Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Abdominal hysterectomy is one of the most frequently performed surgical procedures in the United States. The basis for this operation is an open abdomen (laparotomy), which provides adequate exposure for isolation of the uterus and adnexa from surrounding structures to allow cutting and securing of support structures that attach the uterus to the pelvic floor and sidewalls.
These supporting structures include (1) vascular pedicles together with their peritoneal and connective tissue investments (e.g., infundibulopelvic ligament, uterine artery and veins); (2) muscular supports (e.g., the round ligaments); (3) connective tissue–vascular/neural condensations (e.g., cardinal, uterosacral ligaments); and (4) fat and peritoneum (e.g., broad ligament, uterovesical, uterorectal folds).
Strategic surrounding structures include the bladder anteriorly, the rectum posteriorly, and the ureters and great vessels laterally.
The blood supply to the uterus emanates from the hypogastric arteries and via the ovarian arteries from the aorta. The venous drainage enters the hypogastric veins, the vena cava (right ovarian), and the left renal vein (left ovarian). The uterine artery crosses from the anterior division of the hypogastric artery obliquely above the ureter to join the uterus at the junction of the corpus and cervix. The artery divides into a larger, ascending branch and a smaller, descending branch that supplies the cervix and anastomoses with the vaginal artery. The latter also takes origin from the anterior division of the hypogastric artery.
After the abdomen has been opened and the intestine carefully packed, a self-retaining retractor is placed ( Fig. 13.1A and B ). The abdomen has been previously explored. The pelvic contents in the operative field are identified, and any disease or anatomic distortion is noted ( Fig. 13.2 ).


Thus, surgery is performed in a logical stepwise fashion.
The round ligaments are clamped, divided, and suture-ligated with 0 Vicryl ( Fig. 13.3A to C ).

The bladder flap is cut by grasping the peritoneum of the vesicouterine fold just below its reflection onto the uterus ( Figs. 13.4 and 13.5A to D ). Steps 1 and 2 are repeated on the opposite sides ( Fig. 13.6 ).



With the use of a sponge forceps, the bladder is gently pushed inferiorly from the cervix. Care is taken to stay in the midline, pushing onto the cervix ( Figs. 13.7A and B and 13.8 ). If the patient has had previous surgery (e.g., a cesarean section), the bladder should be separated from the uterus by sharp dissection.


The infundibulopelvic ligaments (ovarian arteries and veins) are isolated from the ureter and triply clamped ( Fig. 13.9A to E ). The ligament is divided between the first and second clamps. The vessels are doubly ligated with the tissue beneath the lowermost clamp simply ligated or suture-ligated. The tissue beneath the second (middle) clamp is suture-ligated with 0 Vicryl ( Fig. 13.10 ).


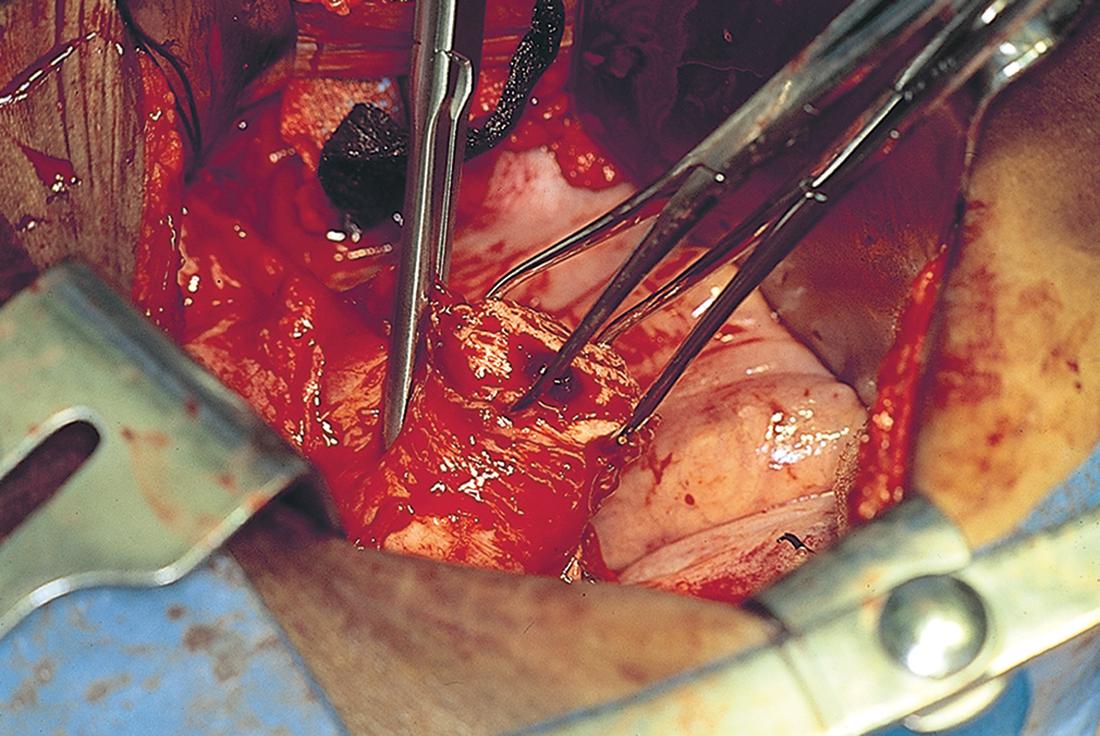
The uterine vessels are skeletonized (i.e., excessive connective tissue is trimmed away, denuding the vessels) ( Fig. 13.11A and B). The vessels are clamped, with this first clamp applied tightly to the uterus ( Fig. 13.11C and D ). A second clamp is applied directly above, never below, the first uterine vessel clamp ( Fig. 13.12 ). Finally, a third clamp is applied above the second to secure back-bleeding ( Fig. 13.13A and B ). The uterine vessels are cut with scissors or a scalpel ( Fig. 13.14A and B ). Next, the uterine vessels are doubly suture-ligated with 0 Vicryl, with care taken to pass the needle immediately beneath the tip of the clamp ( Fig. 13.15A and B ). The clamps (with the exception of the uppermost clamp) are removed after suture placement (see Fig. 13.14B ). The procedure is identical for the right and left sides.





The cardinal ligaments are clamped in juxtaposition to the uterus, with care taken to avoid infringement of the ureter, which is very close to the uterine cervical junction. The upper portion of the cardinal ligament is then cut ( Fig. 13.16A to E ). The procedure is carried out on either side. The ligaments are sutured with 0 Vicryl with a transfixing stitch.

The uterosacral ligaments on either side are clamped, cut, and suture-ligated. This again is carried out close to the uterus because farther back (posteriorly), the ligaments are intimately associated with the ureters. In fact, definite identification of the ureter once again is advised at this point in the procedure. Finally, the cervix is palpated and is confirmed to be separate from the vagina. A clamp is placed across the vagina after it has been confirmed that the margin of the urinary bladder is free and clear. The specimen is removed and the vagina is closed ( Fig. 13.17A to J ).

Alternatively, particularly if the corpus is bulky, the uterus may be “subtotaled” (i.e., the body of the uterus is amputated from the cervix). The uterus is elevated (the remaining clamps are those applied to prevent back-bleeding during step 5) ( Fig. 13.18 ). A sharp scalpel cuts the cervix free from the corpus ( Fig. 13.19 ).


The cervix is grasped with two tenacula, and the superficial portion of the lower part of the cardinal ligament is clamped on each side. Note that the clamp is applied close to the sides of the cervix away from the ureter ( Fig. 13.20A and B ). The pubovesical cervical fascia is incised and pushed inferiorly, creating a plane between the bladder base and the cervix ( Fig. 13.21 ). Finally, straight clamps are placed along the lowest portion of the cardinal ligaments, with the tips of the clamps within the peeled down pubovesical cervical fascia ( Fig. 13.22 ). The ligaments are cut with a sharp scalpel and sutured with a 0 Vicryl transfixing stitch ( Fig. 13.23 ).



The bladder is pushed farther inferiorly, with use of the established infrafascial plane within the pubovesical cervical fascia. Note that the vagina is behind and the bladder and ureters are in front of the plane. Clamps are applied within the pubovesical cervical fascial plane to secure the vaginal angles ( Fig. 13.24 ). The cervix is cut away from the top of the vagina, and a small margin of vagina is incorporated with it ( Fig. 13.25 ). The vaginal angles are secured, and the vagina is closed with interrupted figure-of-8 sutures of 0 Vicryl ( Figs. 13.26 and 13.27A ). Alternatively, the vaginal cuff may be left open by suturing the edges with a continuous running lock suture of 0 Vicryl ( Fig. 13.27B ). The wound should be irrigated to facilitate identification of bleeding sites.




Next, the vagina is suspended by suturing the stumps of the cardinal and uterosacral ligaments to the vaginal vault ( Fig. 13.28 ).

Finally, the peritoneum is carefully closed. The position of the ureter must be definitely identified so as not to ligate it during this phase of peritoneal closure.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here