Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The “climacteric” refers to the phase in a woman's reproductive life when a gradual decline in ovarian function results in decreased sex steroid production with its sequelae. Because this phase is a normal consequence of the aging process, it should not be considered an endocrinopathy. Menopause refers to the last menstrual period, and this occurs on average at age 51.5 years. The perimenopause refers to the several years of more gradually decreasing ovarian function that may be associated with the symptoms of reduced estrogen levels.
Men produce gametes (sperm) frequently and well into their seventh and eighth decade of life. Women are born with all of the gametes (eggs) they will ever have. At birth, several million oocytes are present in both ovaries. Through a process of atresia (physiologic loss), about 400,000 oocytes remain in both ovaries at the time of menarche. Generally, only about 400 oocytes will ovulate during the reproductive life, which typically extends from age 15 to 50 years, when no more effective oocytes remain. Menopause represents the last uterine bleeding from hormones that have been produced by a responsive ovarian follicle. It also represents the end of a woman's reproductive life.
The signs and symptoms of the perimenopause and menopause are related to progressively decreasing secretion of estrogen from the ovarian follicle. The symptoms and signs include hot flashes, insomnia, irritability, and memory loss early, with vaginal atrophy and dryness developing later. Calcium loss from bone is a frequent sign of the loss of estrogenic effect. Stress urinary incontinence and collagen loss from skin are widely reported.
Widespread hormone replacement at or before the menopause has now evolved into more selective and shorter-term hormonal therapy for those women who have significant menopausal symptoms. Prospective studies in both the U.S. and the United Kingdom have confirmed some benefits (less hot flashes, mood changes, bone loss, and colorectal cancer) but have also documented increased risk of breast cancer and stroke when hormones (estrogen and progestin) are used to treat symptoms.
First-line treatment for the menopause should begin with lifestyle changes such as diet and exercise to control mild to moderate symptoms, reserving hormonal therapy for those women who have significant problems. Women with a uterus need combined (estrogen and progestin) hormonal therapy to protect the uterine lining from unopposed estrogen that could lead to hyperplasia and cancer. Careful consideration of the risk to benefit ratio and adequate informed consent should precede menopausal hormonal therapy.
As average life expectancy increases, in the United States and elsewhere ( Table 35-1 ), women and men are often living well into their ninth decade of life. The preservation of their quality of life in terms of both physical and mental activity is a high priority for them. Many women will live for 30 to 40 years after reproductive function ends.
| Year | Age |
|---|---|
| 1900 | 48 yr |
| 1950 | 72 yr |
| 2000 | 79 yr |
| 2015 | >80 yr |
The “climacteric” refers to a period of time when decreasing reproductive capacity occurs in both men and women. For women, this period in their lives is marked mostly by the last menstrual period or menopause and a variable time leading up to the last menses called the perimenopause.
Menopause literally refers to the last menstrual period. The exact time of menopause is usually determined in retrospect; that is, 1 year without menses. In most women, menopause occurs between the ages of 50 and 55 years, with an average age of 51.5 years, but some have their menopause before the age of 40 (premature menopause), whereas a few may menstruate until they are in their 60s.
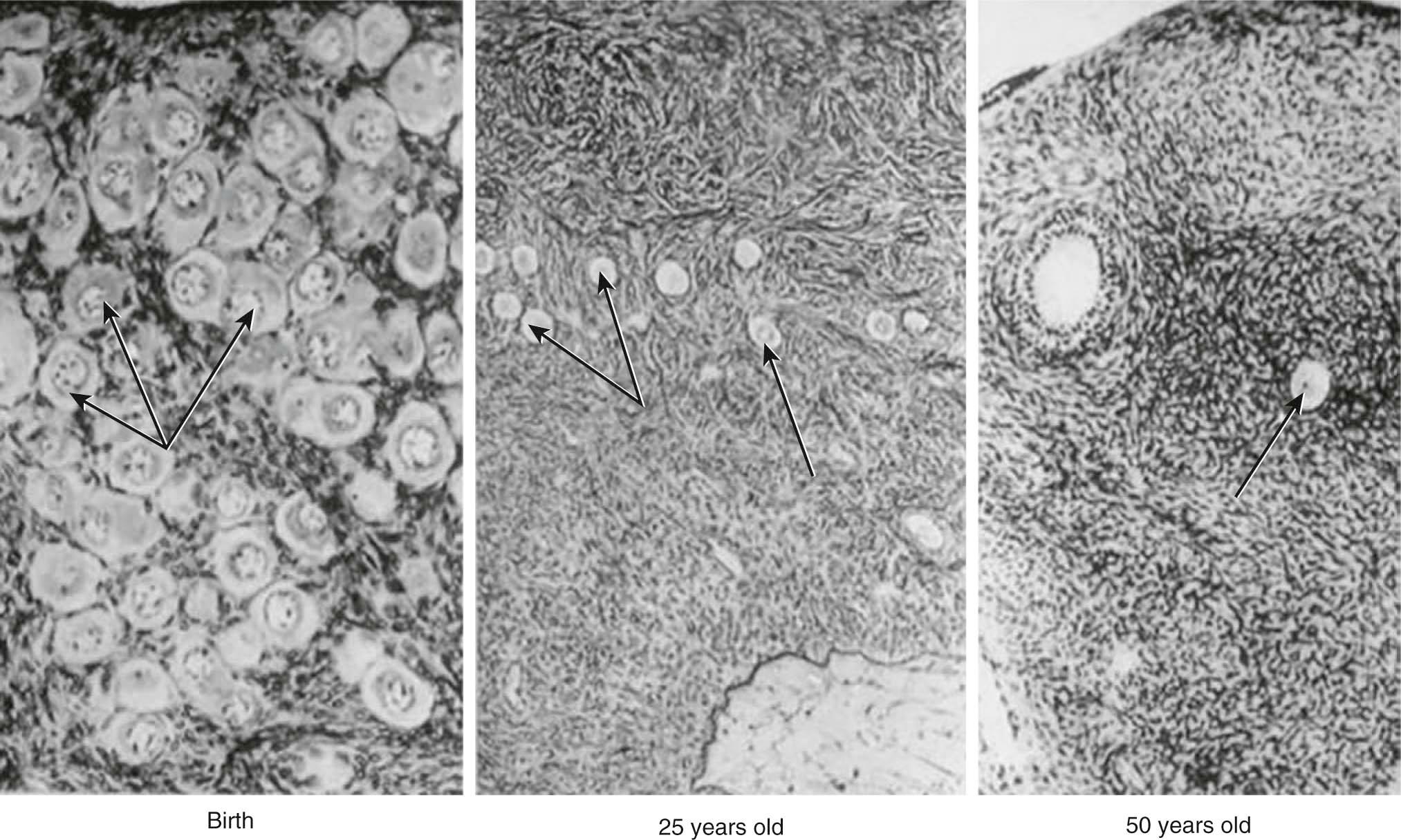
Women are born with between 1.5 and 2 million oocytes (primary ovarian follicles) and reach menarche (first menstruation) with about 400,000 potentially responsive eggs. Figure 35-1 illustrates the decreasing density of oocytes from birth until age 50 years. Most women ovulate about 400 times between menarche and menopause and during this time, nearly all other oocytes are lost through atresia. When the oocytes either have all ovulated or become atretic, the ovary becomes minimally responsive to pituitary gonadotropins, the ovarian production of estrogen and progesterone ends, and ovarian androgen production is reduced. These hormonal alterations often result in unpleasant and even harmful physical, psychological, and sexual changes in postmenopausal women, which can have a negative impact on their quality of life.
Menopause rarely occurs as a sudden loss of ovarian function. For some years before menopause, the ovary begins to show signs of impending failure. Anovulation becomes common, with resulting unopposed production of estrogen and irregular menstrual cycles. Occasionally, heavy menses, endometrial hyperplasia, and increasing mood and emotional changes may occur. In some women, hot flashes (or flushes) and night-sweats begin well before the last menses. These perimenopausal symptoms may occur 3 to 5 years before there is complete loss of menses and postmenopausal levels of hormones are reached.
Some women may suffer a more abrupt loss of estrogen. This usually occurs following a surgical intervention that removes or damages the ovaries or their blood supply or occasionally, following chemotherapy or radiotherapy for cancer. Women who are overweight may continue to produce estrogen indirectly in substantial amounts for many years after menopause. Androstenedione from the ovary and the adrenal gland is converted in peripheral fat tissues to estrone, which is then capable of maintaining the vagina, skin, and bone in reasonable cellular tone and reducing the incidence of flashes. Although this unopposed estrogen may be beneficial to women in terms of symptom control, it is also responsible for the increased incidence of endometrial or breast cancer among obese women. It is important that all postmenopausal women have regular breast examinations and, if abnormal vaginal bleeding occurs, endometrial sampling.
Women who reach menopause before the age of 40 years are said to have premature menopause or premature ovarian failure. Other causes of premature ovarian failure include abnormal karyotypes involving the X chromosome, the carrier state of the fragile X syndrome, galactosemia, and autoimmune disorders that may cause failure of a number of other endocrine organs.
The ovary produces a sequence of hormones during a normal menstrual cycle. Under the influence of luteinizing hormone (LH), cholesterol from the liver is used to produce the androgens, androstenedione and testosterone, in the theca cells of the ovarian follicle. They, in turn, are converted in the granulosa cells immediately surrounding the oocytes into estrogen. Following ovulation, the luteal cells (luteinized granulosa cells) manufacture and secrete progesterone as well as estrogen. The synthesis of these sex hormones depends on the presence of viable follicles and ovarian stroma and the production of follicle-stimulating hormone (FSH) and LH in adequate amounts to induce their biosynthetic activity.
Following menopause, estradiol (E2) values decline (to only 10 to 50 pg/mL), but estrone levels may increase. Estrone (E1) can be produced by peripheral conversion of androstenedione from the ovary and the adrenal gland. In some women, the amount of postmenopausal estrogen may be considerable.
Women normally produce significant quantities of androgens by the metabolic conversion of cholesterol to both androstenedione and testosterone. Although the major portion of androgen is aromatized to estrogen, some androgen circulates. After menopause, there is a decrease in the level of circulating androgens, with androstenedione falling to less than half that found in normal menstruating young women, whereas testosterone gradually diminishes over about 3 to 4 years. Even though postmenopausal women produce less androgens, they tend to be more sensitive to them because of the lost opposition of estrogen. This sometimes results in unwelcome changes such as excessive facial hair growth and decreased breast size.
With anovulation during the climacteric and ovarian failure after the menopause, the production of progesterone declines to low levels. The minimal progesterone present is insufficient to induce those cytoplasmic enzymes (estradiol dehydrogenase and estrone sulfuryltransferase) that convert estradiol to the less potent estrone sulfate and to reduce the levels of cellular estrogen receptors. Altogether, this may result in increased estrogen-induced mitosis in the endometrium. The absence of progesterone also prevents the secretory histologic transformation in the endometrium and its subsequent sloughing. As a consequence, perimenopause is often associated with irregular vaginal bleeding, endometrial hyperplasia and cellular atypia, and an increased incidence of endometrial cancer.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here