Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
hepatitis A virus
immunoglobulin G
immunoglobulin M
The hepatitis A virus (HAV) is a nonenveloped, small, single-stranded RNA picornavirus that replicates within hepatocytes, producing symptomatic or asymptomatic infection in humans. Hepatitis A induces an immune response that causes hepatic inflammation and interferes with hepatic function. Hepatitis A leads to an acute and generally self-limited infection with symptoms including fever, nausea, abdominal pain, and jaundice. This infection results in immune protection against the virus.
HAV transmission is via the fecal-oral route. Transmission occurs with poor sanitation, sexual contact or cohabitation with an infected individual, or intake of contaminated food or drink. For developed nations, available hepatitis A vaccines have led to a dramatic fall in the rates of acute HAV infection. In endemic regions, there are potentially large socioeconomic consequences. In 0.2% of active cases, infection results in acute liver failure and death, and this risk increases with age and the presence of chronic liver disease. In the United States the prevalence of HAV infections has dropped by more than 90% since the initiation of effective vaccination in 1997. However, hepatitis A remains the cause of approximately half of all known cases of acute viral hepatitis in the United States. More than 20,000 cases of hepatitis A occur annually in the United States, and there are approximately 1.5 million known cases worldwide. The diagnosis of hepatitis A depends on detection of serum anti-HAV immunoglobulin M (IgM), detectable 5 to 10 days after exposure. IgM gradually disappears by 6 months after infection. Anti-HAV immunoglobulin G (IgG) develops in early infection and generally lasts for life.
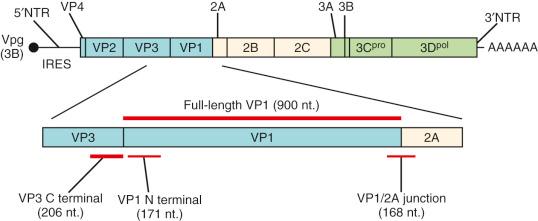
A viruslike antigen was discovered in 1973 by immune electron microscopy, and was identified as a likely causative pathogen for acute infectious hepatitis. It had previously been seen only in primates, although human forms have unique genotypes. Previously known as enterovirus type 72 , HAV is the only species of the genus Hepatovirus . It is one of the large and diverse positive-strand RNA group of viruses making up the family Picornaviridae (picornaviruses). It is unique within this family for its structure and life cycle, as well as its tropism for the liver. It has a primitive capsid structure related to picorna-type viruses, which infect insects. Evolutionary ancestral forms have also been found in bats and shrews. HAV is a nonenveloped, icosahedral particle 27 nm in diameter. It infects its host via the fecal-oral route and is shed in feces as a naked particle but circulates in blood in an envelope produced from host cell membranes. The RNA genome is positive sense, single stranded, and 7.5 kb. Its unique features include an internal ribosome entry site structure, a truncated VP4 capsid protein lacking N-terminal myristoylation, a C-terminal pX extension of VP1, VP2 late domains involved in membrane envelopment, and a cis -acting replication element within the 3Dpol sequence ( Fig. 35-1 ). The HAV genome includes a short 3′ noncoding region that ends in a polyadenylic acid tract, a 5′ untranslated region of 734 bases, and a single, long open reading frame encoding a polypeptide of 2227 amino acids.
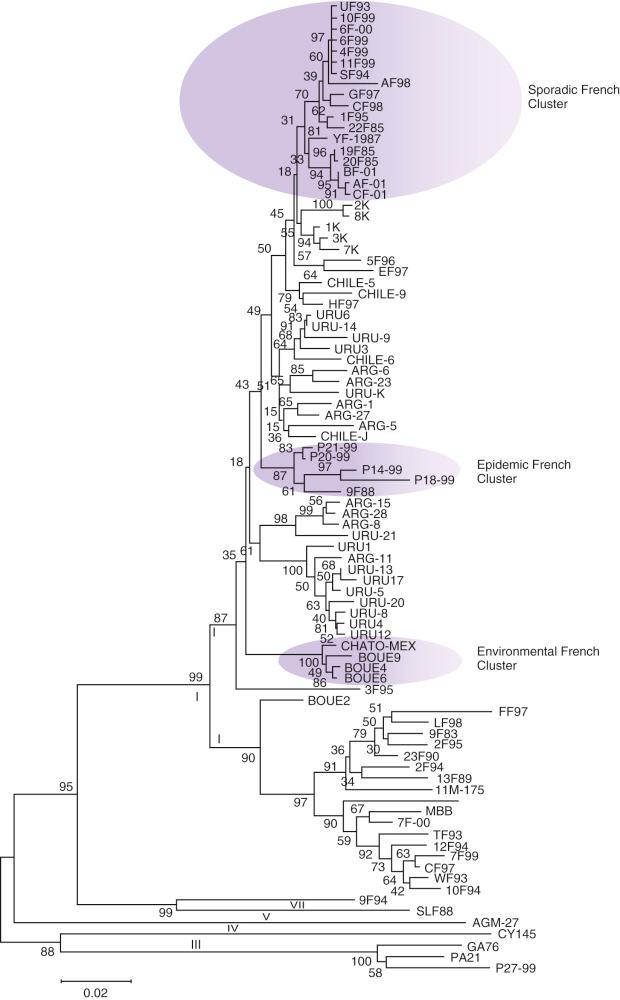
HAV strains have minimal variation over time or place. Genomic characterization of HAV strains from various geographic locations has been performed. With use of a short fragment of the VP1-2A junction region to classify strains, seven different genotypes based on more than 15% nucleotide variation among isolates, and subgenotypes with 7.5% to 15% nucleotide variation have been identified. By VP1-2A junction and VP1 gene evaluation analysis, four genotypes (I, II, III, IV)—each with two subtypes (A and B) in humans and three other genotypes (V, VI, VII) in primates ( Fig. 35-2 )—were revealed. Full-length VP1 sequencing revealed a novel 45-nucleotide deletion variant resulting in a 15–amino acid deletion located in the VP1 region with neutralization escape mutations as antigenic variants. This analysis showed a great level of genetic diversity at the nucleotide (23.5%) and amino acid (10.5%) levels. Most humans have genotype 1 virus, with potential for cocirculation of subgenotypes 1a and 1b demonstrated in one case series. There is only a single major serotype which is felt to be stable given the mode of substitution to VP1 by nonsynonymous substitutions.
During early infection, HAV reaches the basilar surface of hepatocytes through the space of Disse. Attachment to HAV-CR-1, a mucinlike glycoprotein cellular receptor, facilitates entry of the virus into the cell. The asialoglycoprotein receptor mediates infection by binding and internalizing HAV-specific immunoglobulin A molecules. A cell surface molecule, T-cell immunoglobulin and mucin 1, serves as a receptor for HAV.
HAV has subtle but key structural differences as compared with other known picornaviruses (see Fig. 35-1 ). HAV structure lies between classic picornaviruses and the insect picorna-like viruses. Picornaviruses induce restructuring of host intracellular membranes, which allows replication of the genome. They consist of polyprotein with three portions, P1, P2, and P3. P1 codes for capsid proteins (VP1 to VP4), and P2 and P3 have enzymes, accessory proteins, and precursors needed for replication of the virus with polyprotein processing (2A to 2C and 3A to 3D). Polyprotein processing for Hepatovirus occurs between 2A and 2B because of a viral proteinase 3Cpro. This has radically different amino acid preferences at the P4 and P2′ positions of the substrate compared with enteroviral 3C proteinases. HAV 3Cpro cleaves 2A-2B between Gln836 and Ala837, 144 residues higher than the enteroviral junction, resulting in a truncated 2A protein (71 to 73 amino acids) and a longer 2B protein (251 amino acids long). The membrane-targeting proteins 2B and 2C, along with their precursor 2BC, and protein 3A have primary involvement in membrane remodeling and have sequences that allow integration into host membrane bilayers. They rearrange target membranes during infection and tether the RNA replication complex to these. The fibrillar aggregation of the 2B protein pulls together the viral and cellular components needed for HAV replication. Given low HAV viral expression, this recruitment ensures newly synthesized viral factors accumulate in the replication and assembly factories.
HAV has an N -terminal domain swap rendering VP2 similar to the homologous VP1 and VP3 proteins. Thus HAV retains functional and structural features characteristic of primordial picornaviruses, similar to present-day insect picorna-like viruses. The subsequent development of efficient mechanisms of cell entry allowed the growth in diversity characterizing present-day mammalian picornaviruses. HAV cannot shut down host protein synthesis, unlike other modern picornaviruses, grows poorly in tissue culture, and has a highly deoptimized codon usage. Particles are produced with a 67-residue C-terminal extension of VP1, which is implicated in particle assembly (this longer form of VP1 is known as VP1-2A or PX ). Particles containing this extension place themselves within the host membrane, creating enveloped viruses. Host proteases cleave this extension to yield mature capsids. VP4 in HAV is very small (~23 residues) and may not be present within virus particles.
HAV is shed in fecal matter. It may also be spread by contaminated water, sexual contact (especially men having sex with men), personal contact (such as household contacts or at day care centers), and illicit drug use. Approximately 55% of cases globally do not have an identifiable risk factor. Personal protection measures against transmission include avoidance of unhealthy, contaminated drinking water or food. Cooking or boiling water and food for 1 minute or more to 85° C inactivates HAV.
HAV-induced hepatitis presents as a proinflammatory environment in which parenchyma is destroyed by a combination of macrophage- and lymphocyte-induced processes. HAV infection leads to a cellular immune cascade with induction of hepatocyte injury by activation of cytolytic T cells. Liver specimens of patients with hepatitis A contain CD8 + T cells, which lyse infected cells in an HLA class I–restricted manner. Interferon-γ secretion by activated T cells potentially leads to HLA class I determinants on infected liver cell surfaces. The fulminant inflammatory response is accompanied by an increased production by liver Kupffer cells of proinflammatory mediators, including interleukin-1, tumor necrosis factor α, and interleukin-6. Hepatocellular injury is also induced by further immune mechanisms, including natural killer cells and lymphokine-activated killer cells. Apoptosis of liver cells, increased production of oxygen free radicals, and activation of inflammatory and coagulation cascades can result in liver necrosis, with potential for fulminant hepatitis and multiorgan failure.
Each year approximately 1.5 million clinical cases of HAV infection are reported worldwide; the actual infection rate is likely 10 times higher. Reflecting continued poor access to clean drinking water in endemic regions, the World Health Organization estimated the worldwide incidence of acute hepatitis A increased from 115 million to 119 million from 1990 to 2005. Corresponding deaths due to hepatitis A increased from 30,283 to 35,245. Incidence ranging from 15% to 100% strongly correlates with socioeconomic indicators and access to safe drinking water. With a rise in income and access to clean water, the incidence of hepatitis A decreases ( Fig. 35-3 ).
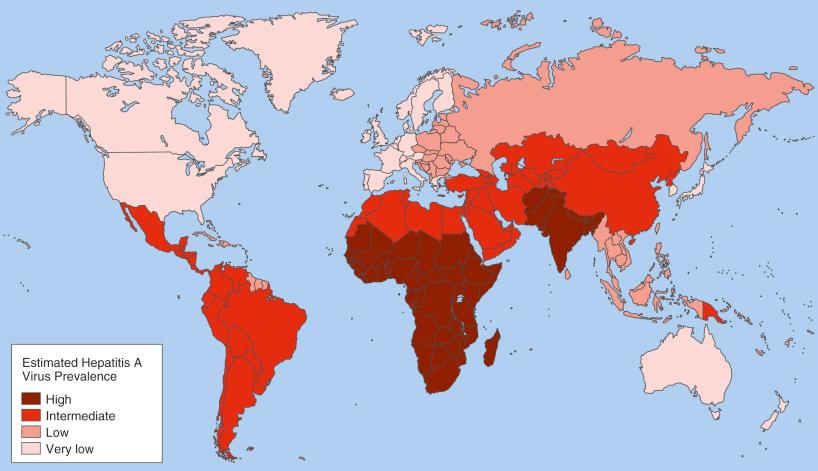
In developing regions, such as India, Africa, the Middle East, and parts of South America, HAV infection is very common (see Fig. 35-3 ). Most infections are asymptomatic and are acquired during early childhood. Individuals in high-endemicity regions are approximately six times more likely to be seropositive than individuals in developed countries. This early exposure reduces the need for vaccination. The reported rates of symptomatic infection are relatively low and outbreaks are not common. In regions with intermediate endemicity, including Southeast Asia, China, and eastern Europe, some community-wide outbreaks occur. Hepatitis A is less common in developed regions, such as western Europe, North America, Scandinavia, Japan, and Australia. Infections in developed countries occur in specific settings, mainly associated with travel.
For most developed nations, there is a general lack of exposure to and immunization against HAV. Seropositivity is generally less than 5% in children and approximately 20% by age 20 years. Most acute HAV infections are due to travel to endemic regions, consumption of contaminated shellfish, and contact with persons with acute HAV infection. Drinking and eating in poor hygienic conditions carries an increased risk, 20 per 1000 individuals per month traveled. Globally, the areas associated with the highest incidence of travel-related disease are East Africa, the Middle East, and the Indian subcontinent. Children aged 0 to 14 years made up 88% of these cases.
Specifically for patients from the United States, approximately 85% of travel-related hepatitis A cases are associated with travel to Central America, Mexico, or South America. Hepatitis A in the United States disproportionately affects specific racial/ethnic groups, including American Indian, Alaska Native, and Hispanic patients. Before recommendations for broad childhood vaccination, the highest seroprevalence of anti-HAV was among Mexican Americans (81.9%) and black adults (50%). Prevalence was lowest among white non-Hispanic adults (29.0%). These disparities among racial/ethnic groups were virtually eliminated with vaccination, with the rates of HAV disease among native American and Hispanic patients decreasing by 98.8% and 86.4%, respectively, to 0.8 and 2.8 cases per 100,000. The rates among non-Hispanic whites, blacks, and Asians decreased by 78.3%, 80.5%, and 63.0%, respectively, to 1.5, 1.5, and 1.7 cases per 100,000 ( Fig. 35-4 ).
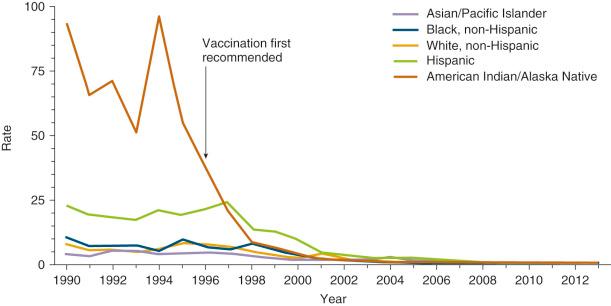
With improvement in education on infectious precautions, the risk of HAV infection in unvaccinated travelers to developing countries has dropped from 3 per 1000 individuals per month of travel to 6 to 30 per 100,000 individuals per month. The incidence of hepatitis A in the United States continues to decline (see Fig. 35-4 ). Nonimmunized individuals traveling to hepatitis A–endemic countries remain at risk of infection. Increased risk is associated with the duration of travel, living conditions, and the incidence of hepatitis A in the destination country. There have been no recent reports of shellfish being the source of a hepatitis A outbreak in the United States, although in other parts of the world, shellfish are a common source of hepatitis A outbreaks. For individuals who live in or visit rural areas, the risk of acute HAV infection is highest in those who travel long distances to remote areas or eat and drink in poor sanitary conditions. A study by Heudorf et al. indicated that there are no significant differences in the incidence of hepatitis A between tourists and business travelers. A study by Mikati et al. of 149 travelers, including 70 immunocompromised travelers (47%), found that the immunocompetent travelers had a risk of acute infection similar to that of immunocompromised travelers.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here