Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
During the reproductive years (puberty to menopause), menstrual bleeding normally occurs every 24 to 38 days, except during the first few years of menstruation, during and for a short time after pregnancy and lactation, and in the perimenopausal period. The normal duration of bleeding is 4.5 to 8 days, and the amount of normal flow is less than 80 mL of blood. Brief deviations from normal bleeding patterns occur in many women. Once pregnancy and malignancy are ruled out, short episodes of abnormal uterine bleeding (AUB) resolve spontaneously with little or no treatment.
Some women may experience heavy irregular AUB during their reproductive years. The causes of most cases of heavy bleeding are benign, and symptoms are often effectively managed with hormonal treatment alone. Up to 20% of women experience debilitating symptoms caused by heavy bleeding at some point during their reproductive years. Heavy menstrual bleeding may result from systemic disorders, coagulation defects, or diseases of the reproductive system.
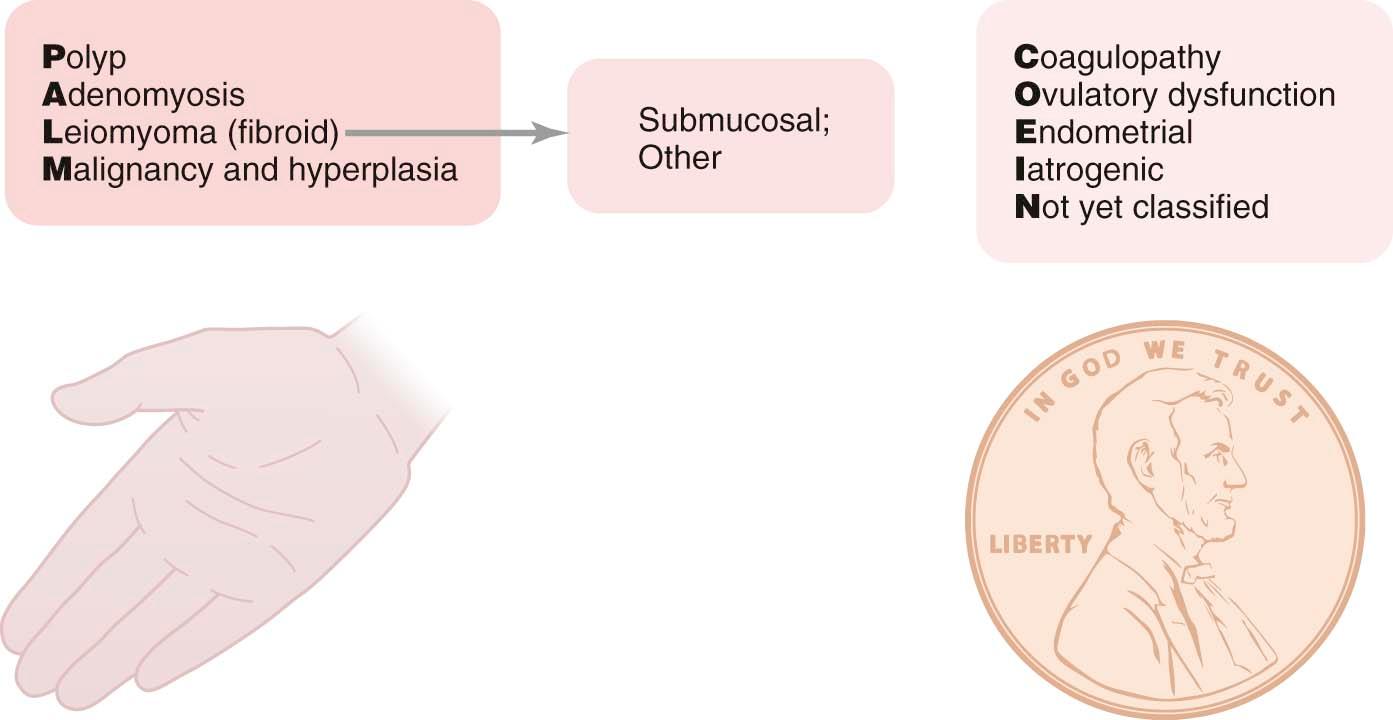
Traditional terminology for AUB has been replaced by more accurate descriptions of the frequency, regularity, duration, and amount of menstrual flow. A newer system for categorizing the causes of AUB (PALM-COEIN) helps to organize the evaluation and treatment of women with bleeding disorders.
After first determining that the source of vaginal bleeding is the uterus, a series of tests is recommended to determine the cause of the AUB. Except in extreme cases, the initial therapy is medical, with a variety of hormonal and nonhormonal regimens available to control the bleeding.
Surgical therapy is reserved for those women for whom medical management fails or for those who have obviously significant pathology (e.g., polyps) or life-threatening hemorrhage when they first present with AUB.
Abnormal uterine bleeding (AUB) patterns (unrelated to pregnancy) are common and can range from complete absence of bleeding (amenorrhea) to life-threatening hemorrhage. The etiology of the bleeding irregularities includes benign or malignant growths, systemic disease, coagulation defects, and hormonal imbalance. Bleeding pattern disruptions caused by imbalance of hormones were previously termed dysfunctional uterine bleeding (DUB). Newer terminology has been introduced to more accurately describe most abnormal bleeding patterns, and a new, more inclusive classification system has been adopted to categorize the various causes of AUB.
Initially, abnormal vaginal bleeding is assumed to emanate from the uterus. A pelvic examination, including the insertion of a vaginal speculum, is essential to eliminate the possibility that the vulva, vagina, exocervix (or ectocervix), or even the rectum or bladder is actually the source of the bleeding. Early pregnancy and its complications should always be ruled out as the cause of AUB in women of reproductive age.
The newer terminology for menstrual bleeding provides information about four dimensions of a woman's cycle: (1) frequency, (2) regularity, (3) duration, and (4) blood loss. Table 26-1 outlines the normal and abnormal values for each of these dimensions and provides the newer terms to describe the abnormalities. As an example, the assessment of abnormal bleeding in a woman with complaints of “irregular menstruation” can be categorized as follows: If her cycle length (first day of menses to the first day of the next menses) is 23 days, she bleeds for 10 days during each cycle, and she loses 100 mL of blood, this would be described as “frequent, prolonged, and heavy menses.” Other important traditional terms include amenorrhea, which refers to the absence of any menstrual bleeding or spotting for at least 3 months; intermenstrual bleeding, which refers to bleeding between normally spaced menses; and postcoital bleeding, which refers to bleeding after vaginal intercourse.
| Clinical Dimensions | Descriptive Terms | Normal Limits (5th to 95th Percentiles) |
|---|---|---|
| Frequency of menses (days) | Frequent | <24 |
| Normal | 24-38 | |
| Infrequent | >38 | |
| Absent | — | |
| Regularity of menses, cycle-to-cycle variation over 12 mo | Regular | Variation ± 2-20 days |
| Irregular | Variation >20 days | |
| Duration of flow (days) | Prolonged | >8.0 |
| Normal | 4.5-8.0 | |
| Shortened | <4.5 | |
| Volume of monthly blood loss (mL) | Heavy | >80 |
| Normal | 5-80 | |
| Light | <5 |
This newer, more descriptive terminology for patterns of AUB replaces the older, less precise terms listed in Box 26-1 . However, it is important to become familiar with these older terms, because they have been used for decades in clinical practice and in the medical literature and are still used for diagnostic coding purposes.
* Less descriptive terms that are no longer recommended.
Polymenorrhea: Abnormally frequent menses at intervals of less than 24 days
Menorrhagia (hypermenorrhea): Excessive and/or prolonged menses (>80 mL and >7 days) occurring at normal intervals
Metrorrhagia: Irregular episodes of uterine bleeding
Menometrorrhagia: Heavy and irregular uterine bleeding
Dysfunctional uterine bleeding: Bleeding caused by ovulatory dysfunction
The newer classification system, called PALM-COEIN, is depicted in Figure 26-1 . Appropriate testing is needed to differentiate the various causes of AUB. The classification system takes into account that there are two different influences on AUB. On the one hand, a woman may have structural abnormalities of her uterus that are the likely causes of her bleeding, with the PALM elements standing for p olyps, a denomyosis, l eiomyomas (fibroids), and m alignancies. Rare problems such as imperforate hymen or transverse vaginal septum are more likely to present with primary amenorrhea and not with chronic bleeding problems. The COEIN portion of the classification system refers to important functional disorders such as c oagulation defects, o varian dysfunction (formerly DUB), e ndometrial (uterine cavity lining) causes, and i atrogenic. A “ n ot yet classified” category completes the acronym and is available for a cause of bleeding that is not currently included or idiopathic.
Chapter 33 covers the causes of infrequent menses (oligomenorrhea) and both primary and secondary amenorrhea. Chapters 35 and 41 address perimenopausal and postmenopausal bleeding. This chapter is focused on the etiology, differential diagnosis, evaluation, and treatments for both acute and chronic heavy menstrual bleeding.
Heavy menstrual bleeding occurs in 9-14% of healthy women of reproductive age and is the reason for up to 20% of outpatient clinic visits by women. Heavy menstrual bleeding can cause severe anemia, but less significant blood loss can diminish a woman's quality of life and even her income when workplace activity is adversely affected.
The etiologies, workups, and therapies of excessive bleeding can differ for acute heavy bleeding compared with chronic heavy bleeding, although often there is considerable overlap. A woman who presents with heavy bleeding needs to be assessed for hemodynamic stability, anemia, and always the possibility of pregnancy. She should be asked about symptoms of dizziness, shortness of breath, or loss of consciousness. Her vital signs must be assessed for hemodynamic stability. It is helpful to get a description of her current bleeding episode as well as her recent and usual bleeding patterns, along with any previous evaluations or treatments. A complete history, including medication history, can provide insight into which of the PALM-COIEN categories is more likely, but a broad differential should be developed. It is quite possible for a woman to have more than one problem as the cause of her abnormal bleeding. Obvious causes requiring immediate surgeries should be ruled out, such as vaginal trauma or bleeding lacerations, as well as aborting fibroids (leiomyomata).
Hospitalization and transfusion are generally recommended for women who have severe anemia (hemoglobin ≤7 g/dL) and those who are hemodynamically unstable. Outpatient transfusion is an option for women with borderline presentations. Patients who decline blood transfusions or blood products in spite of severe anemia should be cared for by a team experienced with other treatment options. Before a transfusion is started, blood tests should be performed. Box 26-2 lists the tests that should be considered for the workup of AUB.
Urine tests
Pregnancy test
Blood tests
Blood count with reticulocyte count and differential
Serum iron and iron-binding capacity
Serum ferritin
Coagulation tests (PT, PTT, and INR)
Thyroid function tests
Liver function tests
Creatinine, BUN
Imaging tests, if indicated
Pelvic ultrasonography
Saline infusion sonography
Biopsies as necessary
Cervical biopsy
Endocervical biopsy
Endometrial biopsy
BUN, Blood urea nitrogen; INR, international normalized ratio; PT, prothrombin time; PTT, partial thromboplastin time.
Baseline hemoglobin is mandatory, and a complete blood count (with red blood cell indices) is performed to determine the chronicity of the problem, to rule out thrombocytopenia, and to identify possible hematologic malignancies. Coagulation factors should be obtained, as well as serum iron, iron-binding capacity, and serum ferritin levels. Following these initial assessments, liver, renal, and thyroid function tests may help to identify other systemic causes of excessive uterine bleeding.
Many of the test results may not be available for days, but the heavy bleeding needs to be promptly controlled. First-line therapy is generally medical. Surgical approaches are usually reserved for women whose condition does not respond to medical therapies and for those who are bleeding so heavily that there is insufficient time to consider medical treatments. First-line medical therapy usually involves hormonal manipulations ( Box 26-3 ).
Conjugated equine estrogen 30 mg intravenously every 3 hr for up to 24 hr
OR
50 µg of ethinyl estradiol (EE), 0.15 mg of levonorgestrel, one tablet orally every 6 hr for 5 days
Medroxyprogesterone acetate 20 mg orally every 8 hr for 7 days, then once daily for 21 days
OR
Oral contraceptive pills with 35 µg of EE, 1.0 mg of norethindrone acetate, one tablet orally every 8 hr for 7 days, then 20 µg of EE, 1.0 mg of norethindrone acetate pills, one tablet orally once daily for 21 days
OR
Medroxyprogesterone acetate 20 mg orally every 8 hr for 3 days with intramuscular injection of depot medroxyprogesterone acetate 150 mg
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here