Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Medial maxillectomy is a procedure historically used for the removal of benign and low-grade malignant tumors of the medial aspect of the maxilla, lateral nasal wall, ethmoid sinuses along the lamina papyracea, and the lacrimal sac.
The endoscopic approach allows superior illumination and magnification as well as the ability to treat diseases that extend beyond the limits of the traditional external medial maxillectomy.
The endoscopic medial maxillectomy (EMM) procedure extends maxillary antrostomy (i.e., mega-antrostomy) that is typically performed in endoscopic sinus surgery for chronic rhinosinusitis.
Indications for EMM are comparable to those indicated for a conventional medial maxillectomy: sinonasal neoplasms, inverted papilloma, and intractable inflammatory maxillary disease.
The maxillary sinus usually consists of a single pyramidal chamber with an adult volume of approximately 15 mm.
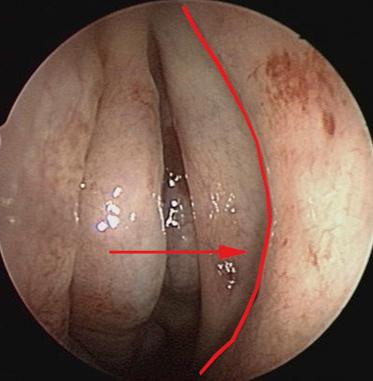
The medial maxillary wall contains the natural ostium of the maxillary sinus and includes the uncinate process (mucosa and bone), posterior fontanelle (mucosa only), the inferior turbinate, the perpendicular plate of the palatine bone, and the lacrimal bone. The natural ostium of the maxillary sinus is located along the inferior 1⁄3 of the medial maxillary line ( Fig. 21.1 ).
The uncinate process is a thin, sagittally oriented sickle-shaped bone that forms the medial boundary of the infundibulum, which is a functional space into which the maxillary sinus and anterior ethmoid sinuses drain.
The lateral apex of the sinus extends into the zygomatic process of the maxillary bone. The roof of the maxillary sinus is formed by the bony orbital floor, and the floor is formed by the alveolar and palatine processes of the maxilla.
The inferior turbinate arises from the medial maxillary bone as the maxilloturbinal.
The distal opening of the lacrimal apparatus is the Hasner valve, located in the inferior meatus, 30 to 35 mm posterior to the limen nasi.
An endoscopic medial maxillectomy is performed with hypotensive anesthesia, as it has been shown to improve the intraoperative field. The use of total intravenous anesthesia (TIVA) has been shown to reduce intraoperative blood loss in a number of studies.
Preoperatively, the nose is decongested topically with 0.05% oxymetazoline or 4% topical cocaine or 1:1000 epinephrine prior to endoscopy. The mucosa of the inferior turbinate and lateral nasal wall is infiltrated with 1% lidocaine with 1:100,000 epinephrine, which can reduce the amount of bleeding during resection.
A transoral pterygopalatine injection can be performed by inserting a 25-gauge needle bent at 2.5 cm into the greater palatine foramen, opposite the second molar to provide additional vascular control. Alternatively, sphenopalatine injection can be performed by inserting a 25-gauge spinal needle bent at 1 cm inferior to the junction of the middle turbinate and lateral wall in the mucosa overlying the crista ethmoidalis. Care must be taken to avoid an intravascular injection of this local anesthetic.
A septoplasty may be performed if a septal deflection is preventing access to the middle meatus. However, consideration must be given to the potential need for a septal window, which can be used to access the lateral and anterior portions of the maxillary sinus.
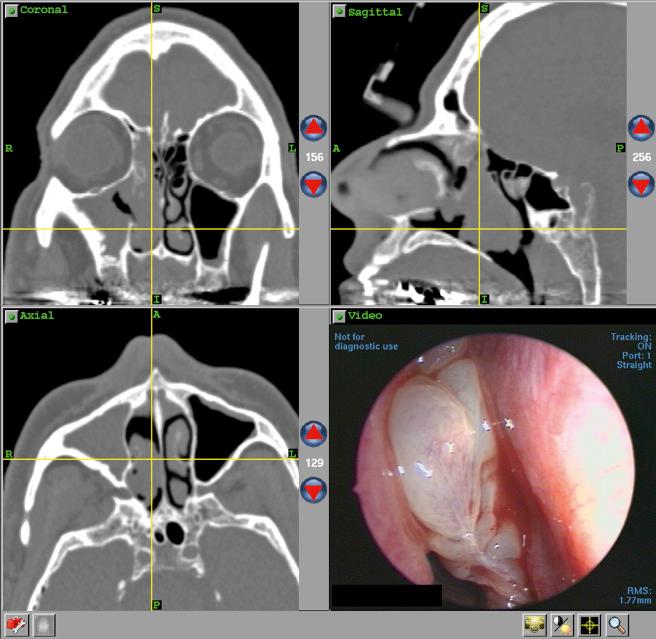
All patients should undergo computed tomography (CT) imaging. In patients with inverted papilloma, this is very helpful in determining the site of attachment since hyperostosis ( Fig. 21.2 ) has been reported to be associated with the origin of the tumor. The CT scan should also be examined for any focal bony erosion, as this is concerning for malignant transformation of the tumor. All boundaries of the sinus must be inspected for tumor.

Magnetic resonance imaging (MRI) helps the surgeon distinguish tumor from inspissated secretions or polypoid mucoperiosteal thickening and reveals the status of extranasal tissue when sinus bone is eroded.
CT showed the highest sensitivity for the site of attachment of inverted papillomas, while MRI showed greater specificity. Preoperative CT plus MRI may provide more useful information than CT or MRI alone if the site of surgical attachment may change the planned operative approach.
Stereotactic image guidance can be helpful to ensure that all regions of the maxillary sinus are addressed ( Fig. 21.3 ).
Meticulous preoperative analysis of CT and MRI scans and individual anatomy is essential for adequate surgery.
The endoscopic technique can maintain key oncologic principles by performing complete resection of the tumor pedicle and allowing adequate margin control with the use of frozen sections intraoperatively.
Preserving a nasal floor mucosal flap aids in covering exposed bone after the case.
Multiple expanded endoscopic techniques exist to reach the anterolateral aspects of the maxillary sinus, including the transseptal, inferior meatal window approach, endoscopic canine fossa puncture, endoscopic anterior maxillotomy, and the endoscopic Denker approach.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here