Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The many specialized structures of the hand and upper extremity work in intimate synchrony to provide a harmonious interplay of precision motor biomechanics with fine tactile senses. Our hands are subject to many common occupational and domestic injuries, including fingertip trauma, tendon lacerations, neurovascular compromise, fractures, and soft tissue loss. Every extremity trauma has its own unique characteristics that offer challenges for soft tissue coverage. Although the principles of the reconstructive ladder apply, this chapter focuses on soft tissue reconstruction of the upper extremity using local, regional, and free flaps only.
All trauma surgeries start with patient stabilization, wound irrigation and debridement, repair and reconstruction of the skeleton and soft tissues, and culminates with definitive closure. The closure decision should incorporate the goals and priorities of reconstruction. Each area of the upper extremity has its own set of unique soft tissue needs that allow that area to function at an optimum level. Soft tissue reconstruction of the upper extremity could be divided up into six main areas ( Box 20.1 ). A final category would add catastrophic injuries such as the mangled or mutilated upper extremity where the zone of injury transcends many of the six zones in the limb.
Fingertips
Digits
Hand
Forearm
Elbow/antecubital fossa
Upper arm
While the goals include life preservation, limb preservation, function preservation, and then functional reconstruction, the priorities of function, contour, and stability, as well as the anticipation of further reconstructive surgery is very important in choosing the flap of choice. Currently used flaps include fasciocutaneous, fascial, musculocutaneous, muscle, and osteocutaneous flaps. Flap selection is based on the characteristics of the defect, including size, shape, and location, the availability of donor sites, and the goals of reconstruction.
Finger reconstruction with flaps traditionally uses adjacent tissue on the finger, tissue from the proximal digit, the adjacent digits, the dorsal or palmar hand, or from distant tissue such as the abdomen or toe pulp. The fingertip is an area where local flaps is commonly used for reconstruction. Box 20.2 illustrates the variety of flaps available for closure of the fingertip injuries.
Volar V-Y
Lateral V-Y
Cross finger
Thenar crease
Moberg volar advancement
Homodigital
Heterodigital
Reverse dorsal metacarpal artery
Thoraco-epigastric
Free toe pulp/nail bed
This flap is used for distal fingertip defects oriented in a dorsal oblique or transverse fashion, measuring <1 cm, usually with exposed bone. The volar triangular flap is oriented with the apex at the distal interphalangeal crease ( Fig. 20.1 ). The skin is incised full thickness. Blunt dissection with spreading of the tissue in the direction of vascular inflow into the flap is performed until the tissue advances to cover the defect. The donor site is sutured to provide a V-Y, tension free closure ( Fig. 20.2 ). Flap length is 1.5–2 times the width, and width is limited to that of the nail bed to prevent tip flattening. This flap provides durable, glabrous, sensate skin for coverage. The flap is limited to cover smaller defects usually <1.5 cm in size. Potential complications include cold intolerance, scarring, and sensory changes.


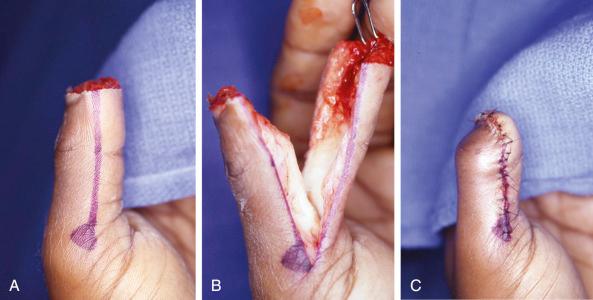
Transverse and dorsal oblique defects of the fingertip can occasionally be closed with a laterally based V-Y advancement with the apex at the DIP joint ( Fig. 20.3 ). It is oriented to be at least 2–3 mm from the nail folds dorsally, with a more thorough dorsal dissection to release the fibrous septae, while preserving the more volar neurovascular contributions. This again provides vascularized, sensate coverage but is severely limited in advancement to about 0.5–0.75 cm.

This flap is most often used for the thumb. Radial and ulnar midaxial incisions are made on either side of the thumb. The flap is elevated in the plane above the tendon sheath incorporating both the neurovascular bundles in the fasciocutaneous flap. The Moberg flap offers up to 2 cm of advancement to cover distal thumb defects. Occasionally the interphalangeal joint needs to be flexed to allow the flap to be inset into the remaining nailbed. The interphalangeal joint extends over time, stretching the flap as it does so. The Moberg advancement flap provides well-vascularized, glabrous, sensate coverage ( Fig. 20.4 ). There has been a number of modifications of the Moberg that are employed to provide a little more length to the advancement. The flap can be advanced as a V-Y flap where the apex is at the volar, proximal thumb crease. Alternatively, a transverse incision can be made in the skin at the proximal thumb, the tissue spread to release the tension from the more proximal palmar skin. A skin graft is then used to close to proximal donor defect as the flap advances distally. The Moberg, volar advancement flap as described is not typically used for other digits of the hand as it may cause flexion contractures of the finger.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here