Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Visceral information reaches the brain through a diverse array of neural, humoral, and immune pathways, conveying an abundance of ascending visceral information that helps to maintain homeostasis within the gastrointestinal (GI) tract. While the vast majority of these physiological processes are subconscious, those that do enter the consciousness include sensations such as hunger, satiety, and the urge to defecate. Contrastingly, at the extreme of this GI sensory spectrum is visceral pain, engendered by a complex interaction between the intraluminal milieu and a plethora of host factors that, in turn, comprise the multifaceted neurobehavioral system. The GI sensory spectrum invokes activity in numerous subcortical and cortical structures via projections from vagal and spinal afferents, which cumulatively results in an individual's unique sensory experience. This chapter will focus on the processing of GI sensation within the brain in health that results in conscious perception with particular attention being paid to the neuroanatomical representations that have been derived from recent functional neuroimaging studies.
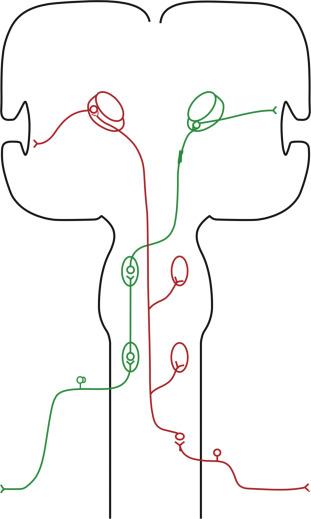
Traditionally, vagal and spinal afferents that innervate the GI tract have been considered to hold distinct roles in mediating GI sensation. For instance, spinal afferents have historically been considered to encode the perception of pain and inhibition of the digestive process in contrast to vagal pathways, which sensed hunger, satiety, and reflex control. However, given the marked multilevel supraspinal convergence of these pathways it is likely that this view is an over-simplification. For example, although vagal afferents synapse in the nucleus of the solitary tract (NTS) in the brainstem, this major integrative visceral sensory relay nucleus also receives inputs from spinal afferents as well as other brain regions. Subsequently, the principal projections from the NTS are to the parabrachial nucleus, within the pons, which receives further visceral sensory input from several spinal dorsal horn laminae. From the parabrachial nucleus, projections ascend toward higher structures including the hypothalamus, thalamus, insula, amygdala, prefrontal cortex (PFC) as well as many other cortical regions; see Fig. 16.1 for a schematic representation.
The thalamus is the largest structure in the dorsal portion of the brainstem and comprises multiple nuclei arranged into six groups in each thalamic hemisphere. Within these groups, nuclei can be broadly divided into two functional types: relay (specific) nuclei and diffuse projecting (nonspecific) nuclei. Relay nuclei convey information between subcortical and cortical regions and mediate perception, voluntary movement, emotion, and language. In contrast, diffuse projecting nuclei receive numerous converging sources of neural input, and project to numerous cortical regions.
Within the lateral portion of the thalamus, neurons in both the ventroposterolateral (VPL) and ventroposteromedial (VPM) respond to noxious sensations. The receptive field of VPL displays somatotropic organization, although visceral input into the VPL is not visceroptopic . Projections from the lateral thalamic nuclei are believed to mediate the sensory discriminatory aspects of pain perception. However, this viewpoint has been challenged with the proposition that this discriminatory function is arguably more attributable to the thalamic area that contributes to the posterior part of the ventromedial nucleus. Nuclei in the ventroposterior inferior (VPI) and medial part of the posterior complex contain nociceptive neurons that project toward the insula and secondary somatosensory cortex (S2). In humans, Lenz et al. showed in a single patient with a background history of angina that micro-stimulation of the VPL nucleus reproduced angina-like symptoms but also concomitant paresthesia in the leg, suggesting that the VPL has a role in both visceral and somatic sensation.
Studies have demonstrated that nuclei within the medial thalamus have large bilateral receptive fields. They do not directly contribute to the localization of pain but do encode its relative intensity, suggesting that they have a role in some aspects of sensory discrimination. The ventromedial nucleus contains nociceptive neurons which respond to noxious mechanical, heat, and cold stimuli. Albeit with relatively small receptive fields, these neurons are somatotopically organized and project primarily to the insular cortex as well as the primary somatosensory cortex (S1). In addition, projections from the medical thalamic nuclei also reach the PFC and the anterior cingulate cortex (ACC), areas well characterized as important in the processing cognitive and emotional aspects of pain. The ventromedial nucleus also receives input from the vagus-NTS-parabrachial pathway, which projects onwards toward cortical areas that receive inputs from lamina I neurons from the spinal dorsal horn. Lamina I neurons have been implicated in homeostatic regulation and indeed pain has been regarded by some as a “homeostatic emotion.” Interestingly the vagus nerve also serves a function similar to lamina I neurons in the neurophysiology of the GI tract, with the exception that it does not assist in the pure sensory encoding of noxious sensation. The vagus has inputs into the thalamic reticular nucleus which itself projects to other thalamic nuclei, influencing the synchronicity of thalamocortical projections and to the intralaminar nucleus of the thalamus, which has widespread projections to the striatum and cerebral cortex.
Overall, the thalamus plays a central integrating and relay role in the process of nociceptive and homeostatic information to higher centers of the brain. Moreover, it also interacts with descending pathways that modulate the autonomic nervous system and visceral sensation.
Although the thalamus extensively projects toward the cerebral cortex, until relatively recently the role of the cortex in pain processing has remained rather uncertain. However, by utilization of human functional neuroimaging, a wealth of evidence has been provided, illustrating that the cerebral cortex plays a central role in sensory-discriminative and affective components of the pain experience. These subsequent sections provide a summary of the role of the S1 and S2, as well as the insula and cingulate cortices.
In humans, lesions within S1 have been shown to result in hyperalgesia, hypoalgesia, and no difference in pain perception. However, this seemingly contradictory evidence may be partially explained by the relative size and location of the lesion, as nociceptive neurons are not uniformly distributed in S1. It should be noted that S1, which importantly includes the cortical sensory homunculus, predominantly processes nonnoxious external somatosensory information, such as pressure and warmth, and thus neurons that encode tactile sensation far outnumber their nociceptive counterparts. There are plentiful projections from S1 to the VPL and medial thalamic nuclei; these neurons are somatotopically organized and have limited receptive fields, with activity directly correlated with the intensity and duration of the noxious stimulation. Taken together, these data suggest that nociceptive neurons in S1 encode the sensory discriminatory aspects of pain.
S2 is located in the parietal operculum in the upper aspect of the Sylvian fissure. In contrast to tactile sensation, the processing of pain in S1 and S2 occurs concurrently. S2 receives bilateral input from the VPI thalamic nuclei, which have bilateral receptive fields. Projections from S2, via the insula, enter the limbic structures of the temporal lobe. S2 is considered to be involved in the recognition of stimulus type and the cognitive-evaluative aspects of the pain experience. Evidence from lesion studies demonstrate that disruption of S2 limits the ability to identify the nature of noxious stimuli such that subjects cannot differentiate between mechanical or heat pain.
The insula (or insular cortex) yields several complex roles in pain processing that are incompletely understood, but are postulated to include interoceptive awareness and emotion. The insula has two distinct regions. Firstly, the granular posterior insula processes tactile, auditory, and visual somatosensation. Secondly, the dysgranular anterior insula is involved in olfactory, gustatory, and viscero-autonomic functions. It receives projections from S2 and the posterior ventromedial (VMpo) nucleus of the thalamus, and has been shown to be activated by visceral stimuli. As mentioned, the insula receives input from S2 but also direct projections from nociceptors within the VPM of the medial thalamus. Nociceptive neurons within the insula have large receptive fields that respond to different modalities of sensory simulation but are particularly activated by noxious visceral stimuli. The insula is thought to integrate information from the thalamus and somatosensory cortices (both S1 and S2), relaying this to limbic regions. Indeed, the insula has been termed the visceral sensory cortex. Direct stimulation of the anterior insula produces sensations of nausea and fullness in contrast to the posterior insula, which produces somatic sensation including pain.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here