Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Wrist injuries are common, and proper management relies on an understanding of normal anatomy, alignment, and kinematics.
Scaphoid fractures can be subtle, and due to the precarious blood supply to this bone, may go on to non-union if not properly managed.
Indications for scapholunate ligament repair and/or reconstruction depend on the patient's symptoms and on the chronicity of the injury.
For distal radius fractures requiring stabilization, external fixation and dorsal plating have largely been supplanted by volar fixed-angle locking plates, which provide the necessary stability for fracture healing, even in osteoporotic individuals.
Ulnar styloid fractures only require fixation in the setting of distal radioulnar joint instability.
Access video content for this chapter online at Elsevier eBooks+ ![]()
The wrist is a complex articulation that connects the hand to the forearm. Entire textbooks have been devoted to detailed discussions of the anatomy, physiology, and pathology of this important joint. This chapter will review some of the more common injury patterns seen in the wrist, including fractures of the carpal bones, ligamentous injuries of the wrist, and fractures of the distal radius and ulna.
The epidemiology of wrist fractures has been investigated in detail. Each year, nearly 1.5 million hand and wrist fractures are estimated to occur in the United States, accounting for 1.5% of all emergency department visits. Of these, approximately 208,000 are carpal fractures.
The scaphoid is the carpal bone most commonly fractured; it accounts for 60–80% of all carpal fractures. Incidence estimates range from 2.9/10,000 person-years in the United Kingdom to 12.1/10,000 person-years in the US military population. The highest incidence is found in the 20–24-year-old age group, and there is a clear male predominance.
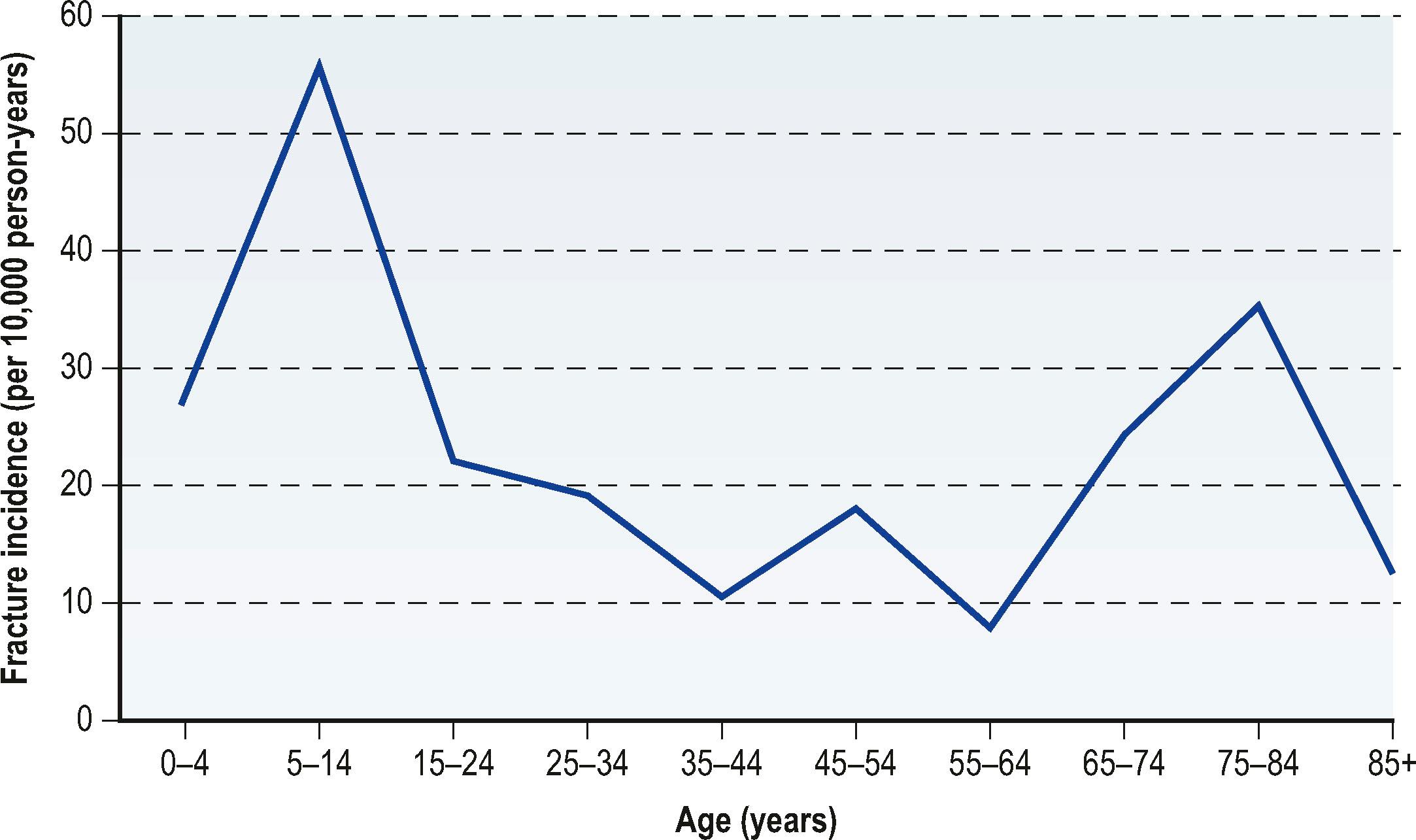
Distal radius fractures are the most common upper extremity fracture; the annual incidence is estimated at 643,000 fractures per year in the United States. When the incidence is examined by age, there are two distinct peaks identified ( Fig. 8.1 ), representing the 5–14-year-old group (55.7/10,000 person-years) and the 75–84-year-old group (35.2/10,000 person-years).
Although a common injury, these fractures should never be treated casually. There is significant potential for patient disability if these injuries are not managed with great care and expertise. Khan and Giddins' review of hand and wrist surgery negligence claims in the UK from 1995–2001 revealed that wrist fracture was the most common condition in which negligence was alleged, comprising 48% of claims.
The carpus was not well described until the 1500 s, when Andreas Vesalius first identified the eight carpal bones. Before then, drawings of the hand connected the metacarpals directly to the distal radius, with no mention of wrist anatomy. Carpal bones are generally named for their shapes. For example, the scaphoid resembles a boat, whereas the lunate resembles the crescent moon. The names of the carpal bones were not solidified until 1955 when Nomina Anatomica established the official nomenclature for the carpal bones that we use today ( Fig. 8.2 ).
Historically, the carpal bones have been grouped together in various ways, based on function and kinematics. The earliest classification separates the wrist joint into two rows, consisting of the distal carpal row (trapezium, trapezoid, capitate, hamate) and the proximal carpal row (scaphoid, lunate, triquetrum). The carpus can also be divided into columns: a radial column (scaphoid, trapezoid, trapezium), a central column (lunate, capitate), and an ulnar column (triquetrum, hamate). The pisiform bone is not involved in wrist motion, so it is not typically included in these groupings.
Abraham Colles (1773–1843) is credited with the first clinical description of fractures of the distal radius. His 1814 manuscript provides an eloquent description of closed reduction and splinting, in an era before the development of radiographs, anesthesia, and plaster-of-Paris. On the results of treatment, he proclaimed, “The cases treated on this plan have all recovered without the smallest defect or deformity of the limb, in the ordinary time for the cure of fractures.”
More than 200 years later, closed reduction and immobilization is still the predominant method of treatment for distal radius fractures, though internal fixation has been steadily gaining in popularity. It is now commonly believed that restoration of anatomic alignment of the distal radius leads to better outcomes, although the age and activity level of the patient certainly contribute to this equation. To achieve these ends, technology has advanced to allow for precise fracture fixation with a variety of techniques. Over the past several decades, pins-and-plaster and external fixation systems have largely given way to internal fixation methods, heavily encouraged by AO (Arbeitsgemeinschaft für Osteosynthesefragen). AO is a Swiss organization started in the late 1950s for promoting more consistent fracture care, chiefly using rigid internal fixation. Despite the development of hundreds of fixators, plates, rods, and other devices, there is little high-level evidence to support the use of one technique over another. In some ways, Colles' conservative approach was probably correct – many patients, especially the low-demand elderly population, achieve excellent outcomes even in the presence of significant malunion or malalignment.
Many textbooks discourage the use of eponyms, believing them to be of historical interest only. However, the various eponyms for distal radius fractures often convey precise information regarding the fracture pattern and the type of injury sustained. The major eponyms for distal radius fractures are: Colles fracture (extra-articular fracture with dorsal displacement of distal fragment) ( Fig. 8.3A ); Smith fracture (also called reverse Colles fracture; extra-articular with volar displacement of distal fragment) ( Fig. 8.3B ); Barton fracture (intra-articular shear fracture of the radiocarpal joint, may be dorsal or volar) ( Fig. 8.3C,D ); and Chauffeur fracture (intra-articular fracture involving the radial styloid) ( Fig. 8.3E ). For some cases, these eponyms may help in selecting a treatment modality.
Normal anatomy of the wrist is covered in detail in Chapter 1 of this volume. However, there are a few points that merit emphasis in this chapter with regard to these injuries.
The vascularity of the scaphoid bone bears particular consideration. The scaphoid bone has a single dominant vascular pedicle that enters from the distal pole of the bone. Therefore, the proximal pole relies wholly on the intramedullary blood supply for survival. It is for this reason that proximal pole fractures typically take longer to heal and have increased incidence of non-union. Furthermore, in cases of non-union, the proximal pole is susceptible to avascular necrosis, which further complicates these injuries.
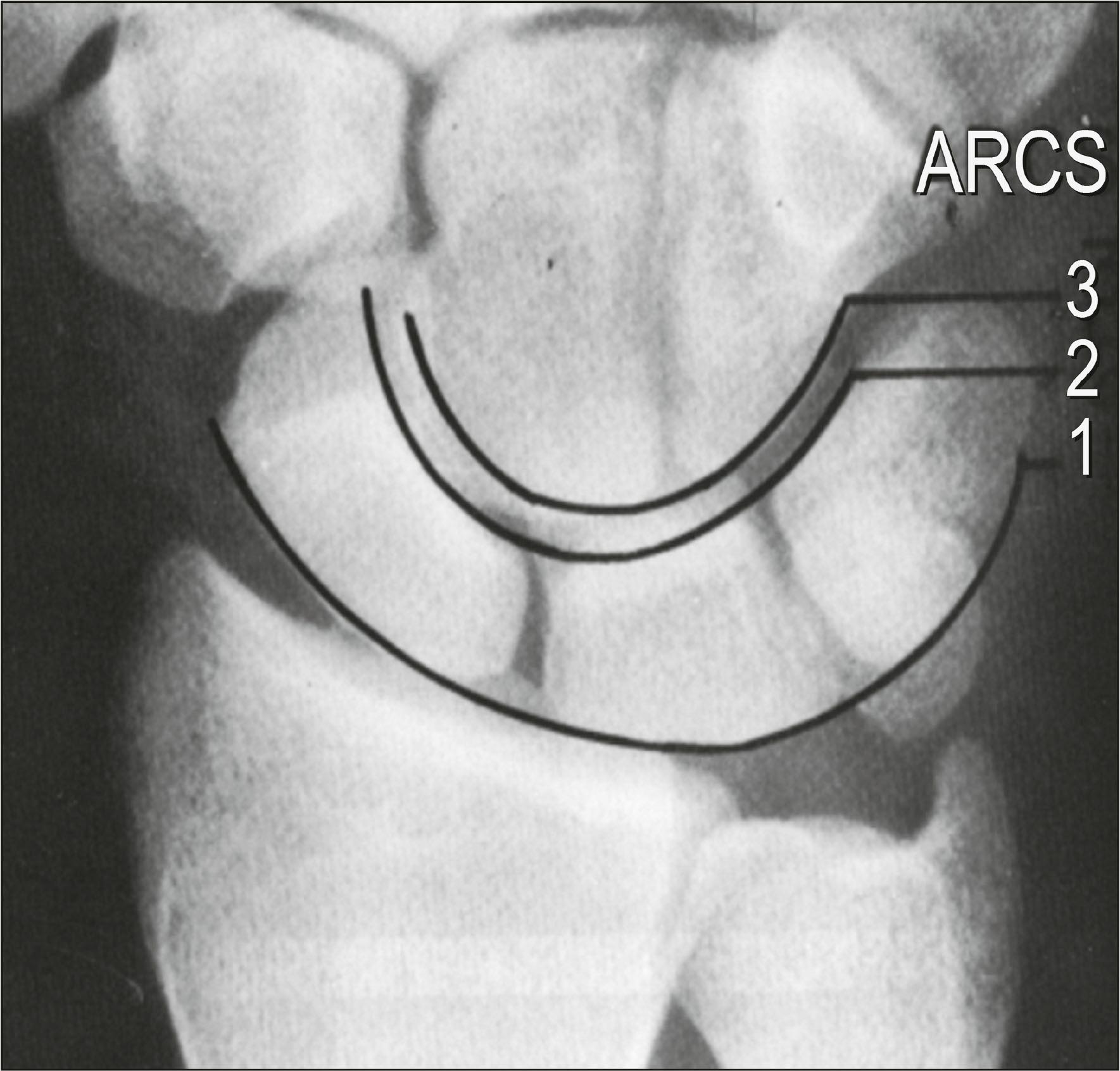
Detection of ligamentous injuries of the wrist is made easier by attention to the Gilula arcs ( Fig. 8.4 ). Dr. Gilula, a radiologist, described three arcs that can be noted on the posteroanterior radiograph of the wrist, formed by the proximal and distal articular surfaces of the proximal row, and the proximal articular surface of the distal row. Increased joint space or deviation of carpal bones from these lines is indicative of wrist instability.
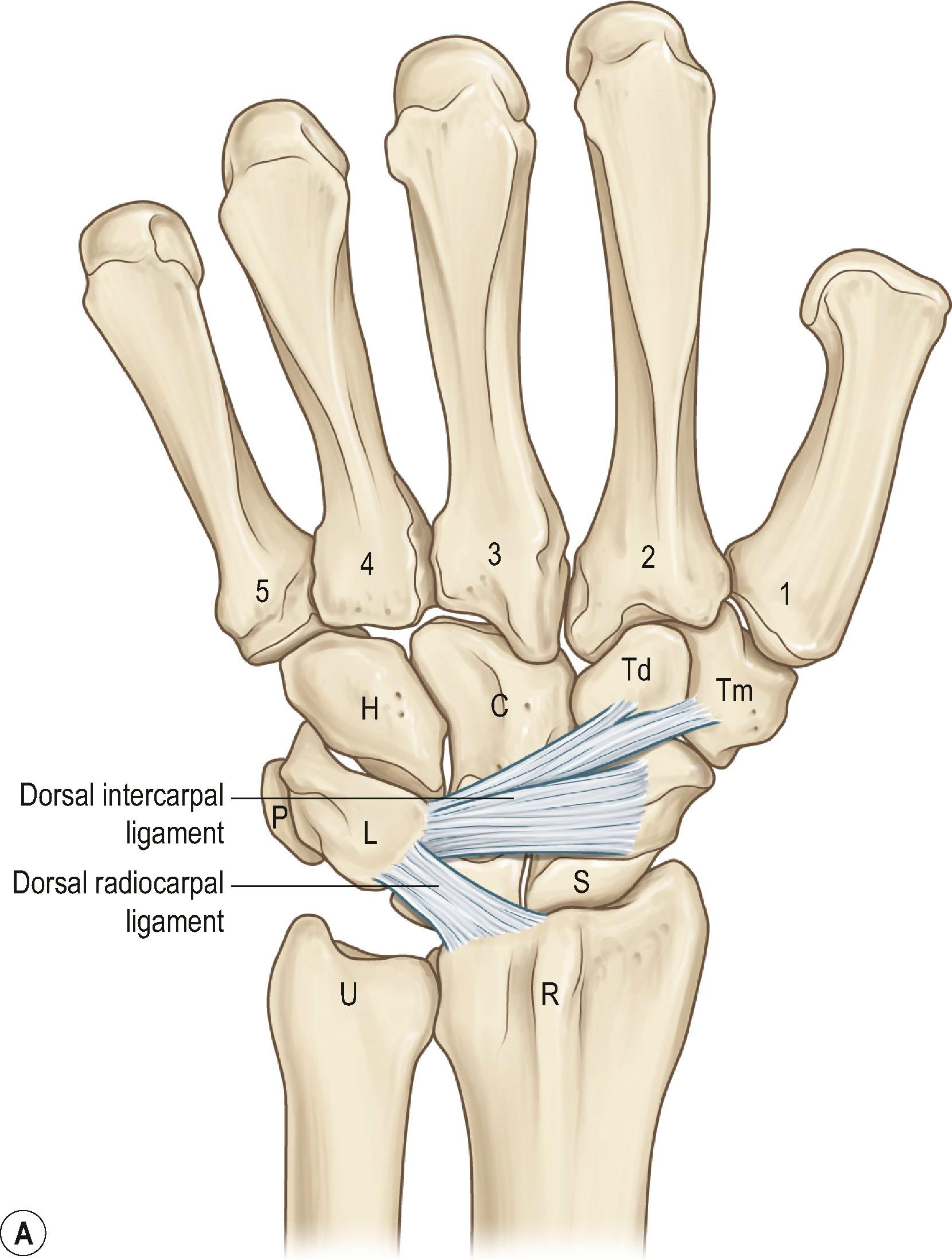
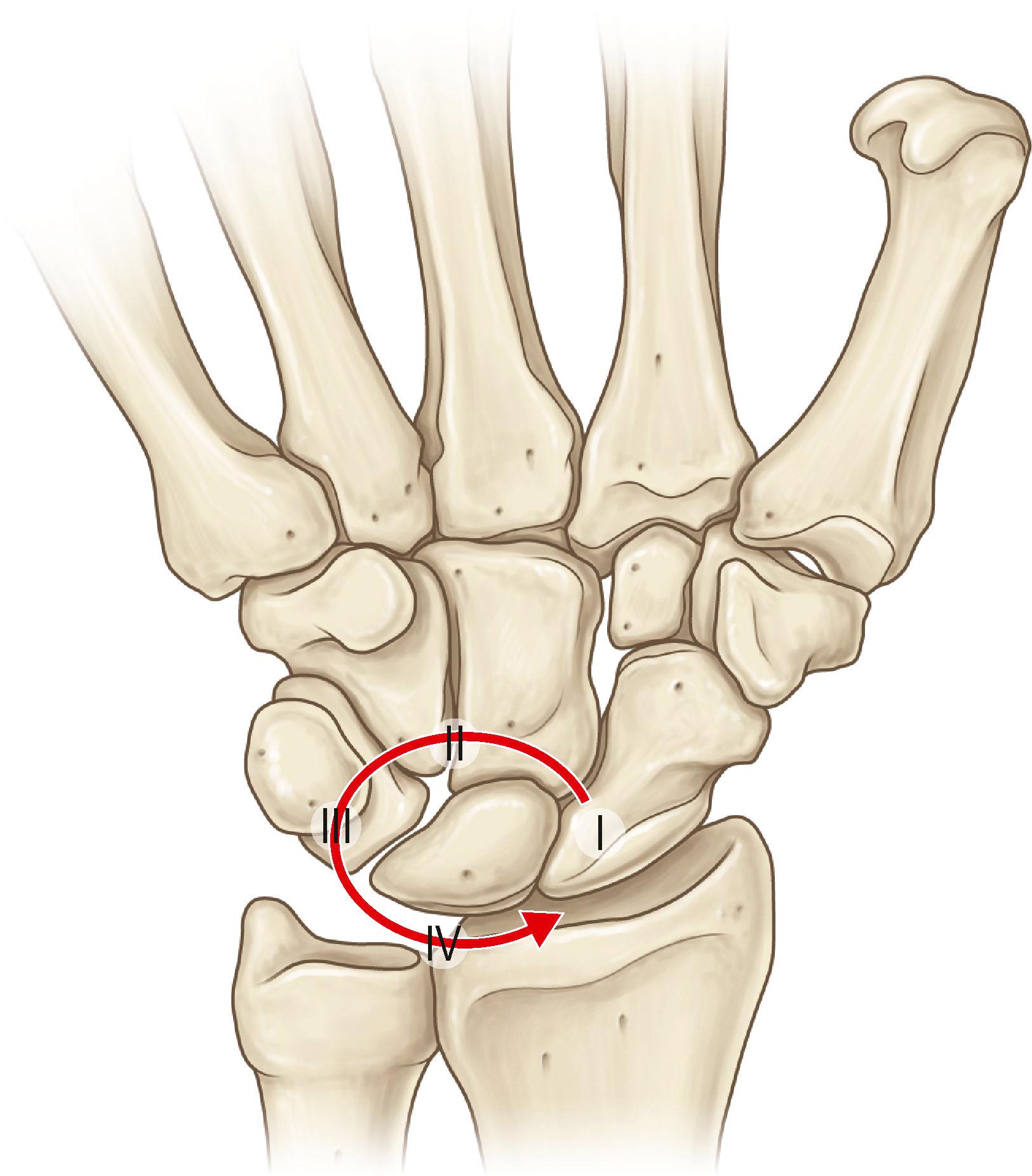
The bones of the wrist are linked by a complex system of intrinsic and extrinsic ligaments ( Fig. 8.5 ). The strength of these wrist ligaments helps determine the injury patterns observed. For example, the very strong short radiolunate ligament tends to resist lunate dislocation, retaining the lunate in its fossa on the distal radius in all but the most severe traumas. Instead, the surrounding carpal bones typically dislocate away from the lunate. This perilunate pattern of injury has been described in stages by Mayfield ( Fig. 8.6 ): (I) rupture of the scapholunate interosseous ligament; (II) capsular disruption through the space of Poirier, an area of inherent weakness of the volar capsule between the lunate and capitate; and (III) rupture of the lunotriquetral interosseous ligament. If the dislocated carpus rebounds, then the capitate will settle into the lunate fossa, and the lunate rotates volarly (IV), hinged on the short radiolunate ligament ( Fig. 8.7 ).

Injury patterns are also influenced by the details of bony anatomy and structure. For example, both the diaphysis and the articular surface of the distal radius have thicker cortical bone than is found at the metaphysis. The thinner cortical bone at the metaphysis is what makes it vulnerable to fracture, especially in the osteoporotic population. Furthermore, within the metaphysis, there is a distinct difference between the dorsal and volar cortices. The dorsal cortex is much thinner, resulting in extensive comminution in most cases of distal radius fracture from falls on outstretched hands, where the force is directed in a volar-to-dorsal direction.
The extensor pollicis longus (EPL) is the tendon most likely to rupture after a distal radius fracture. Of note, rupture is more common with non-displaced fractures, and has been reported in cases of wrist injury without fracture. The etiology of this appears to be related to interruption of the tendon's nutritional supply, leading to attritional rupture. This most commonly occurs at the Lister tubercle, where there is a natural watershed area of this tendon's intrinsic blood supply. If the extrinsic (diffusion-mediated) nutritional supply is also interrupted by fracture callus, fracture displacement, or swelling from edema or hematoma, rupture of the EPL can occur.
The biomechanics of the hand and wrist were reviewed in Chapter 1 , but there are a few points to revisit here.
Disruption of the normal linkages between the bones of the wrist – whether due to ligamentous rupture or fracture – can lead to carpal instability. The concept of carpal instability has evolved rapidly over the past 50 years as we have learned more about the ways in which the wrist bones move (kinematics) and transfer a load (kinetics). Specifically, a wrist is unstable if it is unable to transfer functional loads without sudden changes in stress on the articular cartilage, and if it is unable to maintain motion throughout its range without sudden alterations of intercarpal alignment.
Carpal instability has been thoughtfully classified into four major patterns ( Table 8.1 ). Carpal instability dissociative (CID) occurs when there is a disruption within or between the bones of the same carpal row. Carpal instability non-dissociative (CIND) refers to a disruption between the distal radius and the proximal carpal row, or between the proximal and distal carpal rows. When a combination of elements of both CID and CIND exist, it is referred to as carpal instability complex (CIC). Finally, when the instability is an adaptive response to a problem proximal or distal to the wrist itself, it is called carpal instability adaptive (CIA).
| Pattern | Definition | Example(s) |
|---|---|---|
| Carpal instability dissociative (CID) | Disruption within or between bones of the same carpal row | Scapholunate dissociation; scaphoid non-union |
| Carpal instability non-dissociative (CIND) | Disruption at the radiocarpal or midcarpal joints, with intact proximal and distal rows | Midcarpal instability |
| Carpal instability complex (CIC) | Derangement both within and between carpal rows (CID plus CIND) | Perilunate dislocation with ulnar translation |
| Carpal instability adaptive (CIA) | Instability due to injury proximal or distal to wrist | Distal radius malunion |
Carpal kinematics has perhaps the biggest clinical impact on scaphoid fractures and scapholunate ligament injuries. The proximal carpal row is “pre-tensioned”, with the scaphoid subject to a flexion moment, and the triquetrum tending to follow an extension moment. Any breakage of the connections within this row, whether intracarpal (e.g., scaphoid fracture) or intercarpal (e.g., scapholunate ligament rupture), will result in carpal instability because the disconnected carpal bones rotate in opposite directions. This natural tendency for the components in this row to fall away from each other is in part responsible for the high rate of complications after these types of injury.
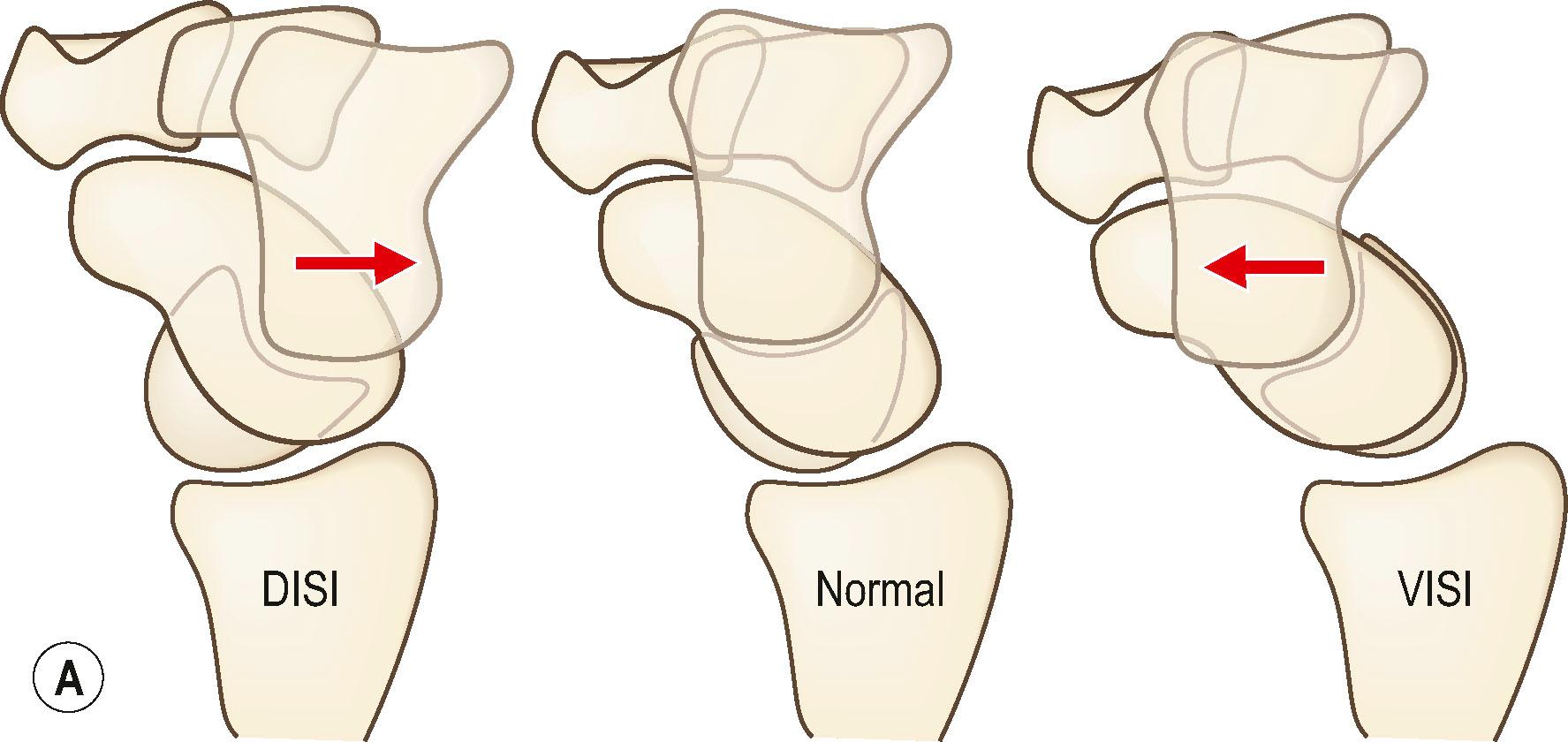
Two particular instability patterns that result from CID within the proximal row are dorsal intercalated segment instability (DISI) and volar intercalated segment instability (VISI) ( Fig. 8.8 ). DISI deformity is commonly associated with scapholunate ligament disruption or displaced scaphoid fractures, whereas VISI deformity is associated with lunotriquetral ligament disruption.
Because of the scaphoid's natural tendency to flex when loaded, delayed treatment of comminuted fractures of the scaphoid waist tend to result in the so-called “humpback deformity” ( Fig. 8.9 ). This term describes the shape of the scaphoid as seen on lateral tomograms, reflecting malunion of the bone with an abnormally acute angle between the proximal and distal poles of the scaphoid.

In elderly osteoporotic patients, wrist injuries are commonly seen after falls from a standing height (fragility fractures). Very often, this is an extra-articular fracture with apex volar angulation, the so-called “Colles fracture” (see Fig. 8.3 ). Patients sustaining one fragility fracture are at risk for future fragility fractures. This population should have appropriate screening, diagnosis, and treatment of underlying osteopenia or osteoporosis.
The younger population typically experiences fractures caused by higher energy injuries, such as motor vehicle collisions or sports-related trauma, resulting in more complex fracture patterns. With increasing force of injury, the chance of associated carpal fracture, intercarpal ligament injury, and/or triangular fibrocartilage complex injury increases.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here