Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Thanks to Cathy Liu and Christine Canilao for assistance with manuscript preparation.
Grant support: National Center for Complementary and Integrative Health R01 R01AT007137 (KT and BDN); NIDDKP50 DK064539 (EAM); NIDDK P30 DK041301.
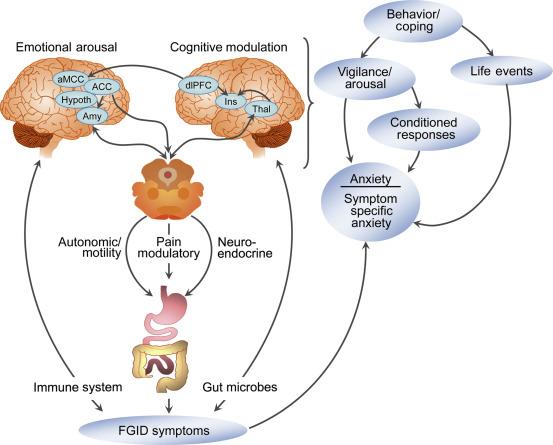
While a variety of peripheral candidate biomarkers related to functional gastrointestinal disorders (FGIDs) continue to be investigated, none appear to account for a large proportion of the symptom variance in this heterogeneous set of syndromes. At the same time, a model for FGIDs that includes a prominent role for brain-gut interactions has emerged and holds promise for helping to elucidate what are likely complex interrelationships between gastrointestinal sensation, motility, immune function, and gut microbes with sensory, cognitive, and affective circuitry in the brain. Brain imaging technologies have been become a standard in the investigation of the pathophysiology of a number of health problems in neurology and psychiatry, as well as various chronic pain conditions, including the FGIDs, where subjective symptom reports are often relied on as primary disease outcomes. Neuroimaging research has often confirmed long-held hypotheses of altered interoceptive, emotional, and cognitive function in FGIDs and increasingly is used to develop a more comprehensive understanding of the interplay between the behavioral aspects of the disorders and their physical symptoms. Fig. 18.1 shows the interaction of the brain and gut in the context of external and internal environmental stimuli. In this chapter, we will highlight the contributions neuroimaging has made to the understanding of the pathophysiology of the most commonly studied FGIDs, irritable bowel syndrome (IBS) and functional dyspepsia (FD), and some of the most promising avenues for neuroimaging research of FGIDs in the future.
The FGIDs are defined by symptom clusters, rather than objective markers of pathophysiology. In fact, there is growing consensus that no single pathophysiological process can adequately characterize any of the individual FGIDs. It is therefore likely that symptoms in a specific patient result from alterations in one or more peripheral and central processes and that this mix varies across individuals and perhaps over time within the same individual. Although there are objective measures for some of the potential peripheral processes (e.g., motility, visceral sensitivity, altered microbiome), subjective responses have been the only measures to determine such factors as illness severity, symptom-related distress or vigilance, and overall response to medications or placebo. Although patient reports remain the gold standard for clinical outcomes, more objective measures are needed to elucidate the brain processes underlying central pathophysiology or a medication's mechanism of action. Pain is the signature symptom of the most prevalent FGIDs, IBS, and FD. The study of FGIDs without including the brain limits our understanding to that of peripheral pain reflex pathways, nonspecific autonomic responses, and symptom reports. Unlike preclinical studies in organic gastrointestinal disorders, animal models of FGIDs remain limited in their predictive value, as surrogate markers for the complex range of symptoms and distress seen in humans with FGIDs are largely not accessible in rodents. This likely explains why such models have largely failed to predict treatment responses of FGIDs in humans. The predominance of higher cortical modulation of subcortical systems seen in humans is not readily replicated in the animal models, and such activity is likely involved in the generation and maintenance of FGID symptoms. Imaging the brain allows us to evaluate the input from the periphery via the interoceptive circuitry in the brain, as well as assess the emotional and cognitive factors in the modulation of the afferent input. Neuroimaging provides a route to objectively assess the central response to a variety of variables including medications, symptoms, gastrointestinal sensations, and psychosocial stress.
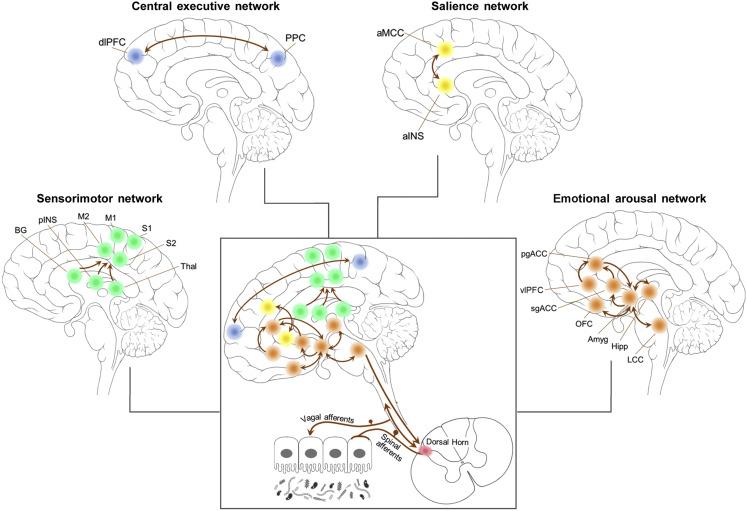
Initial efforts using magnetic resonance imaging (MRI) and positron emission tomography (PET) scanning compared patients and controls by identifying activation in individual brain regions discovered in whole brain analyses or in regions that were selected a priori for their hypothesized relevance to FGIDs. Gradually, the field of neurogastroenterology has advanced from the focus on localized regional activity to directly characterizing regions within brain networks altered in FGIDs compared to healthy controls, and by examining interactions between brain networks. These networks consist of sets of sometimes widely dispersed regions involved in a specific process or function. Based on prior research, clinically driven hypotheses, and primate studies of anatomical connectivity, several networks have been of particular interest in FGIDs. The most consistent brain networks described in FGIDs and other chronic pain syndromes include emotional arousal, central executive control, sensorimotor processing, and salience networks. The emotional arousal network is driven by the amygdala, in communication with the anterior cingulate and prefrontal cortex and extension to the hippocampus and locus ceruleus. It is the network involved in fear-related responses and anxiety related to FGIDs. The central executive network is represented by cortical modulatory regions including the dorsolateral prefrontal cortex and posterior parietal cortex. Impaired function in this network may be associated with diminished cortico-limbic modulation to the emotional arousal network. The sensorimotor network consists of the sensorimotor cortex, posterior insula, basal ganglia, and thalamus which are regions which process somatic and visceral sensation. The salience network is a collection of brain regions working in concert to evaluate the importance of internal or external stimuli and to assist in the coordination of the brain's response to those stimuli. Its main hub is the anterior insula with connection to the anterior mid-cingulate cortex. Descriptions of the salience network can often include additional regions, chiefly the medial prefrontal and orbitofrontal cortex, and amygdala. In FGIDs, the salience network is considered a key region in amplifying the importance of potentially benign body sensations. In the following sections, we will review findings from multiple modalities of neuroimaging and both regional and network-focused studies with an emphasis on these key networks for FGIDs ( Fig. 18.2 ).
Several types of imaging techniques have been used to elucidate brain networks in FGIDs including: (a) functional MRI or PET imaging of task-specific evoked responses or intrinsic connectivity of the brain during a resting state, (b) gray matter morphometric parameters such as cortical thickness, volume, and surface area from structural MRI (sMRI), and (c) diffusion-weighted tensor imaging of microstructural properties of white matter and region to region connectivity. Imaging studies performed in FGID patients using each of these modalities have demonstrated alterations in the above-described brain networks.
The characterization of brain networks requires application of more sophisticated analytical techniques than were used in the early imaging studies. Functional networks and their circuits are analyzed using effective connectivity multivariate pattern analysis including sparse partial least squares and independent component analysis or multivariate regression quantifying the association between voxel-to-voxel or region-to-region activity during evoked responses or time series across the resting state. Using these methods in IBS and, to some extent, in FD studies have generally shown increased activity in emotional arousal and signal salience networks as well as altered sensory processing and diminished corticolimbic inhibition from central executive networks.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here