Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
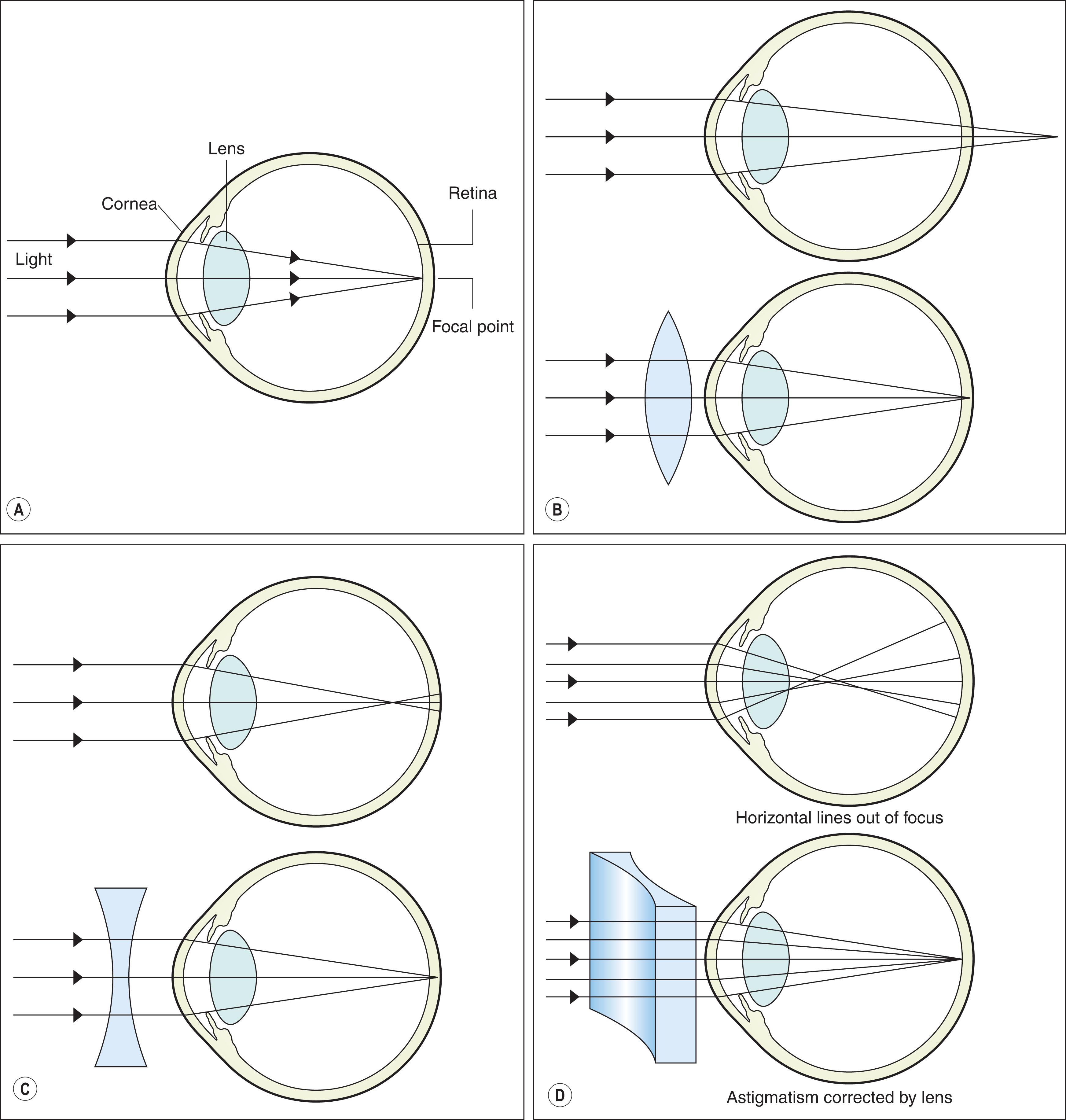
Refractive errors cause blurred vision and potentially amblyopia through inability to form a perfectly focused image on the retina. Emmetropia is the state of a perfectly focused eye when the power of the cornea and lens are exactly appropriate for the axial length of the eye ( Fig. 6.1 ); this is uncommon in young children because their eyes have not completely matured, and a mild hyperopic refractive error is frequently present. Not all refractive errors require treatment. This chapter reviews the current state of diagnosis, treatment, and prevention/control of refractive errors in children.
In children, cycloplegia is required to measure refractive error accurately because accommodation is active, causing overestimation of myopia and underestimation of hyperopia. Phenylephrine 2.5% is often added to cycloplegic agents to enhance dilation. Toxicity from cycloplegic agents is uncommon. Signs and symptoms of anticholinergic effects include flushing, fever, rash, rapid or irregular heartbeat, dry mouth, and mental status changes. These should be reported immediately. Cycloplegic agents include atropine 1%, cyclopentolate 0.5%, 1% or 2%, and tropicamide 0.5% or 1%. Atropine provides the most complete cycloplegia, but has the longest time to onset, duration of effect, and the most severe side-effect profile. Tropicamide has the shortest onset and is better tolerated because of its shorter duration of action and low side-effect profile, but residual accommodation remains. Cyclopentolate 0.2% combined with phenylephrine 1% is available in the United States as Cyclomydril™. It is primarily used for pupillary dilation of premature infants. Table 6.1 outlines the cycloplegic agents employed in the authors' practice based on age.
| Age | Recommended agent | Dosage | Onset of cycloplegia | Duration of cycloplegia + mydriasis | Side effect profile |
|---|---|---|---|---|---|
| Preterm to 3 months | Cyclomydril (cyclopentolate 0.2% and phenylephrine 1%) | Two sets of one drop every 5 minutes | 20–60 minutes | 6–48+ hours | Minimal |
| 3 months to 1 year | Cyclopentolate 0.5% | Two sets of one drop every 5 minutes | 20–60 minutes | 6–48+ hours | Moderate |
| 1 to 12 years | Cyclopentolate 1% or | Two sets of one drop every 5 minutes | 20–60 minutes | 6–48+ hours | Moderate |
| Atropine 1% drops or ointment | One drop twice a day for 3 days | Hours | 1–2+ weeks | High | |
| 12 years and older | Tropicamide 1% | Two sets of one drop every 5 minutes | 25–40 minutes | 2–6+ hours | Low |
Useful techniques for measuring refractive errors in children include cycloplegic retinoscopy, autorefraction, and post-cycloplegic subjective refraction. Ocular biometry and corneal topography are useful adjunctive measures in selected children.
Cycloplegic retinoscopy is useful in very young and developmentally delayed children. Cycloplegic retinoscopy is also useful to confirm findings of autorefraction. In addition, cycloplegic retinoscopy performed over existing glasses or contact lenses can be a rapid way to determine whether there has been a significant change in the prescription, or whether media irregularities are present that may preclude successful neutralization of refractive error with spectacles. A description of the technique is beyond the scope of this chapter but is published elsewhere.
Dynamic retinoscopy can help to confirm accommodative dysfunction, which is sometimes present in children with cerebral palsy, Down syndrome, and other neurodevelopmental concerns. To perform dynamic retinoscopy, the authors use the monocular estimate method (MEM). The patient fixates on a detailed target held in the plane of the retinoscope. Testing is performed with the spectacle correction in place. Room lights are dim, but bright enough for the child to be able to see the target. The examiner should use a working distance of about 40 cm. If the patient is accommodating appropriately, the retinoscopy reflex should be neutral when the child fixates on the target. If a “with” reflex is present, there is a “lag” in accommodation, and if an “against” reflex is present, there is a “lead” in accommodation. A small lag in accommodation is acceptable (1 diopter or less), but children who have larger amounts of accommodative lag can benefit from correction of hyperopia and possibly even reading glasses or bifocals. Occasionally, infants will present with a delay in development that is due to moderate-to-high hyperopia and poor accommodation. Dynamic retinoscopy is invaluable in identifying this disorder ( Fig. 6.2 ).

The authors have found in their practice that autorefraction performed monocularly and with cycloplegia using late model stationary and hand-held devices provides very accurate measurements of refractive errors and can be used in cooperative children and even some infants ( Fig. 6.3 ). Autorefraction may more accurately detect astigmatism than retinoscopy. Nevertheless, we recommend confirming autorefraction findings with retinoscopy and visual acuity measurements, when possible, rather than prescribing spectacles based on autorefraction alone.

Post-cycloplegic subjective refraction can be useful in children. Often, a prescription can be written for the full refractive error detected with cycloplegic refraction, but sometimes it can be helpful to have the patient return to the office for subjective refraction after the cycloplegic agent has worn off. Examples include children with high hyperopia who do not tolerate the full plus correction, children who have significant changes in refractive error over relatively short periods of time, children with incomplete cycloplegia at the time of retinoscopy, and children with irregular red reflexes that limit the ability to perform retinoscopy or autorefraction.
Corneal topography can be a useful diagnostic tool in children with significant corneal astigmatism to confirm the axis of astigmatism, to diagnose irregular or asymmetric astigmatism and early keratoconus, and to identify lenticular astigmatism. It can also help with contact lens fitting.
A-scan ultrasound or non-contact optical biometry measurement of axial length, anterior chamber depth, and lens thickness can be useful to determine the etiology of refractive errors, and is invaluable in determining intraocular lens power for cataract surgery, but is not used routinely to diagnose refractive errors. Ocular biometry will likely take on an important role in evidence-based myopia control as these practices evolve.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here