Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The concept of resource management is borrowed directly from the domain of aviation. It should be no surprise that we turned to other complex, dynamic systems such as aviation and nuclear power for useful parallels. These industries have directly addressed issues of optimal crisis management performance by the humans “in the loop.” In the case of military aviation, the need to optimize human performance systematically has been evident since before World War II and still exists. These efforts have been spurred by the need to recruit and train large numbers of pilots and by the pilots’ very cogent desire to stay alive in the air. Commercial aviation learned much from military aviation, and the last 30 years have seen intensified efforts to improve human performance issues among aircrews and air traffic controllers. For the nuclear power industry, it was largely the accident at Three Mile Island (and later the Chernobyl catastrophe) that demonstrated the importance of human factors in the safe performance of these reactors. For many years these industries have recognized that maximizing safety and productivity requires an understanding of individual and group cognitive psychology aimed at changing organizational structure, equipment design, operational protocols, and crew training.
For example, in 1979 a thorough analysis of 60 airline accidents, including data from cockpit voice and flight data recorders, disclosed lethal decision-making errors by individual crew members or inadequate teamwork by crews. These findings were confirmed in detailed simulator studies of flight crews. As a result of these investigations of crew performance, the aviation industry embraced a training philosophy originally called “cockpit resource management” (CRM)—later “crew resource management.” In the CRM approach, crews are instructed not only in the technical “nuts and bolts” of managing crises such as engine fires, but also in how to manage their individual and collective resources to work together optimally as a team.
There have been six generations of CRM in aviation, and CRM has now been adapted not only to health care (as described more fully in this chapter) but also to other diverse domains including maritime operations, spaceflight, and firefighting. Many issues concerning resource management in these various dynamic domains are not yet completely understood. More than 25 years of experience and study of the CRM approach in aviation, health care, and elsewhere has demonstrated that effective resource management is an important component of managing challenging situations. Successful conduct of an anesthetic depends on more than just having the requisite medical knowledge and technical skills. These must be translated into effective management of the situation . In this chapter we provide core concepts and a set of practical principles to guide you in improving or refreshing your case management skills. These principles should be useful for any anesthesia case, but they are particularly important in difficult or complex cases and in crisis situations.
Between 1989 and 1990 we first adapted aviation’s crew resource management to anesthesiology, naming our approach and course Anesthesia Crisis Resource Management (ACRM). We changed the term crew to crisis because the term crew is not as familiar to most health care personnel as the concept of crisis. The term crisis resource management (hereafter considered roughly synonymous with aviation’s crew resource management and using the same generic acronym of CRM) has been widely adopted within the health care community. This choice of terminology has unintentionally led to several misconceptions. One is that ACRM says nothing about how to prevent crises. Another misconception is that the ACRM principles apply only to patients who are already in a serious state and thus do not pertain to management in mildly abnormal or anomalous situations that have not deteriorated catastrophically. As will be seen shortly, anticipation and planning is a key element of ACRM that includes recognizing risks, preventing anomalies, optimizing safety in ordinary patient care, and handling early states of deterioration to prevent the development of a full-blown crisis.
Whether at an early stage or at the height of a crisis, ACRM encompasses the ability of the anesthesia professional to command and control all the resources at hand to execute the anesthesia as planned and respond to problems that arise. This is, in essence, the ability to translate the knowledge of what needs to be done into effective team activity in the complex and ill-structured real world of perioperative settings. In ACRM, the fundamental principles fall into two categories: decision-making components and team management components. In this chapter we will describe these principles in detail and offer practical advice about how to implement them in the real world ( Table 2-1 ).
| Cognitive Components of Dynamic Decision Making | Team Management Components |
|---|---|
| Know the environment | Call for help early enough to make a difference |
| Anticipate and plan | Designate leadership |
| Use all available information and cross check it | Establish role clarity |
| Allocate attention wisely | Distribute the workload |
| Mobilize resources | Communicate effectively |
| Use cognitive aids |
Your different work environments (e.g., OR, PACU, ICU, emergency department) contain many individuals, systems, and physical objects that you must coordinate to manage the patient optimally. Some resources are obvious, such as the anesthesia machine; others are not very obvious, such as use of the scrub nurse to perform manual ventilation during a major catastrophe. You or the rest of the team are very unlikely to identify all the relevant resources in the heat of the moment unless you have given them some serious thought beforehand. Resources can be categorized as self, OR personnel, equipment, cognitive aids, plans, systems, and other external resources. We discuss each of these in detail as follows.
Your professional knowledge and skills are your most important resource because they enable you to take direct action to protect the patient or to supervise the use of the other resources at your disposal. However, like all resources the self resource is neither omnipotent nor inexhaustible. Many factors will limit your ability to care for the patient optimally. As discussed in the previous chapter your attention is a scarce resource, and you must learn to use it wisely. A significant part of these principles of crisis management will address ways in which you can best divide your attention between the various tasks at hand and the various problems you face.
Remember, too, that as a human being your performance is not constant. It will vary both over the course of a day and from day to day, and it is affected by many performance-shaping factors such as fatigue, stress, illness, and medication. Fortunately, good anesthesia practice does not typically demand continuous peak human performance, but any case could call on more personal reserves than you have available.
Your personality and style of interaction with others is important in achieving the optimum use of yourself as a resource. As will be discussed more fully in this chapter ideal interactions blend respectful assertiveness and decisiveness with calm rational leadership and decision making. Your underlying temperament may be more or less easily adapted to this style.
The responsibility for providing good patient care is yours. You should be sensitive to any degradation of yourself as a resource, whether you detect it yourself or are told about it by others. You must respond appropriately to changes in your performance status; a patient should never suffer for your decision to “tough it out.” No one will thank you for going ahead with a case if you cannot do your job properly and a catastrophe then ensues.
What can you do if you find that your performance is lagging? Under some circumstances, if you are ill, sleep-deprived, or preoccupied with a personal matter, you may need to postpone the case or insist that someone replace you. The organizational structure of your practice should provide for such situations. If you are currently in training, think about this when you evaluate the practice opportunities available to you after graduation.
If your ability is less severely degraded, you may still need to mobilize additional resources to maintain adequate performance levels. You could, for example, ask a colleague to assist you with particularly difficult parts of a case, or you could alert the circulating nurse to be ready to help you more than usual. You might also set the alarm limits on your monitors more stringently than you otherwise would and raise their audio volume so that you can be alerted early to potential problems. For impairments linked to your overall level of arousal (such as fatigue or illness) there are specific countermeasures that you can take to raise your arousal level. These have been summarized in the literature and include things such as standing rather than sitting throughout the case, conversing with OR personnel, strategically using caffeine (before or during periods where high alertness is needed but not too close to an upcoming sleep period), or trying to obtain a short nap before beginning a case (which may be feasible unless the situation is truly emergent).
Your attitudes are an important component of your abilities. They can affect your performance just as strongly as physiologic performance-shaping factors. In addition, psychologists studying judgment in aviators have identified five attitude types as being particularly hazardous, and they have developed specific antidote thoughts for each hazardous attitude ( Table 2-2 ). Aviation psychologists instruct pilots to actually verbalize the antidote thought whenever they find themselves thinking in a hazardous way.
| Hazardous Attitude | Antidote |
|---|---|
| Antiauthority: “Don’t tell me what to do. The policies are for someone else.” | “Follow the rules. They are usually right.” |
| Impulsivity: “Do something quickly—anything!” | “Not so fast. Think first.” |
| Invulnerability: “It won’t happen to me. It’s just a routine case.” | “It could happen to me. Even ‘routine cases’ develop serious problems.” |
| Macho: “I’ll show you I can do it. I can intubate anybody.” | “Taking chances is foolish. Plan for failure.” |
| Resignation: “What’s the use? It’s out of my hands. It’s up to the surgeon.” | “I’m not helpless. I can make a difference. There is always something else to try that might help.” |
The invulnerability and macho attitudes are particularly hazardous for anesthesia professionals. The belief that a catastrophe “cannot happen to me,” and that your expert performance allows you to do anything, can make you cavalier about planning and executing patient care. It can alter your thresholds for believing abnormal data or for recognizing problems, thereby leading to the fixation error of “everything’s OK.”
Hazardous attitudes are compounded by production pressures (see Chapter 1 ) and by the lack of a culture of safety in the work unit or institution. The economic and social realities of practice can cause these pressures to become internalized by anesthesia professionals, who then develop hazardous attitudes they might otherwise have resisted. For example, the surgeon will no longer need to overtly push you to go ahead with a case that should be canceled if you have already altered your own approach to conform to the surgeon’s wishes. Of course, there may be valid reasons to proceed with a questionable case when medical urgency demands it. Under these conditions the usual protocols for elective case management must be adapted to seek the best outcome for the patient.
In the final analysis, you must ensure that the patient’s benefit is the primary criterion in such decisions, and you should establish a bottom line of safe planning, pre-use equipment checks, and patient preparation beyond which you will not be pushed. Even if surgeons, nurses, or administrators have pressured you to do things that you do not think are safe, they will not thank you if the patient suffers, nor will they come to your defense should litigation arise.
To simplify these decisions, many institutions have developed multidisciplinary written consensus guidelines on the preoperative preparation of patients that address the appropriate workup for patients with various medical conditions in different surgical urgency categories. This approach is analogous to preestablished “flight mission rules” used in spaceflight operations. “Flight mission rules are agreements among NASA management, flight crew personnel, flight operations personnel, and others on courses of action to take in non-nominal (abnormal) in-flight situations.” These are intended to encapsulate detailed objective analyses and to isolate decisions from the pressures of the “heat of the moment.” Centers that utilize preoperative evaluation clinics that apply such guidelines have reduced the number of day-of-surgery cancellations for medical causes while maintaining appropriate standards of patient safety.
The other members of the OR team are also important resources. The surgeon and anesthesia professional (and other team members) will all feel responsibility for the patient, but it is the surgery that actually provides definitive benefits to the patient. Anesthesia itself has no therapeutic benefit. From the viewpoint of the anesthesia professional, surgeons have other important roles. The surgeon may know the patient well and may be able to give you important information about underlying medical or surgical conditions that could not be obtained from the patient or from the chart. Most surgeons are also more capable than you are to perform certain important technical procedures that might be needed to manage a crisis.
Nursing and technical staff each has a duty to safeguard the patient by using their specialized knowledge and skills within their defined scope of practice. Effectively using them as resources, while not exceeding their limits, is essential to achieving good outcomes. As we shall see, every person in the OR can help you manage a complex situation.
The OR is a relatively unique team environment. Each discipline—anesthesia, nursing, surgery, etc.—may have multiple individuals in its “crew” (e.g., a primary surgeon plus one or more assistants, an attending anesthesiologist plus a nurse anesthetist or resident). The crews then come together to work as a “team.” There are rarely fixed crews or teams of personnel that always work together, but rather pools of individuals forming the crews and teams. Moreover, on different days even the same team may be working on vastly different sorts of cases. Depending on the size of the work unit, you may occasionally or regularly work with the same set of people. In other settings, such as working in a “locum tenens” position, or on a cardiac arrest response team (“code team”) you may have never met the other members of the team. Until the last decade health care has not placed much emphasis on attitudes of team orientation and cohesion, relying instead primarily on the ethos of individual clinical responsibility. The variability in team makeup places a premium on the ability of individuals to form a coherent team when the going gets tough, and it places a burden on you as a team leader to manage the team’s resources appropriately (see later section on Leadership and “Followership” ).
Your institution can also adopt mechanisms to help promote team orientation. As one example of such an approach, over the last 2 years the code team at one of our hospitals (VA Palo Alto Health Care System) has adopted twice-daily (8 am and 10 pm ) 5-minute code team briefings where all members gather in a convenient spot to introduce themselves, to review key aspects of code management, and to provide a heads-up on unstable patients whose condition could deteriorate to a cardiac arrest. Merely knowing who the other team members are that day has proven to be extremely valuable to improve team cohesion.
Although clinical observation and direct manipulation of the patient are important skills for anesthesia professionals, they are not enough for optimal practice. Anesthesia care in the industrial world requires considerable equipment, including gas delivery systems, ventilators, monitors, infusion pumps, and OR tables. Although errors in equipment use can directly cause harm to the patient, or can trigger accident sequences, the use of every piece of equipment to its best advantage will maximize your ability to obtain a good clinical outcome. In order to achieve this goal you must
ensure that the relevant routine equipment is present and is working properly
ensure that critical backup equipment is immediately available (e.g., a self-inflating bag for emergency ventilation), and
know how to operate each piece of equipment you use, including knowledge of its operating characteristics in both normal and abnormal circumstances
In commercial aviation, pilots are “type-rated” and can only fly aircraft of the type for which they are certified. For example, a captain type rated only for a Boeing 737 cannot act as pilot in command on a Boeing 747 regardless of the number of hours of total flying experience. Furthermore, aircrews receive extensive training in the operation of the aircraft’s systems. Our own experience as clinicians and teachers in real and simulated anesthetic cases suggests that many anesthesia professionals are not sufficiently knowledgeable in the operation of their equipment. These devices are the tools of the trade and knowing how to use them is just as important as, if not more important than, knowing about physiology and pharmacology. It is our responsibility as anesthesia professionals to acquire this knowledge and skill. The operation of many devices is not intuitive, and there are often hidden pitfalls in their operation that can lead to a failure to function properly. Although the human-factors engineering and anesthesia professions are attempting to address these difficulties, they will never be solved completely, which makes it important for you to be well versed in the individual operational features of your equipment.
The human factors literature demonstrates conclusively that cognitive functions such as memory and arithmetic calculation are fallible, even more so during periods of stress. A particular vulnerability exists for “prospective memory”—remembering in advance to do something that has been postponed. Pilots and professionals in all domains of intrinsic hazard make extensive use of a variety of written, electronic, or mechanical “cognitive aids” to help support thinking and execution of complex tasks. These aids relieve decision makers of having to memorize every piece of information that might be needed for all possible cases. Although a few written checklists and protocols have been widely used in health care for many years (e.g., the Malignant Hyperthermia Association of the United States protocol for treating malignant hyperthermia [MH]), cognitive aids until recently have not been prominent in anesthesia. Even the language frequently used in health care to describe such aids shows how little they are valued—they are sometimes called “cheat sheets” or “crutches,” and people apologize for “having to look it up.”
We have been long-time pioneering advocates of a completely different philosophy that encourages the use of cognitive aids as a sign of strength. The attitude toward cognitive aids may be changing. For example, working with this book’s authors in 2003, the National Center for Patient Safety of the Veterans Health Administration produced a set of cognitive aids on the recognition and management of 16 serious perioperative events printed on laminated sheets. A study of the use of the cognitive aids suggested that they were beneficial to VA anesthesia professionals. Other research by several authors of this book has demonstrated that (1) medical and technical performance is better during a simulated crisis (e.g., MH) when a cognitive aid is used, and (2) it can be very helpful to the anesthesia professional leading the team if there is a “reader” whose job is to read the relevant aid to the team and keep track of whether the relevant tasks have been performed. A group from Boston has published results from simulation testing of 12 “crisis checklists” demonstrating a substantial reduction in failure of adherence to critical steps in management when the checklists were used. , In 2014 multiple papers and editorials in a single issue of Anesthesia and Analgesia discussed a number of important issues about cognitive aids and their implementation.
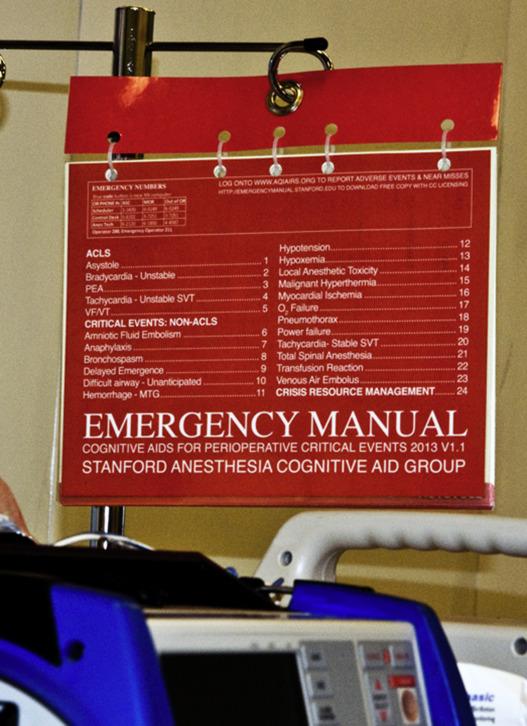
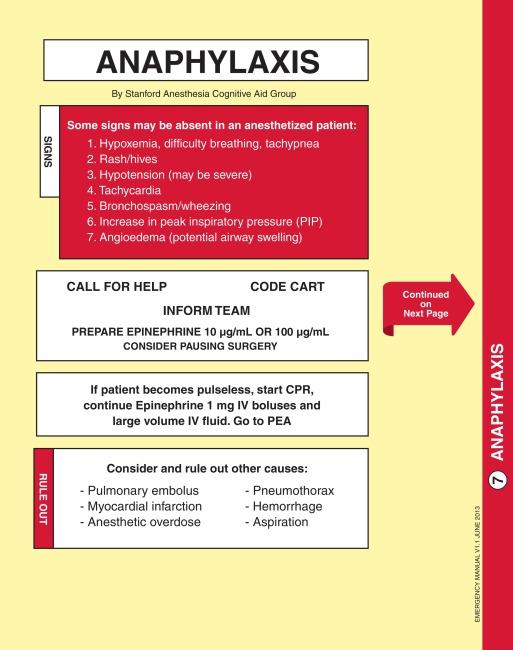
The Catalog of Critical Events in Anesthesiology ( Section II of this book) can be used as a cognitive aid during case management, but it has not been optimized for use as an emergency aid in the heat of the moment. The Stanford Anesthesia Cognitive Aid Group (SACAG), which includes two of this book’s authors as members, has conducted many years of simulation testing of cognitive aids meant for intraoperative use. These have evolved with increasing levels of optimization through enhanced graphic design and attention to usability. SACAG has now produced an Emergency Manual for Anesthesia, comprising 23 cognitive aids for perioperative events ( Figs. 2-1 and 2-2 ) (an earlier version of the cognitive aids was published as an Appendix in the textbook Manual of Clinical Anesthesiology ). These cognitive aids have been placed in all anesthetizing locations in the Stanford family of teaching hospitals. The manual is now available for free throughout the world as a downloadable portable document format file under a Creative Commons license (allowing free use of the document as is, without unauthorized modifications, and with attribution of the author). To download the manual go to http://emergencymanual.stanford.edu . Users can print out the manual locally, and instructions are given on best choices of printing paper, binding, and placement in perioperative patient care settings. The impetus to use cognitive aids has also been fostered by the widespread adoption of the World Health Organization (WHO) Safe Surgery (preoperative) Checklist (see http://www.who.int/patientsafety/safesurgery/en/ ) promulgated in part by noted patient safety advocate Atul Gawande, MD. The use of the WHO checklist, incorporating a preoperative timeout, has now become ubiquitous in the immediate preanesthesia process.
Mnemonics are another form of cognitive aid; they are learning techniques to assist in information retention and retrieval. They are often auditory in nature, such as an acronym or memorable phrase. For example, a phrase to remember the names of the carpal bones is “some lovers try positions that they can’t handle.” A frequently used mnemonic for preoperative anesthesia workspace preparation is MS MAID (monitors, suction, machine check, airway equipment, IV equipment, drugs). Another example is the mnemonic checklist THRIVE for preparation for weaning from cardiopulmonary bypass (CPB), developed by one of this book’s authors after he witnessed and heard about “near-miss” cases in which key items (such as ventilation) were omitted:
T emperature is acceptable.
H emodynamics and cardiac function are acceptable.
R hythm is acceptable.
I nfusions are selected as desired and are infusing properly.
V entilation is taking place at the rate and volume desired.
E lectrolytes are acceptable.
Although other personnel (including the surgeon) can provide important cognitive support, their memory is also fallible. It is probably better to use a written aid or call the hospital pharmacist to determine how to mix and dose a drug that is rarely used rather than rely solely on your memory or the memory of someone else who is not completely familiar with the medication.
Reference works and handbooks contain a wealth of useful information on the medical and anesthetic management of virtually every type of condition. Many anesthesia professionals also use written tables and lists that contain information on the preparation of drug infusions and their appropriate dose ranges. By law, each drug approved by the U.S. Food and Drug Administration (FDA) comes with a package insert containing extensive information on the drug’s characteristics. These are compiled in widely available references and are also available on the internet. The internet has become an increasingly useful cognitive aid and may be available on computer terminals, tablets, and smartphones in hospital settings. The medical literature can be queried directly via PubMed ( www.pubmed.gov ) and there are a variety of open or proprietary sites with well-researched evidence-based summaries of best practice. Accessing internet-based resources in the middle of a case is a two-edged sword. Useful information may be acquired but at the cost of significant distraction and increase in mental workload. If extensive interaction with a computer is needed it is probably best to have someone else assist you.
Bedside use of aids embedded on tablet computers and smartphones is also becoming more common. In addition, these devices bring mathematical calculators immediately to hand for anesthesia professionals. Under stress the ability to perform calculations—even simple addition or multiplication—degrades quickly. We encourage you to use a calculator to compute drug doses (especially for unfamiliar drugs or patient weights) rather than to rely only on memory or on-the-spot mental arithmetic. Of course people make errors with calculators too, so the results of any calculation also need to be checked for sensibility by the anesthesia professional.
The patient’s medical record is a key source of information that contains the current and past medical history as well as the results of laboratory and radiologic tests. The advent of electronic medical records has made it possible to access data for patients in your system more expeditiously. Your anesthetic record is another important source of information, especially if you have not been present for the entire case. Always double-check your recollection of important data with the written source. Additional case information may also be obtained from the data stored as trends within the monitoring equipment in use.
We encourage you to seek out cognitive aids of all types and to use them whenever possible. Obviously there are some limits to this—you cannot be an effective anesthesia professional if you have to look up everything. But our experience, in real patient care and in simulated cases, shows that even when the aids are available their value is underestimated. Where cognitive aids have not been published formally, we encourage you to develop and produce them for yourself, in concert with others in your practice, or through professional societies.
In most sites in which surgery is performed (hospitals and stand-alone outpatient surgery centers) the OR is a subsystem linked to other systems. Thus there may be many external resources available to assist you in preventing or managing adverse events. For example, such system resources include preoperative assessment clinics, postoperative care units, laboratory services, blood bank, radiology, consulting physicians (most commonly cardiologists and neurologists used for crisis management), engineers, risk managers, and administrators. Experience shows that the best use of systems resources is difficult, and in fact the interface between systems can itself be a source of errors. You must consider in advance how you will mobilize and utilize these resources and communicate with them. Knowing where the key sites (such as the blood bank) are physically located as well as their phone numbers will help; this is information that lends itself to cognitive aids posted in clinical work areas. If you work in more isolated locations, such as a surgeon’s private office, you are responsible for knowing what resources are available and what plans exist should a problem develop, making it necessary to obtain help or transfer a patient to a higher level of care.
Regional and national resources also exist. A good example is the MH hotline in the United States (1 800 MH HYPER), which can provide expert advice in the management of patients with suspected MH susceptibility or with full-blown MH. Keep in mind, however, that contacting the hotline should not interfere with carrying out critical tasks of patient management. If extra personnel are available, one person can be delegated to contact the hotline.
There is also telephone or online technical support offered by poison control centers and by many manufacturers of drugs and medical devices. Such contact information should be available on the internet. For example, such technical support has been especially helpful in the management of patients with cardiac pacemakers or implanted defibrillators.
Resources can be mobilized and used “on the fly,” but the best use of resources requires advance planning. The plans themselves become key resources because they enable you to manipulate the situation more quickly. Appropriate plans come in three forms: A work environment plan for resource mobilization in a specific work setting; an anesthetic plan for dealing with the particular problems of a specific patient; and emergency procedures for the management of critical incidents. A good program of quality management or quality improvement is of enormous value to all forms of planning. It is the mechanism by which knowledge of past adverse events can be translated into changes in practice that minimize their recurrence.
Work environment plans should incorporate a detailed knowledge of each environment in which you care for patients, whether it is an OR, a PACU, or a remote setting such as a magnetic resonance imaging (MRI) suite. The equipment and external resources available in each setting may differ, and you will not be able to use them effectively unless you plan in advance. It sounds obvious, but our experience shows that clinicians often fail to know what they have available, where it is, and how to use it. Know the contents of your anesthesia carts, including emergency use items such as flashlights, resuscitation drugs, and pressure infusion sets. Know the location and operating characteristics of emergency equipment. Learn to operate the available defibrillators and to troubleshoot minor problems. Know what other equipment exists and where it is located, such as spare O 2 cylinders and regulators (and become familiar with changing cylinders and regulators), MH carts, difficult airway equipment, fire extinguishers, and battery-powered monitors. Think about the location of critical external resources such as satellite laboratories or pharmacy stations so that you can instruct runners how to get back and forth. Know how to call for help and how to call a “code” in the event of a cardiac arrest or other major emergency. Every facility has its own procedures and code alert language (e.g., “code blue” for a cardiac arrest, “code red” for a fire, “code silver” for an active shooter). Find out who will respond to a code both day and night. If you are not sure who to contact, call the facility’s telephone operator (usually dial 0). If you are not in a hospital or other all-hours facility, you may need to call outside the institution for help, for example dialing 911 (in the United States) to reach the dispatcher for paramedic, police, and fire departments.
Preoperative evaluation of the patient and construction of a suitable anesthetic plan is an important task that you perform to prevent the occurrence of events that can evolve into adverse outcomes. The plan delineates how you will conduct the anesthetic, how you will deal with the problems you are likely to face, and what other resources you must mobilize to meet the anesthetic goals for the case. A sound plan matches the anesthetic technique to the patient’s disease state, the technical requirements of surgery (e.g., position of the patient), the anesthesia equipment available, and the skills of the anesthesia professional. It also includes specific backup procedures and contingency plans to be used if the original plan fails or needs to be changed. Often, faulty plans occur when underlying disease states are missed or ignored because of inadequate data gathering during preoperative evaluation. Poor planning may also result from the invulnerability type of hazardous attitude. A faulty anesthetic plan will expose the patient to risk even if it is carried out perfectly .
Systematically prepared emergency procedures are used in virtually all complex dynamic work environments, not because the operators are ignorant or stupid, but because experience has shown that even well-trained, intelligent people need decision-making support during rapidly changing problem situations. Every licensed pilot (including the purely recreational pilot) is taught specific emergency procedures for a variety of contingencies. In the case of large commercial aircraft the emergency procedure manuals are quite extensive. Pilots are expected to memorize certain critical portions of each procedure and then to rely on the manual (and not on their memory) for the rest of the procedure. Airline pilots practice these procedures regularly during simulator-based recurrent training programs.
The situation in medicine in general (including anesthesiology) has been considerably different. Responses were described in a formal fashion for only a few extremely severe events (e.g., CPR, MH). For the most part, anesthesia professionals were expected to learn responses to adverse events solely by experiencing them. Each teaching anesthesia professional may have a favorite “clinical pearl” concerning emergency responses to hand down to trainees, but few pass these on consistently. For most practitioners serious adverse events are uncommon, and even those responses that were once second nature are soon forgotten for lack of use. It is for this reason that we created the Catalog of Critical Events in Anesthesiology for this volume and the Anesthesia Emergency Manual (see earlier section on Cognitive Aids ).
For planning to be most effective it should ensure the coordination of all members of the patient care team. This begins with greeting the patient (the most important member of the team) just prior to surgery. In addition to identifying the patient and surgical site properly, this meeting allows further clarification of the plan.
It is important to ensure that all members of the anesthesia crew and the rest of the OR team (surgeons, nurses, technicians) agree with and understand the plan. Aspects of the surgical procedure, such as the desired patient position and the extent of planned dissection, may alter the plan; if these are not clearly defined on the surgical schedule, the surgeons must be consulted. If predictable problems might necessitate changing plans or aborting the procedure, this should be specifically discussed in advance with the surgical team.
Over the last 10 years there has been a major movement to formalize such briefings. The WHO began a “Safe Surgery Saves Lives” campaign, creating a preoperative checklist to be used in a mandatory preoperative briefing involving surgeons, anesthesia professionals, nurses, and others. In these briefings an important element is to define likely critical events and patient specific considerations. This is an opportunity to delineate contingency plans and who will determine when to switch from the initial plan to a backup one.
Handoffs from one anesthesia professional to another, or from the anesthesia professional to the PACU staff, are also important times for a different kind of formal briefing. There is considerable research ongoing about handoffs of many kinds in health care. Although many different protocols have been suggested, none has proven to be ideal. This puts the burden on you to determine the best mechanism to conduct such briefings. The less formal and very rapid kind of briefing that is needed when a helper arrives in a crisis is discussed more fully later in this chapter.
The discussion of resources should help you prepare to provide good anesthesia care at any time. We now turn to the question of how to act optimally during intraoperative patient management. Every strategy that you might choose is a two-edged sword, ideal for some situations but inadequate for others. Optimal care therefore requires constantly balancing and adapting your behavior to the changing situation.
We have stressed the need to anticipate the requirements of a case in advance. One aspect of this is to have a high index of suspicion for the medical problems that you might expect to encounter because of a patient’s underlying diseases. You should look for these and make preparations to treat them. However, the risk of this strategy is that other problems that mimic the one you expect may in fact occur. It is important to keep an open mind and to make sure that you consider other possibilities (see discussion of reevaluation in the section titled Repeatedly Assess and Reevaluate the Situation ).
Throughout the case you need to maintain awareness of every change that occurs in your environment. As mentioned in Chapter 1 pilots call this “situation awareness.” The goal is to “stay ahead of the game.” You can easily fall behind if the situation changes radically or quickly or if you fail to devote sufficient resources to meet the changes. When you find yourself getting seriously behind the events of a case, regardless of the reason, you must either slow down the progress of the case (e.g., ask the surgeon to hold off from significant actions while you catch up) or mobilize additional resources (see Call for Help—Early Enough to Make a Difference ) so that you can catch up and get ahead. Staying behind for any prolonged period exposes the patient to risk.
Vigilant observation of the patient is the necessary (although insufficient) starting point for expert case management. In discussing the self-resource, we mentioned several performance-shaping factors and hazardous attitudes that can globally degrade your vigilance. There are two other factors that can specifically degrade your vigilance whenever they exist in a case: one is distractions , the other is a high task load .
Distractions of various kinds occur during every case. They include activities that are important to other OR personnel, such as surgeons taking photographs, nurses counting surgical instruments or entering data in the computer, or phone calls from the ICU asking for the surgeon’s instructions on a patient’s care. Your attention to the patient can suffer if you assist in these activities. For example, if there is a phone at the anesthesia workstation, it should not be used routinely for phone calls that are not important to you. Nurses or clerks can transcribe laboratory results or relay messages between the surgeons and the ICU.
Routine tasks can be very distracting. The use of transesophageal echocardiography has been shown to alter the vigilance of anesthesiologists to the occurrence of secondary tasks. Rotating the operating table (especially 180 degrees) or repositioning the patient on the table (e.g., prone or lateral) is also a high workload distracting activity. Increasingly, anesthesiologists interact with patient data management systems. As pilots have discovered, spending too much time “heads down” at the computer can reduce vigilance for key events in the “cockpit.”
Distractions can also include music, social conversation, and jokes. Each of these activities is appropriate under the right circumstances. They can make the work environment more pleasant and promote the development of team spirit, but they can also seriously lessen your ability to detect and correct problems. You must take charge of modulating these activities so that they do not become distracting. If the music is too loud, insist that the volume be reduced or that it be turned off (a rule of thumb is that the pulse oximeter volume should always be louder than the music or conversation). When a crisis occurs, all distractions should be eliminated or reduced as much as possible.
Tenney and colleagues have described how interruptions and distractions are prime contributors to the evolution of small problems into major catastrophes. Distractions are problematic because of a known human weakness in “prospective memory”—remembering in advance to do something. These “remembered intentions” are particularly prone to disruption by distractions and interruptions. Besides modulating potential distractions, other strategies can help to reduce the likelihood of forgetting a task because of interruptions or distractions (an error of prospective memory). Take the example of being interrupted when you have turned off the ventilator for an appropriate reason. There are various strategies to deal with this. Some anesthesia professionals leave their finger on the ventilator switch. Other strategies include putting a small sign on the ventilator to remind you that it is off, or executing a checklist periodically after turning off the ventilator to ensure it has been turned on again when appropriate (see THRIVE example previously mentioned). As a last resort in this example, properly set alarms should warn you of apnea should you forget to turn the ventilator back on.
Allocation of attention is a dynamic process through which you must constantly prioritize the tasks requiring your attention. You should handle critical items quickly and leave the less critical problems for when you have ensured the stability of the patient. On the other hand, you should deal with minor problems when the task load is low because they might otherwise evolve to something more significant. You can also use times when the workload is low to prepare for upcoming high workload periods, such as emergence from anesthesia or termination of CPB.
It is important to maintain vigilant assessment of the patient even while you continue to carry out a myriad of routine tasks and interact with students, teachers, subordinates, or supervisors. If you suspect that a problem is developing, allocate your attention primarily to problem recognition and patient evaluation until you prove to yourself that all is well. Whatever tasks occupy the OR team, at least one individual should be watching the patient’s condition at all times. The task load can quickly become excessive, making you so busy that it will be impossible to maintain vigilant situational awareness. If you find yourself in this situation, you must mobilize additional resources to help you carry out the needed tasks and watch the patient. A frightening example from aviation that has proved compelling in the training of anesthesia professionals is that of the airliner (Eastern 401) that crashed because all of the cockpit crew were preoccupied with a faulty indicator light for nose gear deployment. The crew failed to notice that the autopilot had become disengaged—in other words, no one was flying the plane (a web search will show multiple sources for information about the details of this flight).
No single piece of information tells the whole story. Considerable controversy has been generated since the early 1970s concerning the relative merits of direct clinical observation versus the use of electronic and mechanical monitoring devices. This is a false dichotomy; neither clinical observation nor any single monitor currently in use gives the entire picture. The goal is to utilize all the information at hand to help you care for the patient. The challenge is to learn how to integrate data from every possible source, giving each datum its appropriate weight toward a decision.
Similarly, it is important to pay attention to the patient care activities of surgeons and nurses. Be very aware of the medications drawn up on the surgical field. A number of catastrophes have resulted from errors in dilution or administration of such drugs. If something unusual appears to be happening with the surgery, insist on finding out what is going on. Comments and concerns of other team members may not be addressed to you but may give early warning of an impending problem or provide critical information on how the problem can or cannot be solved.
Every type of observation has possible artifacts. Alarms from electronic monitors often occur repeatedly but falsely. A “cry wolf” syndrome can develop in which the anesthesia professional assumes that an alarm is false, even when it is really true. Alarm sounds are typically distracting, and they seem to trigger a “make it stop” response in anesthesia professionals, whose first (and sometimes only) move is to turn off the alarm. This assumption can lead to catastrophe for the patient. When a monitor alarm sounds or when a question of patient safety is raised by your own observations or those of others, the burden of proof is on you to first determine that the patient is safe, and then to deal with any technical problems. Your evaluation of the patient can include checking alternate electronic monitors, but you should always remember to check the patient and equipment using all your senses, including your eyes (visual inspection), ears (auscultation), and touch (feeling the pulse). Some anesthesia professionals describe their overall practice style as always assuming that the patient might be in trouble, and then continuously proving to themselves that the patient is really safe.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here