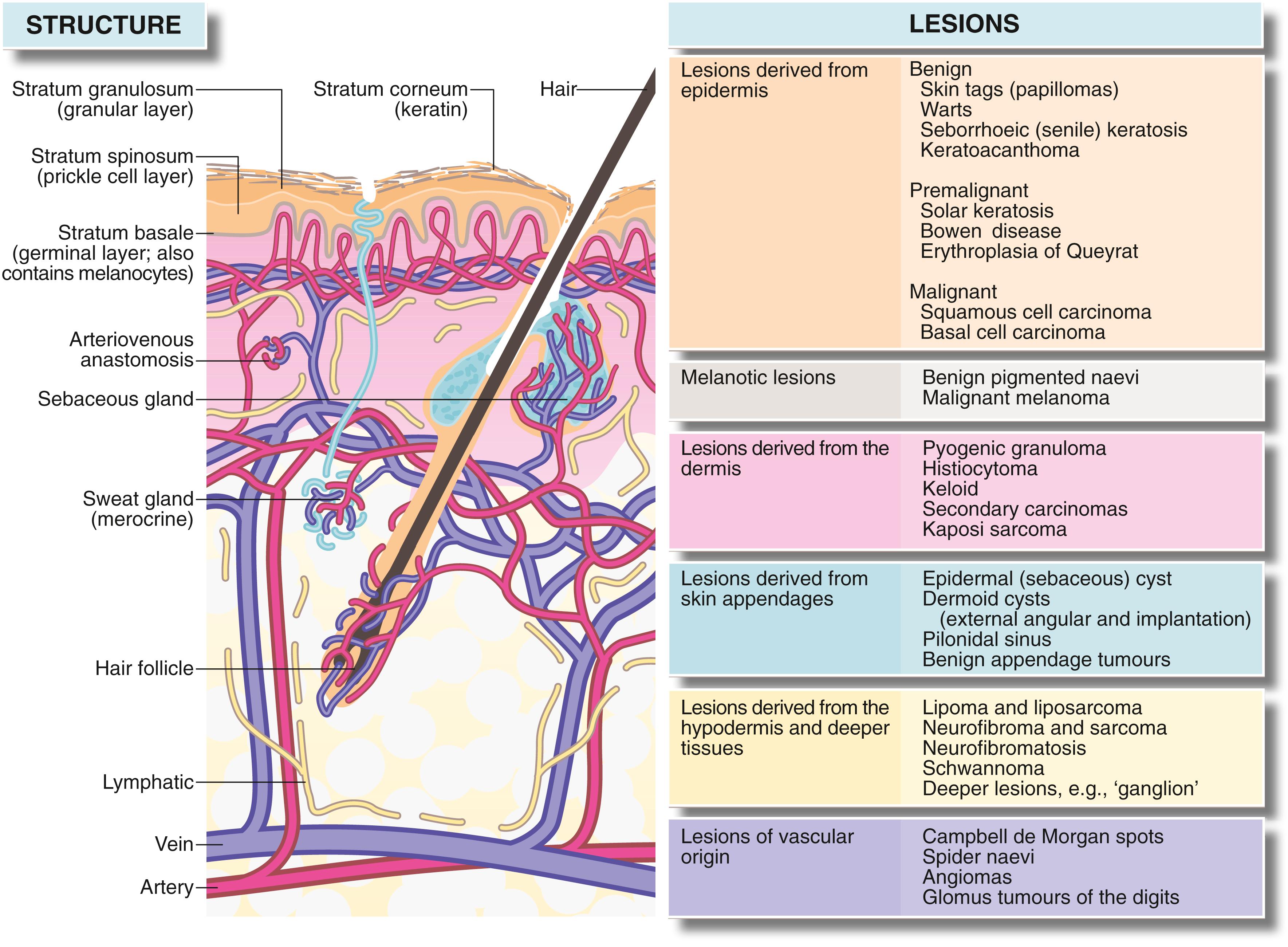
The skin has three main strata, the epidermis (the protective waterproofing layer), the dermis and the hypodermis:
The epidermis has four layers—from the base outwards: basal, prickle-cell, granular and keratin layers. Cell division normally occurs only in the basal layer.
The dermis consists of papillary and reticular layers , separated by a vascular (middermal) plexus. The dermis contains keratinocytes and collagen and elastin fibres produced by fibroblasts, and also ground substance composed mainly of glycosaminoglycans.
The deepest layer is the hypodermis , consisting of loose fibrofatty tissue and containing skin appendages—sweat glands (mainly eccrine), apocrine glands (sweat glands in armpits, groins and around nipples), hair follicles and associated sebaceous glands. The skin is generally mobile over deeper structures, because the hypodermis is only loosely connected to the superficial fascia, but is tightly bound to fascia in the palms, the soles of the feet and the scalp.
Collagen in the deeper reticular layer provides much of the skin’s strength, while the elastin contributes to its elasticity. Both layers are well vascularised and rich in nerve endings. The orientation of collagen and elastin fibres in the dermis determines lines of skin tension known as Langer lines . These are surgically important because incisions parallel to them heal with minimal scarring.
As the incidence of skin cancers continues to rise in all adult age groups, the numbers of patients referred with skin lesions also increases. Patients may be concerned by changing appearances of a lesion, such as size, shape or colour; or changes in its behaviour, such as pain, bleeding or ulceration. Assessing any new skin lesion begins with a clinical history and examination, to formulate a differential diagnosis and management plan.
Pertinent questions about the skin lesion include:
How long has the lesion been present?
How is it changing?
Is it getting bigger?
Is any size increase slow or rapid?
Is it itchy?
Is it painful?
Is there any bleeding or other discharge?
Is there any change in colour?
Past history includes any previous skin lesions, surgery or trauma to the affected area. Previous skin cancer makes this diagnosis more likely, whilst surgery or trauma can lead to implantation cysts, keloid scarring or a chronic inflammatory response to a foreign body. The history should also seek disorders predisposing to infection or causing immunosuppression. Previous radiotherapy can increase the risk of skin cancer.
Family history can direct the diagnosis towards rarer genetic disorders, such as neurofibromatosis, Muir-Torre and tuberous sclerosis. There may also be a genetic link in some melanomas.
Social history should include occupational details (environmental exposures to carcinogens increase the risk of BCC and SCC). The sun exposure history can be clarified by questions about work, living abroad or frequent sunny holidays. Previous service in the armed forces may have included deployment to tropical climates. When dealing with suspected melanomas in particular, a history of childhood sunburn is important. Chronic ulcers may be contracted during foreign travel or after injury, and with chronic nonhealing wounds and burns, there is a small risk of malignant transformation.
Drug history —immunosuppressive therapies may be relevant
The lesion should be examined in detail with an A–E Assessment:
A symmetry
B order
C olour
D iameter
E levation/evolution
Other characteristics, including consistency, mobility and tenderness, should also be assessed and documented ( Table 46.1 ). A top to toe examination should then be carried out, searching for other similar lesions, lymphadenopathy or sources of primary malignancy elsewhere that has metastasised to skin. The glabrous (nonhairy) surfaces of hands and feet and the nails should be examined for melanotic lesions.
| Symptoms and Signs | Diagnostic Significance |
|---|---|
|
Epidermal lesions (such as warts) usually have a surface abnormality but deeper lesions are usually covered by normal epidermis. A punctum suggests the abnormality arises from an epidermal appendage, for example, epidermal (sebaceous) cyst |
| Depth within the skin Superficial and deep attachments Which tissue is the swelling derived from? |
Tends to reflect the layer from which lesion is derived and therefore the range of differential diagnosis (i.e., epidermis, dermis, hypodermis or deeper) |
| Character of the margin Discreteness, tethering to surrounding tissues, three-dimensional shape |
A regular shaped, discrete lesion is most likely cystic or encapsulated (e.g., benign tumour). Deep tethering implies origin from deeper structures (e.g., ganglion). Immobility of overlying epidermis suggests a lesion derived from skin appendage (e.g., epidermal cyst) |
| Consistency Soft, firm, hard, ‘indurated’, rubbery |
Soft lesions are usually lipomas or fluid-filled cysts. Most cysts are fluctuant unless filled by semisolid material (e.g., epidermal cysts), or the cyst is tense (e.g., small ganglion) Malignant lesions tend to be hard and irregular (‘indurated’) with an ill-defined margin caused by invasion of surrounding tissue Bony-hard lesions are either mineralised (e.g., gouty tophi) or consist of bone (e.g., exostoses) |
| Pulsatility | Pulsatility is usually transmitted from an underlying artery, which may simply be tortuous or may be abnormal (e.g., aneurysm or arteriovenous fistula) |
| Emptying and refilling | Vascular lesions (e.g., venous malformations or haemangiomas) empty or blanch on pressure and then refill |
| Transilluminability | Lesions filled with clear fluid, such as cysts ‘light up’ when transilluminated |
| Temperature | Excessive warmth implies acute inflammation, for example, pilonidal abscess |
|
These symptoms often indicate acute inflammation. Pain also develops if a noninflammatory lesion becomes inflamed or infected (e.g., inflamed epidermal cyst). Malignant lesions are usually painless |
|
Malignant lesions and keratoacanthomas tend to ulcerate as a result of central necrosis. Surface breakdown also occurs in arterial or venous insufficiency (e.g., ischaemic leg ulcers), chronic infection (e.g., tuberculosis or tropical ulcers) or trauma, particularly in an insensate foot |
| Character of the ulcer margin | Benign ulcers—the margin is only slightly raised by inflammatory oedema. The base lies below the level of normal skin Malignant ulcers—these begin as a solid mass of proliferating epidermal cells, then the centre eventually becomes necrotic and breaks down. The margin is typically elevated ‘rolled’ and indurated by tumour growth and invasion |
| Behaviour of the ulcer | Malignant ulcers expand inexorably (though often slowly), but may go through cycles of breakdown and healing (often with bleeding) |
Normal colour |
If a lesion is covered by normal-coloured skin, then the lesion must lie deeply in the skin (e.g., epidermal cyst) or deep to the skin (e.g., ganglion) |
| Red or purple | Redness implies increased arterial vascularity, which is most common in inflammatory conditions, like furuncles. Vascular abnormalities which contain a high proportion of arterial blood, such as Campbell de Morgan spots or strawberry naevi are also red, whereas venous disorders, such as port-wine stain are darker. Vascular lesions blanch on pressure and must be distinguished from purpura or haematoma, which does not |
| Deeply pigmented | Benign naevi (moles) and their malignant counterpart, malignant melanomas, are nearly always pigmented. Other lesions, such as warts, papillomata or seborrhoeic keratoses may become pigmented secondarily. Hairy pigmented moles are almost never malignant. Rarely, malignant melanomas may be nonpigmented (amelanotic). New darkening of a pigmented lesion should be viewed with suspicion, as it may indicate malignant change |
|
Keratoacanthoma, warts and pyogenic granuloma may all develop rapidly and eventually regress spontaneously. When fully developed, these conditions may be difficult to distinguish from malignancy. Spontaneous regression marks the lesion as benign |
|
In certain rare syndromes, multiple similar lesions develop over a period. Examples include neurofibromatosis and recurrent lipomata in Dercum disease. Prolonged or intense sun exposure predisposes a large area of skin to malignant change. Viral warts may appear in crops. Malignant melanoma may spread diffusely (superficial spreading melanoma) or produce satellite lesions via dermal lymphatics |
|
Some skin lesions arise much more commonly in certain areas of the body. The reason may be anatomical (e.g., pilonidal sinus, external angular dermoid or multiple pilar cysts of the scalp) or because of exposure to sun (e.g., solar keratoses or basal cell carcinomas of hands and face) |
|
Congenital vascular abnormalities, such as strawberry naevus or port-wine stain may be present at birth. Benign pigmented naevi (moles) may be detectable at birth, but only begin to enlarge and darken after the age of 2 years |
The lesion in question should ideally be photographed and dermoscopy performed to examine it in detail, assessing its pigmentation and vascularity and seeking features of malignancy. If skin malignancy is suspected, regional lymph node basins should be examined.
Many skin lesions can be diagnosed from the history and clinical examination alone. If there is concern about malignancy, a biopsy should be performed. Incision and excision biopsy techniques are illustrated in Chapter 10 , p. 14, and Box 46.1 summarises surgical options for skin conditions.
Simple excision or other physical methods, for example, electrocautery, laser therapy or cryotherapy—for small, obviously innocent lesions.
Excision biopsy —if there is any risk of malignancy or the clinical diagnosis is doubtful (only for small lesions).
Incisional biopsy —for large lesions, where only a representative section is removed. Definitive therapy is then planned according to the histology.
Wide local excision with or without skin grafting—for malignant melanomas and sometimes for other large malignant lesions.
Radiotherapy —an alternative to excision for basal cell carcinoma and primary squamous cell lesions. Also sometimes used if regional lymph nodes are involved in squamous cell carcinoma.
Topical chemotherapy —with 5-fluorouracil cream (or other agents) for certain skin malignancies.
Photodynamic therapy —for certain skin malignancies. Malignant cells absorb a photosensitising chemical, which reacts with light of a particular wavelength applied locally to destroy the cells.
Surgical lymph node clearance —if nodes are involved by malignant melanoma or squamous carcinoma.
An excision biopsy takes an ellipse of skin with a 2-mm or so margin of normal tissue and an underlying cuff of fat. The ellipse should be placed along natural skin tension lines to enable the skin edges to be readily opposed. All excised lesions should be sent for histological evaluation. For large lesions, an incisional biopsy can be taken or, if facilities allow, the lesion can be excised and a dressing placed on the wound awaiting histological confirmation of clearance.
Following the diagnosis, management may involve other members of a MDT as well as deciding on long-term follow up.
Skin tags or squamous papillomas are small benign polypoid lesions consisting of loose connective tissue covered by epithelium. They are common in adults and occur particularly on the trunk, face, neck, axillae and groins. Although benign, they can be irritated by clothing or jewellery and cause bleeding. Nonsurgical management includes cryotherapy (freezing) or tying a thread around the base and so the tag becomes ischaemic and falls off. A surgical approach is narrow-margin excision under local anaesthesia.
Warts are small, virus-induced epidermal lesions (frequently caused by human papillomavirus or HPV), which present as epidermal thickening with hyperplasia and hyperkeratosis, plus enlarging dermal papillae known as papillomatosis . Morphology varies with location. The common wart (verruca vulgaris), is a papilliferous lesion up to 1 cm across, most often found on the fingers and back of the hands. Warts are often multiple in children, and can occur on the face, where the lesions are often less keratotic and have a smoother, more dome-like shape. They are often called juvenile or plane warts (verruca plana juvenilis). Lesions on the sole of the foot, plantar warts (verruca plantaris), become very keratotic and flattened by pressure. They may extend deeply into the foot and cause pain. Warts may also occur on the genitalia, perineum and perianal area. These originate from HPV infection and are usually spread by sexual contact. Genital warts sometimes grow large and are then known as condylomata accuminata .
Warts are common in immune-suppressed patients. They can grow and regress spontaneously over months and years. Most are managed conservatively with topical antiviral creams or ointments. If inadequate, other measures include cryotherapy, laser treatment or surgical excision. National Institute for Care and Health Excellence (NICE) guidance also considers that photodynamic treatment may be of benefit.
Seborrhoeic keratoses ( seborrhoeic warts ) or basal cell papillomas, are very common in older patients and arise primarily on the torso and neck. The patient may present with multiple different sized lesions, with varying pigmentation. Lesions appear waxy and raised with a ‘stuck on’ appearance and keratotic plugs on the surface ( Fig. 46.2 ).

Histologically, there are several types, which can be classified as acanthotic, hyperkeratotic, clonal, reticulated or irritated. Owing to the superficial nature of the lesion, they can be ‘scraped off’ with a curette or scalpel under local anaesthesia. Alternatively, they can be treated with cryotherapy, electrocautery or laser.
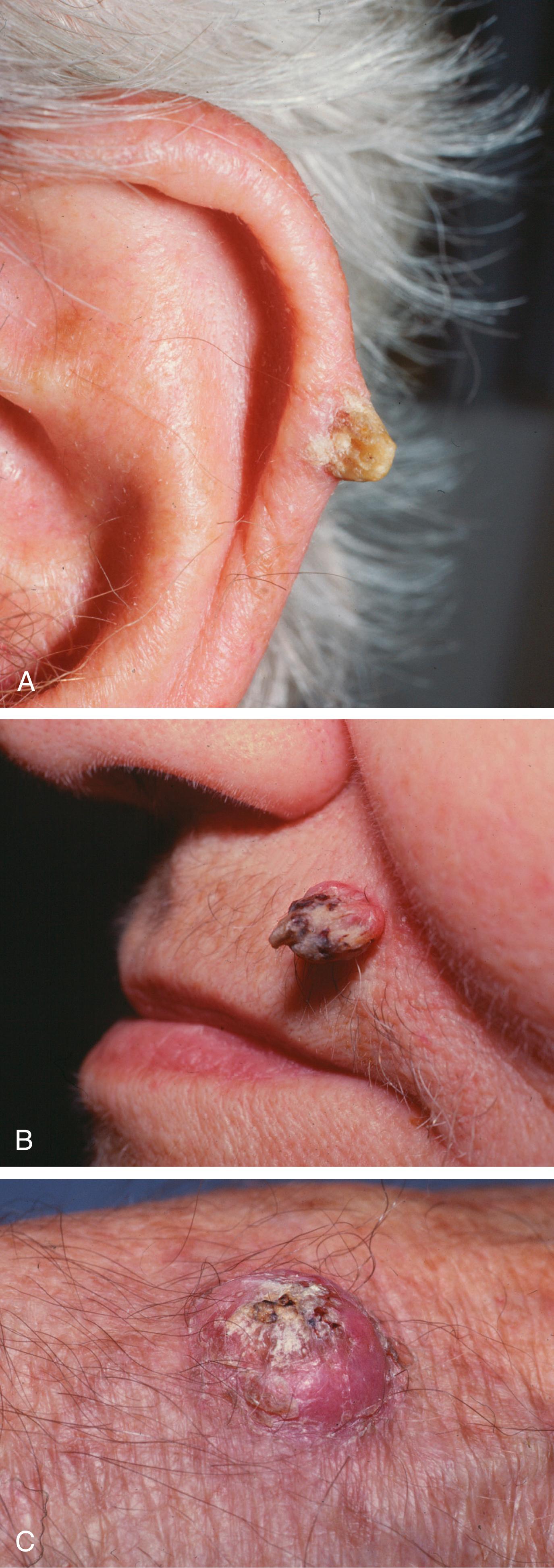
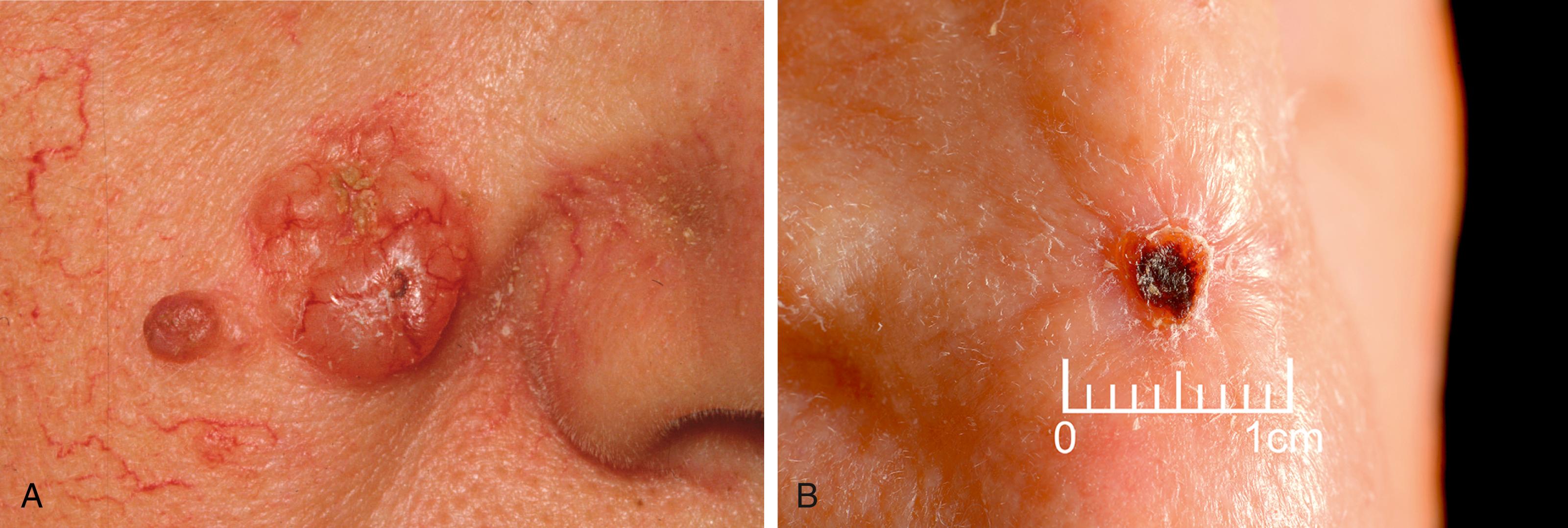
Keratoacanthoma (KA) is an epithelial tumour that can present as a nodular skin lesion with well-defined, raised edges and an irregular central crater containing keratotic debris. Previously considered completely benign, pathologists are moving towards considering them a form of low-grade SCC. They typically have a rapid acute growth phase, and then regress spontaneously over a few weeks. When seen during the growth phase, it can be clinically difficult to distinguish from an SCC, and it is a brave surgeon who opts to wait for the lesion to involute.
If the lesion is regressing, watching and waiting is acceptable, but one should have a low threshold for biopsy if there is diagnostic uncertainty. It can be difficult to distinguish even histologically between KA and well-differentiated SCC, and these cases should be managed as for SCC.
Keratin (cutaneous) horns may look similar but rarely regress ( Fig. 46.3 ). They tend to arise in older people.
Melanocytes are derived from the neural crest during embryological development and are located in the basal layer of the epidermis. They synthesise melanin and distribute it to nearby epidermal cells, where it is responsible for skin colour. A localised collection of melanocytes confined to the epidermis is known as a freckle or lentigo . If a cluster of normal melanocytes enters the dermis, this is known as a naevus (plural naevi).
Naevi can be classified into naevus cell naevi (subdivided into congenital, acquired or special naevi), and melanocytic naevi , which may be epidermal or dermal.
Congenital naevus cell naevi are either giant (projected to be reach >20 cm in adulthood) or nongiant congenital melanocytic naevi . Giant naevi used to be considered at risk of malignant transformation, and young children were offered excisional surgery. However, this risk has proved relatively low. So operation is not offered for risk reduction, but the lesion is monitored for changes in appearance or new symptoms, such as bleeding in any area of it. In this case, a biopsy of the troublesome area should be performed.
Acquired naevus cell naevi are of three main types—junctional, compound and intradermal. These are rare in infancy and can appear up to the age of about 50 years. New naevi that develop after the age of 50 should be considered suspicious. The pigmentation of acquired naevi can change with age but the pattern remains the same.
Special naevus cell naevi include Spitz, atypical and halo naevi . Spitz naevi tend to occur in young adults, and clinically, can appear similar to melanomas. Excision biopsy is recommended to make or confirm the diagnosis.
A lentigo (plural = lentigines) is a flat pigmented lesion. All, except freckles, maintain their pigmentation in the absence of sun exposure. There are several types including simple lentigo, café-au-lait patches and Becker naevi, all of which are benign. However, lentigo maligna is a premalignant lesion containing abnormal melanocytes confined to the epidermis (and is a precursor of lentigo MM). Lentigenes are different from freckles (ephelis) in that they contain increased numbers of melanocytes and show hyperplasia, whereas freckles just have increased melanin. Solar lentigo are commonly referred to as ‘liver spots’ and occur on the face and hands of older patients.
This category includes Mongolian blue spots, naevi of Ota and Ito (typically present at birth) and blue naevi, which tend to appear in childhood or young adulthood. They are all characterised by melanocytes in the dermis and thus present with bluish pigmentation. They are thought to result from failure of normal melanocyte migration from the embryonic neural crest to the epidermal basal layer.
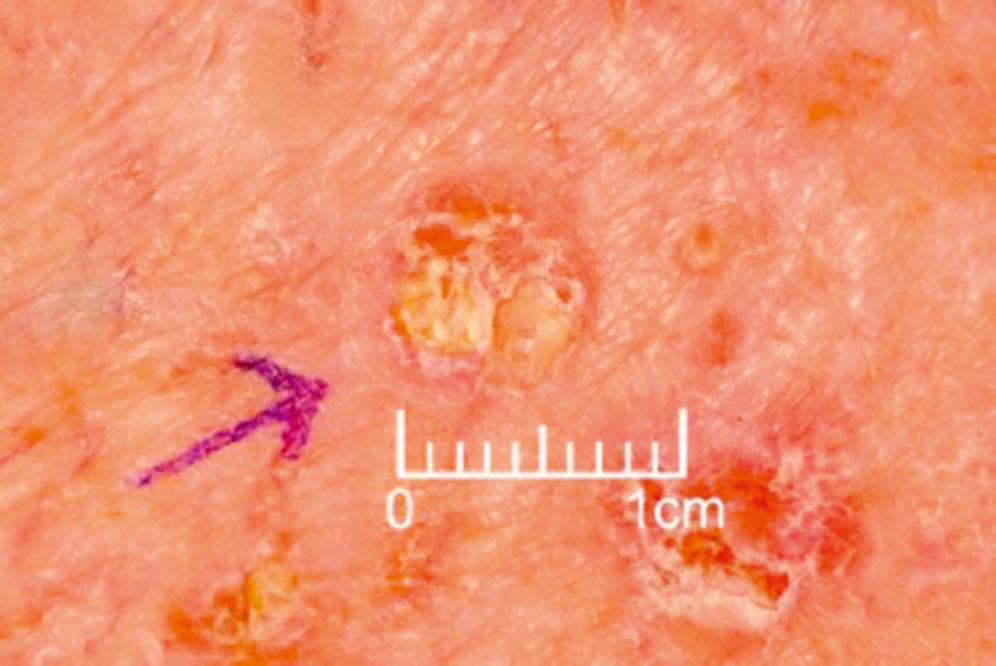
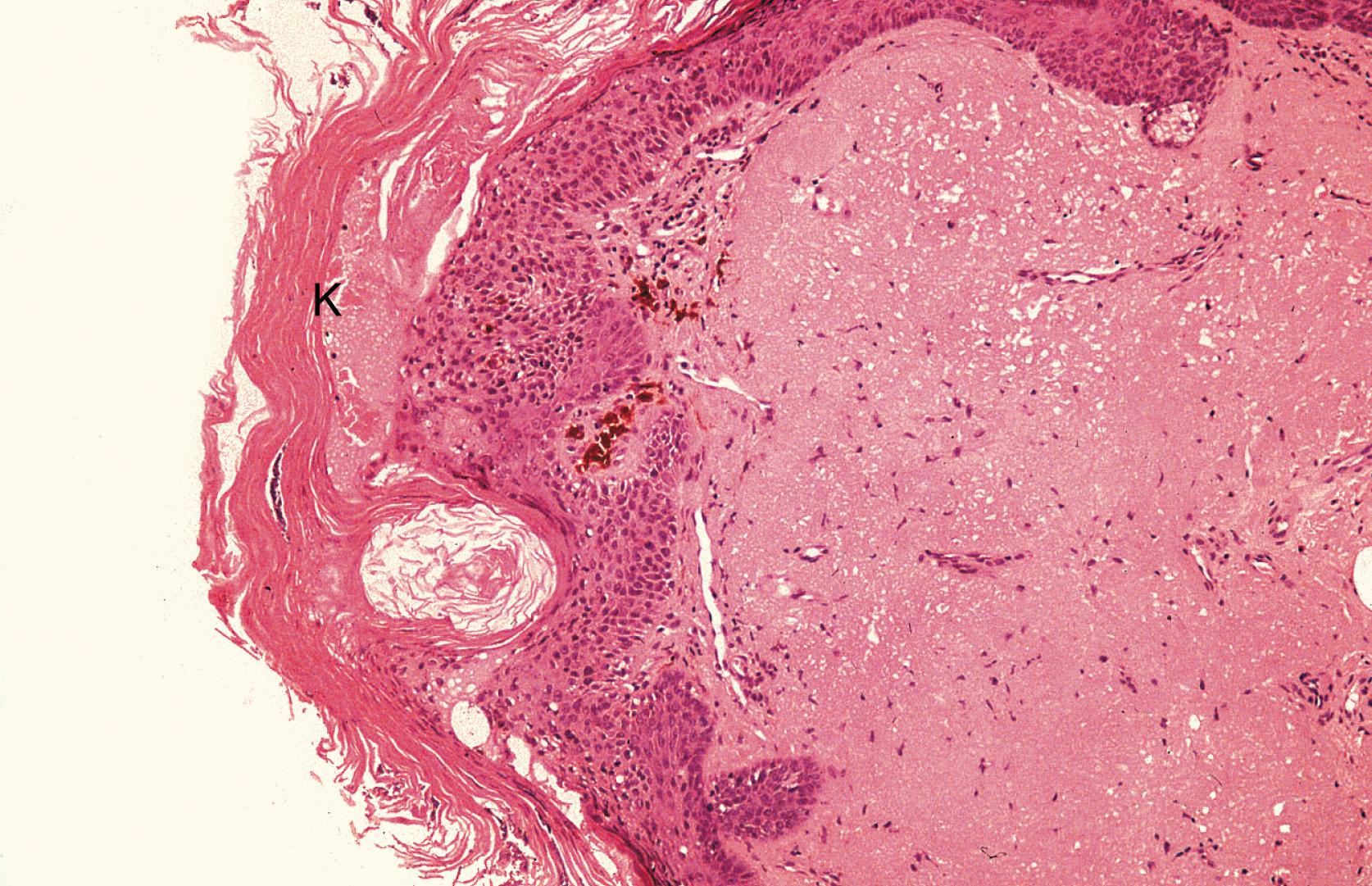
Actinic keratoses (AK) are flat, well-demarcated, brown, scaly or crusty lesions with an erythematous base ( Fig. 46.4 ). They bleed easily, if traumatised or scratched, and are frequently found as multiple patches on sun-exposed surfaces, such as the face, neck and upper limb. On histology, there is hyperkeratosis and acanthosis, with a variable degree of dysplastic change and abnormal mitotic activity deep in the epidermis ( Fig. 46.5 ). Although these features suggest malignant transformation, the basal layer remains intact, thus AK is managed as a premalignant condition, predisposing to squamous carcinoma. However, not all actinic keratotic patches will progress to a malignancy.
These lesions look similar to AK, but histology shows dysplastic changes extending the full thickness from basal layer to the surface, yet without invasion. The lesion is termed carcinoma-in-situ, also known as Bowen disease ( Fig. 46.6 ). The aetiology is cumulative sun exposure and though it typically occurs on sun-exposed sites, it can occur on other parts of the body. Eczema unresponsive to topical treatments could be Bowen disease and thus a biopsy should be performed.

When Bowen disease occurs on the glans penis, it is known as erythroplasia of Queyrat .
Conservative management includes advice on limiting sun exposure and using sun screen skin protection. Patient choice may be to watch and wait with regular follow-up for possible invasive SCC, but medical treatment with topical 5-fluorouracil or imiquimod cream is possible, either alone or in combination. Alternative options include cryotherapy, curettage or excision.
Lentigo maligna are slowly-growing lesions confined to the epidermis (also known as melanoma-in-situ ), which can transform to become invasive MM. Lesions have an indeterminate edge even under dermatoscope evaluation and can have varying pigmentation across their width. These are best managed by surgical excision, taking a 5-mm margin of healthy tissue to reduce the risk of local recurrence. A large resulting defect may need reconstructing with a skin graft or flap, depending on the site of the lesion.
Cutaneous SCCs (cSCCs) occur anywhere on the skin, particularly in areas repeatedly exposed to ultraviolet light, and usually in older age groups. Historically, cSCCs developed in skin chronically exposed to industrial carcinogens, such as arsenic or chromium compounds, soot, tar, pitch or mineral oils. Examples include carcinoma of the scrotum in chimney sweeps in the 19th century, with soot as a predisposing factor, whilst smokers are at risk for developing SCCs on the lips.
Chronic inflammation in chronic nonhealing burn wounds, osteomyelitis sinuses or longstanding ulcers predisposes to SCC. These SCCs are termed Marjolin ulcers and tend to have a worse prognosis. Other risk factors for cSCCs include long-term immunosuppression, such as therapeutic in transplant patients and in those with leukaemias and lymphomas.
cSCC can present clinically as an enlarging painless ulcer with a rolled, indurated (hardened) margin. In other cases, lesions can have an exophytic (outward growing, proliferative) cauliflower-like appearance with areas of ulceration, bleeding or serous exudation. cSCCs can invade deeper tissues and metastasise, so it is important to determine whether the lesion is fixed to underlying structures, such as bone or cartilage and to examine the regional lymph nodes for spread.
Several histological subtypes are described. Microscopically, there is invasion of dysplastic keratinocytes (with varying differentiation) throughout the stratum basale to the dermis. The cells tend to form concentric layers, giving the appearance of keratin pearls. On dermoscopy examination, there may be glomerular or irregular vascular patterns and areas of erosion and ulceration. Clinically and even histologically, well-differentiated cSCCs can appear similar to KA ( Fig. 46.7 ).

Cutaneous SCCs are graded using Broder ratio of differentiated to undifferentiated cells, and staged using Tumour Node Metastasis (TNM) classification. Lesions with poorly differentiated cells on histology, or perineural or perivascular invasion are more likely to recur and metastasise. Cutaneous SCCs are thus classified as low-risk or high-risk, according to the risk of recurrence and metastasis. High-risk cSCCs tend to have the following characteristics:
Size—diameter >2 cm
Site—ear, lip, central face, non-sun-exposed sites, within chronic wounds
Patient immunosuppressed
Histological features—tumour thickness >4 mm, poorly differentiated histology, or with invasion of the subcutaneous tissue, nerves and blood vessels
Surgical excision is appropriate in most cases, with the margin width determined following a biopsy, and discussion at a specialist skin cancer MDT. In low risk tumours (<2 cm), a 4-mm peripheral margin is usually sufficient. In larger or high-risk lesions, a 6-mm peripheral margin is needed. If the lesion is large and has an indistinct border, Mohs micrographic surgery (MMS) can be carried out to preserve more normal tissue in cosmetically sensitive areas, such as around the eyes or nose, or in cases of recurrence, where the lesion edge is ill-defined. The principle is to take smaller margins with the initial lesion, rapidly freezing the lesion for immediate histology and depending upon the presence of remaining tumour, for further margins to be excised as necessary. This process is repeated until clear margins are obtained.
In cosmetically sensitive areas, such as the lip, radiotherapy alone is an option. For smaller, well-defined low risk lesions, alternative options include cryotherapy, curettage and cautery.
There is evidence to show that 75% of local recurrences and metastatic disease will be detected within the first 2 years, and up to 95% in the first 5 years, thus recommended follow up of cSCC is generally 3- to 4-monthly for the first 2 years, then 6-monthly for a further 3 years to a total of 5 years. This may vary according to specific tumour factors.
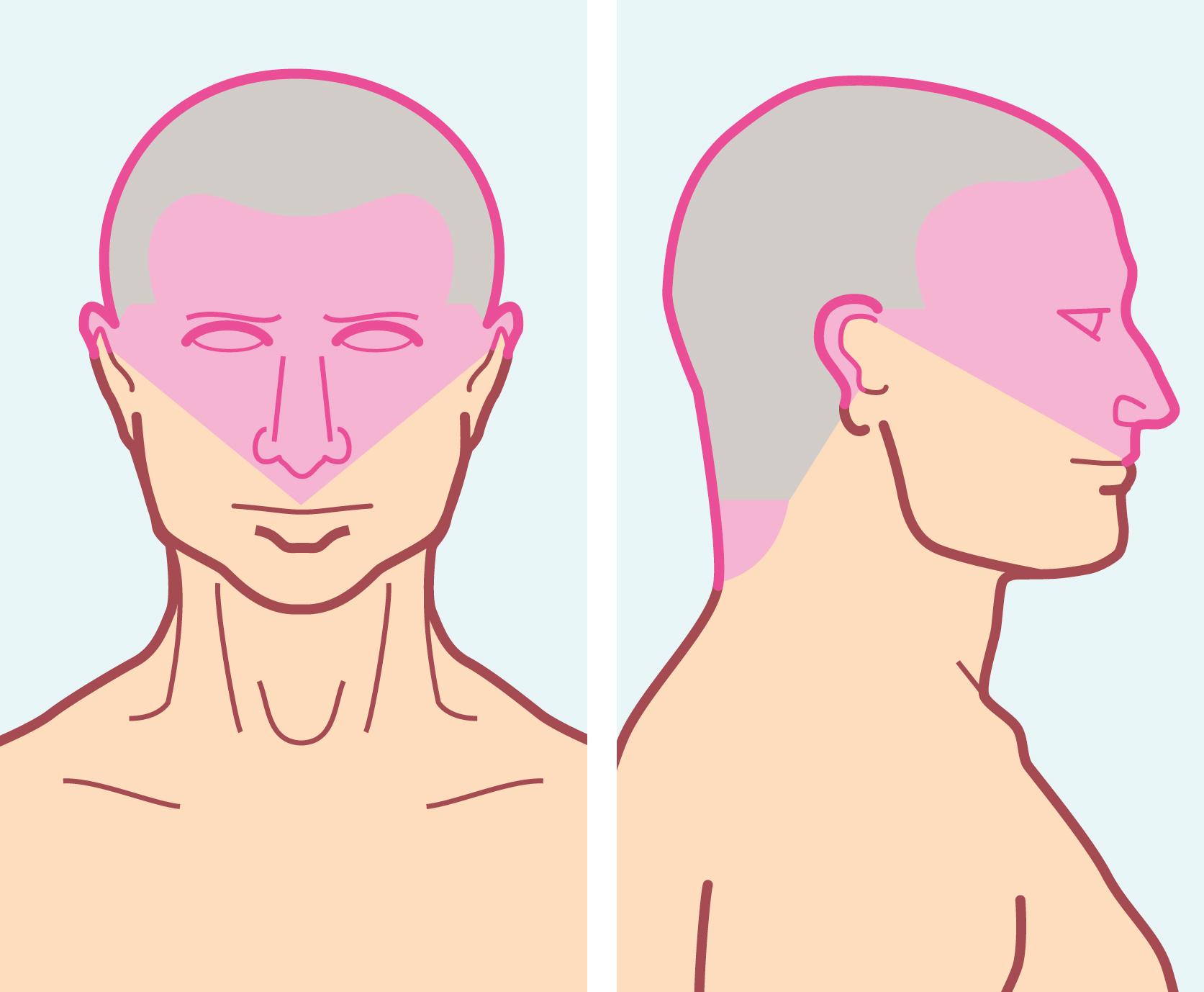
BCCs are slow growing locally invasive malignant epidermal tumours that occur predominantly in sun exposed areas of the head, neck and limbs (80%) and most frequently over the age of 40 years (85%). Most BCCs arise on the upper part of the face ( Fig. 46.8 ), although any area of skin can be involved. Most patients present early because lesions are so visible. In immunosuppressed patients, there is a greater risk of multiple BCCs and recurrences.
BCCs can be broadly categorised into low-risk (e.g., nodular, superficial) and high-risk (e.g., morpheic [ill defined and spreading laterally], infiltrative) although 26 histopathological types have been described. Lesions commonly present as pearly-white nodules with a rolled edge and a central ulceration or crust, often with arborising blood vessels. Although they are surface lesions, they have the potential to erode into underlying tissues, such as cartilage and bone if neglected ( Fig. 46.9 ). A very small percentage of BCCs metastasise, although this is rare. Histologically, the central tumour cells have basophilic nuclei and small amounts of cytoplasm, whilst the peripheral cells are arranged in a palisade pattern reminiscent of normal basal cells.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here