Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Mucous membrane pemphigoid (MMP) is a blinding, systemic autoimmune disease characterized by autoantibodies deposited along the basement membrane zone of mucous membranes and skin.
Ocular involvement occurs in approximately 80% of patients with MMP.
Clinical course is characterized by slow progression from chronic conjunctivitis to subepithelial fibrosis, fornix foreshortening, symblepharon, and ankyloblepharon formation with ocular surface keratinization.
The gold standard for diagnosis of MMP is a conjunctival biopsy using immunofluorescent or immunoperoxidase techniques.
Early diagnosis and management is crucial to optimize long-term vision.
No topical medications have been shown to be effective in controlling disease activity in ocular MMP, and therefore systemic therapy is necessary to prevent blindness.
The goal of pharmacotherapy is to reduce morbidity and to prevent complications. Combination therapy in a stepladder regimen is needed in many cases to improve disease control.
Mucous membrane pemphigoid (MMP) is an autoimmune chronic cicatrizing disease characterized by autoantibodies deposited along the basement membrane zone (BMZ) at the epithelial–subepithelial junction of mucous membranes and occasionally skin.
The disease causes subepithelial scarring of the mucosal surfaces, hence its previous and still used name of cicatricial pemphigoid (CP).
The rate of ocular involvement varies in ophthalmic and oral literature and ranges from 30% to 80% depending on the source. Ocular MMP, also known as ocular cicatricial pemphigoid (OCP), primarily affects the conjunctiva (and the mucosae, including oral, nasal, and esophageal, in lesser frequency), with the β4 subunit of α6β4 integrin the target of attack.
The clinical course of ocular MMP is characterized by slow progression from chronic conjunctivitis to subepithelial fibrosis, fornix foreshortening, symblepharon, and ankyloblepharon formation with ocular surface keratinization. Such processes typically last for several years and can ultimately lead to blindness without treatment.
The average age at onset of MMP is 65 years. However, this figure does not report the true epidemiologic features of this disease, because the reported cases are usually not in their earliest stages. Conjunctival involvement may occur as early as 10 years before other mucosal or skin lesions develop, or it may occur as much as 20 years following the onset of other lesions. The disease may also be limited to the conjunctiva and go undiagnosed for many years.
Wichmann is credited with the first description of MMP involving the conjunctiva, although he interpreted the disease as “pemphigus.” The progressive clinical course leading to end-stage disease in CP was subsequently described by von Graefe in 1878. It was not until 1953 that Lever, a Boston dermatologist, made the clinical and histopathologic distinction between pemphigus and pemphigoid.
Franke published a report in 1900 summarizing the clinical course of 107 patients with CP affecting the conjunctiva. Since that description, many other authors have published their observations, and all agree that the disease is invariably progressive and that the ultimate prognosis is quite poor. Unfortunately, it seems to take each new generation of ophthalmologists some personal experience to appreciate this fact. Because few ophthalmologists have the opportunity to observe significant numbers of patients with this disease over a sustained period, and because the disease does not progress inexorably and continuously but rather in fits and starts, there are still many ophthalmologists who have the mistaken belief that CP affecting the conjunctiva can be treated with drops (steroid, vitamin A, cyclosporine) or with subconjunctival injections (steroid, mitomycin C). It may take the disease 10–30 years or more to reach end stage, with bilateral blindness as the result. However, if one follows patients with MMP on conventional therapy long enough, one will invariably observe the long-term devastating consequences. The progression of the disease, although usually slow, may be punctuated by periods of remission or by periods of explosive exacerbation with rampant progression of conjunctival scarring and associated keratopathy. It is also clear that the more advanced the disease is, the more likely it is to progress significantly within 2 years.
Histologically, the conjunctival lesions show submucosal scarring, chronic inflammation, perivasculitis, and squamous metaplasia of the epithelium, with loss of goblet cells; mast cell participation in the inflammation is surprisingly great.
Tissue-fixed immunoglobulins and complement components are present in the epithelial BMZ in patients with MMP. Indeed, this immunoreactant deposition is the sine qua non for definitive establishment of the diagnosis.
Management, prognosis, and treatment of MMP depend on the extent of the disease. Immunosuppressive therapy is used in an attempt to halt the progression, and various immunosuppressive agents have been used to suppress the inflammatory response; most of them will be reviewed in this chapter.
MMP has been thought to be a rare disorder; however, the reported incidence figures vary and concentrate on patients with more advanced stages of the disease, thus underestimating the true incidence. Most articles quote rates from 1 in 8000 to 1 in 50,000. Lever and Talbott stated frankly that it is impossible to make an accurate estimate from available data; they guessed that the incidence of MMP is somewhere between 1 in 12,000 and 1 in 60,000 ophthalmic patients. However, these figures estimate the incidence of relatively advanced MMP. Diagnosis of this disorder in its early stages is difficult, and most cases are not recognized as MMP until they reach what could be categorized as late-stage disease. There are, therefore, patients with early MMP uncounted in the epidemiologic estimates.
Data on the average age of MMP patients are also somewhat distorted by subtleties of the diagnostic signs. MMP is said in many publications to be a disease of older people, with average age given as 60 or 70 years. Although reports of MMP in children may, in fact, represent cases of localized erythema multiforme, it certainly is now recognized that MMP can begin at least as early as the third decade of life. MMP has a slight but definite preponderance for women at a rate of 2–3:1. No racial or geographic predilection has been reported.
MMP has been classically described as an autoimmune disease with a genetic predisposition and probably a “second hit” environmental requirement to trigger the onset of the disease. It exhibits a type II immune reaction characterized by the deposition of immunoreactants (IgG, IgA, IgM, and/or complement) along the epithelial BMZ. A genetic predisposition was initially implicated with an increase in frequency in the human leukocyte antigen (HLA)-DR4 and HLA-DQw3 alleles among patients with MMP. Subsequently, the true susceptibility gene was felt to be in close linkage disequilibrium with the gene HLA-DQ β1∗0301 . DQ β-chain sequencing studies from patients with the HLA-DQ β1∗0301 gene affected by CP and from their unaffected relatives with the HLA-DQ identical gene HLA-DQ β1∗0301 disclosed that the amino acid sequences of the HLA-DQ β-chains from patient and unaffected relatives were identical. These identical genes suggest, therefore, that it is not the HLA-DQ β1∗0301 gene itself, but rather a different gene, in close linkage disequilibrium with HLA-DQ β1∗0301, that is truly the susceptibility gene.
The second-hit environmental trigger that stimulates the genetically susceptible individual to develop MMP may be microbial, as is suspected for idiopathic MMP, or may be chemical, as in the case of so-called drug-induced MMP or pseudo-MMP, which develops in some individuals exposed to practolol or to a limited variety of ocular medications. Patients with pseudo-MMP carry the same susceptibility gene (HLA-DQ β1∗0301) in addition to another, but the autoantigens in these two forms of OCP are different. Foster and colleagues identified a 205 kilodalton (kDa) protein molecule in the BMZ of conjunctiva and epidermis as a relevant target antigen in idiopathic MMP. This target autoantigen is the β4 peptide of α6β4 integrin. Further, the autoantibodies in the sera of patients with MMP directed against this autoantigen are directed (predominantly) against epitopes within the large cytoplasmic domain of the β4 peptide. Additionally, these autoantibodies produce lesions in conjunctiva in an in vitro organ culture system, indicating their very likely pathogenic role in MMP. Sera from patients with pseudo-MMP bind to 97 and 290 kDa proteins in conjunctiva and epidermis lysates, and to 45, 150, 290, and 400 kDa proteins in dermal lysates. None of these autoantigen protein targets is absorbed from the tissue lysates by sera from patients with bullous pemphigoid, pemphigus vulgaris, or MMP, indicating that the autoantigens in MMP, pseudo-MMP, and bullous pemphigoid are distinct from each other.
The autoantibodies that develop in patients with MMP can be detected in all of these patients when the disease is active. The autoantibodies are probably pathogenic, just as they are in patients with pemphigus. , The binding of the autoantibody to the autoantigen at the epithelial basement membrane then sets in motion a complex series of events. CD4 (helper) T lymphocytes far outnumber CD8 (suppressor) T-cells in the inflammatory cell population, which develops in the substantia propria of the conjunctiva. Plasma cells, histiocytes, and mast cells are present in very large numbers, and a panoply of cytokines are elaborated from these cells, including macrophage migration inhibitory factor, interferon-γ, and transforming growth factor (TGF)-β, the effects of which are only now being dissected by molecular biologic techniques. , The result of this complex activity is corneal epithelial damage from inflammatory cytokines and from the xerosis, meibomian gland dysfunction, and trichiatic trauma developing as a consequence of cytokine-induced conjunctival fibroblast proliferation and activation, with resultant subepithelial fibrosis.
The diagnosis of MMP is extremely important, given the natural history of the disease, the effective but potentially toxic therapy, and the potential confusion in differentiation from other causes of chronic cicatrizing conjunctivitis ( Box 45.1 ). Too often, patients present during the later stages of the disease. Foster established that 86% of patients have greater than 50% fornix shortening at the time of first clinical diagnosis. The mean duration of symptoms prior to diagnosis of MMP is 2.8 years. Since the initial symptoms of MMP are nonspecific and easily misdiagnosed, the ophthalmologist must maintain a high level of clinical suspicion in cases of unexplained chronic, recurrent conjunctivitis, or chronic nonresponsive dry eye especially when there is any evidence of subepithelial scarring or trichiasis. All scarring in the conjunctiva obligates a clinical explanation to prevent the inevitable progression of MMP. The earlier a diagnosis is reached and appropriate therapy is initiated, the more likely the blinding sequela of MMP can be prevented.
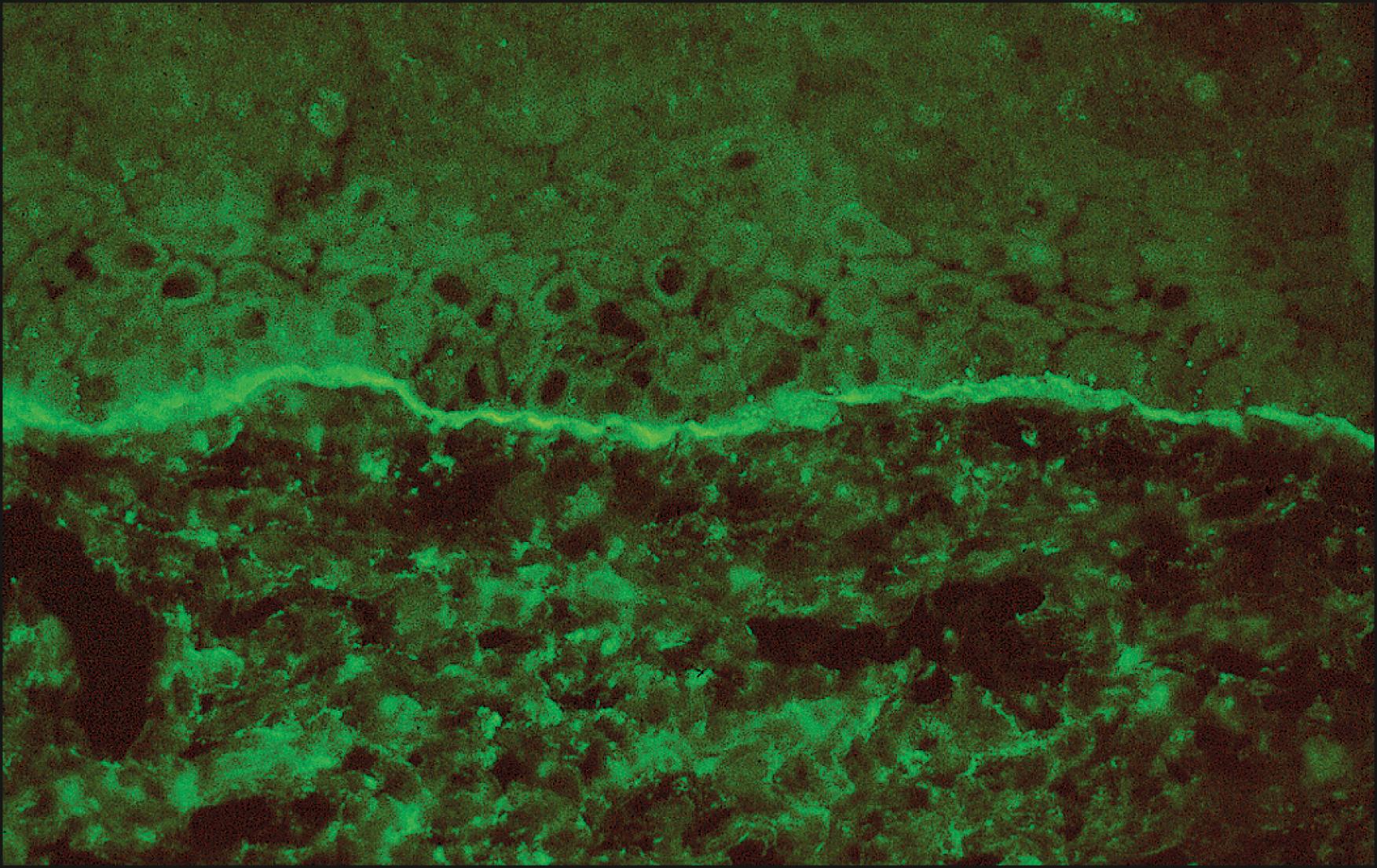
The gold standard for diagnosis of MMP is a conjunctival biopsy using immunofluorescent or immunoperoxidase techniques. Homogeneous linear deposition of immunoreactants, such as IgG, IgA, IgM, and Complement 3 component (C3) along the BMZ of inflamed conjunctiva, is diagnostic of MMP ( Fig. 45.1 ). The rate of positive biopsies has varied in the literature from 20% to 67%. A negative biopsy does not exclude MMP and further investigation and rebiopsy may be indicated depending on the degree of clinical suspicion. A repeat biopsy should employ a more sensitive immunoperoxidase staining with supplemental avidin-biotin complex (ABC) methodology. In 1991, Tauber and coworkers reported an increase in sensitivity of conjunctival biopsies from 52% to 83% with the addition of immunoperoxidase testing to standard immunofluorescent studies.
When a conjunctival biopsy is suggested from the clinical features to diagnose MMP, the tissue needs to be obtained from an area abutting inflamed and noninflamed or scarred conjunctiva. Fresh tissue should be sent immediately for immunofluorescent studies; if immediate testing cannot be performed, then the specimen can be placed and maintained in Zeus or Michel fixative. One must underscore that the most important maneuver to improve the positive yield of biopsies is to sample the interface of inflamed and uninflamed regions. Also, if multiple mucous membranes are involved, the initial biopsy should be taken from one of the nonocular sites less fraught with complications.
Few laboratories (even dermatopathology labs) are sufficiently equipped and experienced to diagnose MMP, which involves the processing of small pieces of conjunctiva, snap freezing and cryostat sectioning, and performing not only immunofluorescent probing studies, but also the much more tedious yet more sensitive immunoperoxidase ABC studies, which are often positive even when the immunofluorescent studies are negative.
Pemphigus is an important histopathologic differential diagnostic consideration but involves the conjunctiva far less frequently than MMP. The former is an intraepithelial blistering disease while MMP is focused on the basement membrane region. In pemphigus, autoantibodies are directed against the intercellular desmosomal connections conducing to cavities containing rounded acantholytic cells that have lost their attachments to each other. The basal germinal cells sit on the basement membrane in a “tomb-stoning” fashion. Immunofluorescence techniques will demonstrate the deposition of autoantibodies between the epidermal or conjunctival epithelial cells in the intercellular space.
MMP has to be distinguished from many mimickers that can provoke chronic cicatrizing conjunctivitis. An extensive list of causes of chronic cicatrizing conjunctivitis can be found in Table 45.1 . Obtaining a careful clinical history from the patient, elicitation of systemic diseases through a review of symptoms and other organ systems, a review of medications used (topically and systemically), determination of timing of symptoms, bilaterality, and exposure to infectious agents can guide the clinician to a proper diagnosis.
| Autoimmune |
|---|
| Ocular cicatricial pemphigoid, Stevens-Johnson syndrome, graft-versus-host disease, sarcoidosis, granulomatosis with polyangiitis, systemic lupus erythematosus, Sjögren syndrome |
| Conjunctival |
| Atopic blepharoconjunctivitis, ligneous conjunctivitis, rosacea blepharoconjunctivitis |
| Infectious |
| Bacterial: Corynebacterium diphtheriae , β-hemolytic streptococcus, Neisseria gonorrhea |
| Viral: Adenovirus, herpes simplex conjunctivitis |
| Chlamydia : Trachoma, Lymphogranuloma venereum |
| Medication-induced |
| Systemic: practolol, D-penicillamine |
| Topical: epinephrine, echothiophate iodide, pilocarpine, idoxuridine |
| Trauma |
| Chemical burns, thermal burns, mechanical trauma, radiation damage, conjunctival surgery, carotid-cavernous fistula |
| Systemic bullous diseases |
| Toxic epidermal necrolysis, epidermolysis bullosa acquisita, pemphigus vulgaris |
Although a definitive tissue diagnosis is helpful to confirm the diagnosis of MMP, lack of a positive biopsy should not exclude the diagnosis or prevent systemic treatment if warranted by clinical exam. A significantly higher proportion of patients with ocular disease alone (46.2%) had negative biopsies compared to those with both ocular and extraocular disease. Yet, the negative biopsy patients present and have a clinical course similar to that of biopsy positive patients. The diagnosis of MMP can be made based on clinical findings and careful exclusion of other causes; therefore lack of a positive biopsy should not prevent or delay initiation of systemic treatment.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here