Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Interdisciplinary care of patients with chronic pain has proven to be of significant value.
A collaborative relationship between patients and rehabilitation professionals is essential to enhance successful outcomes.
The pain management treatment plan must be tailored to the individual patient.
Establishing treatment goals, patient education, therapeutic exercise, and behavioral techniques are at the core of rehabilitation management.
Active involvement of patients and treatment adherence are necessary.
Ideally, patients with pain related disability resulting from chronic pain are treated by an interdisciplinary team of health professionals, commonly consisting of physicians, psychologists, physical and occupational therapists, social workers, and nurses, to address the biopsychosocial nature of pain. Interdisciplinary treatment is defined as multimodal treatment provided by a multi-disciplinary team collaborating in assessment and treatment using a shared biopsychosocial model and goals. For example, the prescription of an anti-depressant by a physician alongside exercise treatment from a physiotherapist, and cognitive behavior treatment by a psychologist, all working closely together with regular team meetings (face to face or online), agreement on the diagnosis, therapeutic aims, and plans for treatment and review. Rehabilitation specialists working in pain management settings appreciate the complexities of chronic (vs. acute) pain, i.e. unclear relationships between pain, impairments, and disability, and the need to address the behavioral, emotional, and cognitive aspects of chronic pain. Chronic pain is understood as a disease, a pathology of the nervous system that produces abnormal changes in the brain and spinal cord and not as a symptom or warning of tissue damage.
Patients come to our pain management programs with certain expectations for evaluation and treatment. Although several studies investigated the expectations of patients with chronic pain of their physicians in a pain management program, there is a paucity of patients’ expectations of their rehabilitation specialists. Most patients expected an explanation or an improved understanding of their pain problem (pain education), pain relief, and a definitive diagnosis from physicians. , Many patients with chronic pain resist referral to physical rehabilitation. Part of the difficulty lies in the history of treatment failures with which patients often present. Several factors may be responsible for past treatment failures, including persistent failure of health professionals (physicians, physical and occupational therapists) to recognize and treat the differences between acute and chronic pain states, past treatment that did not address the emotional and cognitive aspects of chronic pain, and an inability of the patient to recognize anything less than total pain relief as success. Therefore it is crucial to identify patient expectations at the initial visit to prevent disappointment with referrals to physical rehabilitation for pain management.
In evidence based practice, clinical decisions must include consideration of, first, the patient’s clinical and physical circumstances to establish what is “wrong” and what treatment options are available to address this problem. Second, the latter needs to be tempered by research evidence concerning the treatment options’ efficacy, effectiveness, and efficiency. Third, given the likely consequences associated with each option, the clinician must consider the patient’s preferences and likely actions (in terms of what interventions she or he is ready and able to accept). Clinical expertise is needed to bring these considerations together and recommend a treatment that the patient agrees to accept. The purposes of a rehabilitation specialist evaluation are to establish a baseline from which to plan and begin interventions, help to select appropriate interventions, and evaluate the efficacy of interventions.
As described in the biopsychosocial model of pain introduced by Fordyce, contributing factors to disability can be biologic, psychological, as well as social. Essential in this model is the idea that factors maintaining the pain problem are not necessarily the same as those initiating pain. Therefore to establish a baseline, a thorough inventory of all factors contributing to a patient’s perceived level of disability is important. The International Classification of Functioning, Disability and Health (ICF) provides a biopsychosocial model that identifies three concepts described from the perspective of body systems, the individual, and society. Within the context of health, the ICF defined bodily functions and structures as physiologic functions of body systems or anatomic elements, such as organs, limbs, and their components. Second, activity is defined as the execution of specific tasks or actions by an individual, whereas participation is envisioned as encompassing involvement in a life situation. In the ICF, functioning refers to all body functions, activities, and participation. Disability is the ICF umbrella term for impairment, activity limitation, and participation restrictions. Contextual factors are provided within the ICF framework ( Fig. 60.1 ), consisting of external environmental factors (such as significant others, employers, medications, and healthcare providers) and personal factors (such as age, education, income, worry that activity will exacerbate pain or injury resulting in avoidance of activity to prevent anticipated negative consequences).
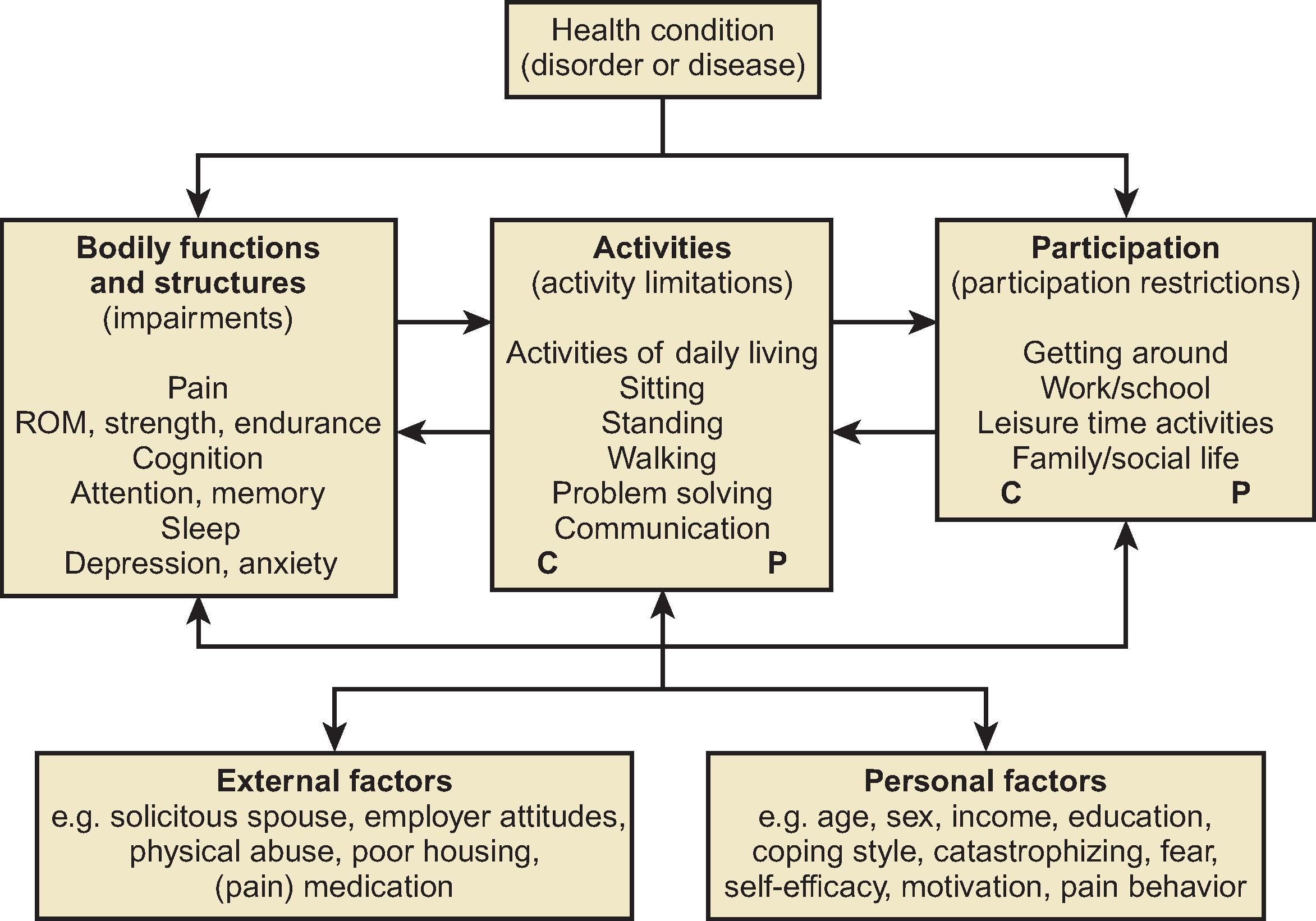
Qualifiers for the activities and participation classification make it possible to clearly separate the patient’s inherent capacity to perform actions within a domain and performance in his or her actual environmental context. Capacity refers to the environmentally adjusted inherent ability of the individual or, in other words, the highest probable functioning of a person in a given domain at a given point in time, in a standardized environment. Capacity can be measured by physical tests or by questionnaires that ask, “Can you?” Performance describes what a person actually does in her or his current environment and thus describes the person’s functioning as observed or reported in the person’s real-life environment with the existing facilitators and barriers. Performance can be measured by direct observation. However, as visual observation is often highly impractical, self-report measures can be substituted that ask, “Do you?” Increasingly accelerometers are being used to get some objective sense of a person’s activity and sedentary level.
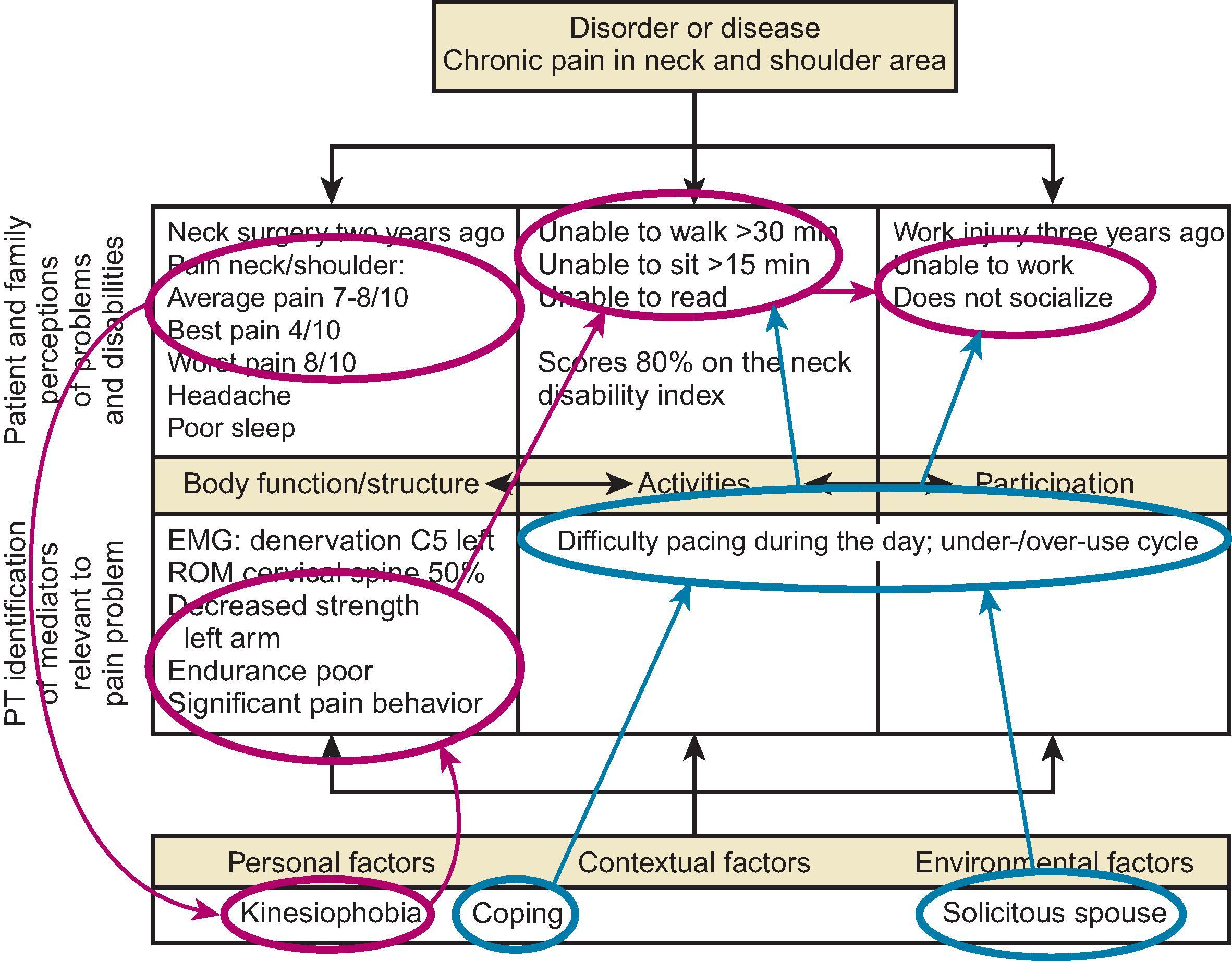
The rehabilitation problem solving (RPS) form is based on the ICF and is a practical tool to use to visualize the patient’s state of functioning and disability. The form is used to specify precise and relevant target problems, discern factors that cause or contribute to these problems, and plan the most appropriate intervention. In addition, the form was designed as a tool to facilitate both intra- and interprofessional communications and improve the communication between healthcare professionals and their patients. The form is divided into three parts: (1) the header provides basic information, (2) the upper part is used to describe the patient’s perspective, and (3) the lower part is used for the analysis of the healthcare professionals.
The form can visualize the current understanding of the patient’s state of activities and participation, his or her target problems, and how the healthcare team relates them to hypothetical mediators and contextual factors ( Fig. 60.2 ).
From the information obtained through carefully selected questionnaires, an interview, the physical examination, and physical tests, most of the information needed to develop an appropriate treatment plan should be obtained.
The Joint Commission on Accreditation of Healthcare Organizations requires that all patients have the right to an adequate pain assessment, including documentation of pain location, intensity, quality, onset/duration/variations/rhythms, manner of expressing pain, pain relief, what makes it worse, effects of pain, and a pain plan. Besides questions about the location, intensity, frequency, and duration of pain, questions such as “What do you think causes your pain?” and “What is the worst thing you think might happen to you because of your pain?” will give insight into the patient’s belief system—especially important if the patient comes from a different culture—and the presence of catastrophizing. In addition, rehabilitation specialists focus on determining how much the pain interferes with activities and participation: activities of daily living such as housework, grocery shopping, and getting around in the community; recreational and social activities; and the ability to do work and sleep. For example, the number of hours lying down and changes in activity level because of pain during a day is noted. Patients are further asked about significant others, partners, parents, and children; do they help out, ignore the patient, or prevent them from doing things as they fear the patient might “harm” him- or herself.
Unfortunately, there are no perfect measures of physical activity or activity limitations. Comparison measures include both “subjective” measures (based on self-report) and “objective” measures (based on direct measurement). Self-report measures can be self-administered or interviewer administered, both in person and on the telephone. However, self-report of physical activity can reflect a difference between how active patients really are and how active they perceive they are, resulting in a difference between self-reported physical activity level and the actually observed active behavior. Studies, including self-report and objective measures on activity and activity-related disability, indicated a gap between self-report and objective measurement. In rehabilitation practice, there is a tendency to use objective and self-report measures to assess physical activity. Objective measures include functional capacity tasks, markers of movement (accelerometers, registration of activity by smartphone, or activity monitors), and observed or videotaped activity (direct observation). Self-reported status often involves outcomes of most relevance and importance to patients and their loved ones because they capture patient experience and perspective. Rehabilitation professionals should know these differences during their assessment. Besides assessing a patient’s level of activity, labeling a patient’s activity-related behavior style seems of additional value when choosing the most appropriate ingredients for treatment: Will this patient avoid activities because of pain (avoider), or will he or she persist in the performance of activities regardless of pain (persister)?
Psychosocial factors have been found to have a significant impact on perceived disability, particularly among persons with chronic pain. The rehabilitation professional’s observations of a patient’s behavior during the interview or functional testing as a part of a screening procedure can deliver valuable information and should be communicated clearly to the rest of the team, which can then direct appropriate psychological and psychiatric treatment. Psychological screening by rehabilitation professionals with history taking has been shown to have low sensitivity and predictive value for identifying distressed patients. Thus formal screening of some sort, such as with a questionnaire, is recommended. Psychosocial factors contributing to a patient’s disability level that can be assessed by a questionnaire are, for instance, fear of movement (Tampa Scale of Kinesiophobia), catastrophizing (pain catastrophizing scale ), and depression (the Beck depression inventory). High pain catastrophizing has also been found to be a predictor for patient dropout during treatment. As previously mentioned, particularly important are questions about what the patient expects from treatment. Patients’ beliefs and expectations play a large role in treatment participation and eventual treatment outcome. Studies have shown that high patient expectations may positively influence clinical outcomes independent of the treatment itself. Treatment of chronic pain is often complex and may be further complicated when patients and healthcare providers have differing goals and attitudes concerning treatment. Difficulties in engaging in collaborative treatment decision making may result. A negative expectation on treatment outcome can influence treatment compliance. For instance, a patient who is looking for pain relief only and insists on medication management as the sole treatment for the pain is not likely going to comply with a rehabilitation program. Efforts to enhance patient-provider communication as well as to systematically examine non-specific treatment factors are likely to promote effective management of chronic pain. This includes adapting health information to the level of patients’ health literacy by not using medical jargon, not delivering too much information at a time, and confirming patients’ understanding of what was discussed by using teach back techniques. Unfortunately, despite the widespread recommendations to medical practitioners to check patients’ understanding directly, it does not yet appear to be routine practice.
The traditional rehabilitation-oriented physical examination assesses impairments in joint range of motion (ROM), strength, neurologic integrity, and gait. Diagnostic procedures should focus on identifying potentially serious “red flag” conditions that require prompt medical evaluation. The main objective is to determine whether there is a relationship between pain reports and objective physical findings or whether the patient presents with chronic primary pain or chronic secondary pain. In the former, rehabilitation might focus on improving physical functioning in general and have a more significant behavioral approach. In contrast, in the latter case, rehabilitation might focus more specifically on impairments related to pain that interfere with the ability to function.
Patient anxiety may complicate the physical examination. Catastrophic cognitions, behavioral displays of pain, and somatic sensations measured during examination have been shown to uniquely predict anxiety experienced during examination. Muscle guarding and pain behaviors are often displayed during physical examination and include moaning, sighing, rubbing, reluctance to perform any active movement (ROM), and the presence of giveaway weakness and non-physiologic signs. Waddell’s non-physiologic or behavioral signs in patients with back pain can be assessed through palpation and simulation tests, including axial loading (pressure applied to the top of the patient’s head), simulated rotation (moving shoulders and hips together so that no rotation occurs in the trunk), inconsistency between the straight leg raise in a sitting versus supine position, giveaway weakness with resisted muscle testing, and regional sensory change. Several studies examined the cross-sectional construct validity of the Waddell score and found evidence that it measures a combination of pain intensity, illness behavior, physical dysfunction, and psychological functioning, somatic over-reporting, increased perceived disability, and pervasive pain interference. Recognizing that studies in patients with chronic pain have identified discrepancies between self-report of physical activity and actual level of physical activity, capacity testing is performed in addition to traditional impairment examination. This involves direct observation of patient performance on specific tasks and assessment of whether the patient is willing to move or fears performing specific tasks. Baseline functional ability assessment can provide objectively verifiable information about a patient’s quality of life and ability to participate in normal life activities.
Functional tests can be used to focus on performance in basic daily life activities, such as walking, stair climbing, and lifting. Various specific tasks or sets of tests that intend to represent daily functioning are available for this purpose. Simple tasks such as 5 min walking, 50 foot walking, sit-to-stand, 1 min stair climbing, loaded forward reach, or various lifting tasks are available to test a patient’s capacity during one specific activity. However, the ability of the tests to reflect the level of functioning in patients with pain has to be taken with caution. The test-retest reliability and responsiveness appeared to be only moderate for most of the tests. In addition to single tests, test batteries have been introduced to represent functioning in patients with pain. For example, the Back performance scale is a condition-specific performance measure of activity limitation in patients with back pain and includes five tests of daily activities requiring mobility of the trunk: sock test, pickup test, rollup test, fingertip-to-floor test, and lift test. The psychometric properties of this test battery have been demonstrated. , A second example is a generic test battery that includes nine physical performance tests: the time taken to complete various tasks (e.g. picking up coins, tying a belt, reaching up, putting on a sock, standing from sitting, a 50 foot fast walk, a 50 foot walk at preferred speed), the distance walked in 6 min, and the distance reached forward while standing. The reliability and discriminant ability of this battery has been confirmed.
In the assessment of work related performance, a functional capacity evaluation (FCE) is often used. , An FCE is an evaluation of the capacity of activities that are used to make recommendations for participation in work while considering the person’s body functions and structures, environmental factors, personal factors, and health status. The purpose of an FCE is to test a person’s physical abilities to the maximum to produce objective documentation regarding work and activities of daily life. The FCE has become part of the accepted practice in work injury prevention and rehabilitation. , During an FCE, the patient has to complete a standard protocol of physical tasks while a trained observer records the capacity and limitations. Assessment includes the ability to lift weights from the floor to waist and from waist to overhead, carry, crawl, squat, sit, stand, walk, climb stairs, and push and pull weights. Aerobic capacity may be determined from a maximal bicycle or treadmill test. Additional specific tests may be performed, such as those used to evaluate fine motor skills for the hands and handgrip strength. Practical data on the use of FCEs to determine an individual’s physical capacities have been available since the early 2000s, and normative data have now been established. Biopsychosocial factors may influence functional test and FCE test results, although it is unclear to what extent and which factors are important. A systematic review concluded that there is conflicting evidence for the influence of psychological factors and absence of evidence for the influence of social and biologic/physiologic factors in patients with non-specific chronic low back pain (CLBP) that influence capacity test results. Therefore interpretation of FCE test results is not entirely objective because the observer has to decide if a patient performed maximally or submaximally during the test. In addition, pain and pain related constructs have been shown to negatively influence FCE performance levels. FCE should thus not be considered a purely “objective” indicator of functional impairment independent of subject or evaluator perceptions.
Several studies have shown that self-report and performance and capacity tests, although related, appear to tap into different aspects of the physical functioning domain. For instance, patients with CLBP showed considerable differences in limitations when comparing self-report, clinical examination, and functional testing for assessing work related limitations. Professional healthcare workers should be aware of these differences when using them in daily practice. ,
An important difference between patients with acute pain and those with chronic pain is the variation in relationships between pain, activity limitations, and participation restrictions. For patients with acute pain, nociception, perceived pain, activity limitations, and participation restrictions often have a close relationship. Therefore treatment in the acute phase focuses on eliminating the causal factor of the pain, resulting in a reduction of activity limitations and the prevention of disability. However, for patients with chronic pain, this treatment strategy is often insufficient. Patients with chronic pain may never return to work even when the only impairment identified is pain. Treatments that address chronic pain as a warning of tissue damage, like in acute pain, do not alter the illness and disability behavior of patients with chronic pain, nor will they improve their health-related quality of life. The focus of therapy should be to help these patients regain control over their lives by active participation in their pain management program and learning to cope with pain. To achieve this goal, an active partnership is needed between the patient and the rehabilitation professional. Like other patients, patients with chronic pain want a confidence-based association that includes understanding, listening, respect, and being included in decision making. The input from the interview and patient assessment form the basis of shared decision making, which involves at least two participants who engage in a process of both mutual information and interactive discussion. Patient participation should result in a greater sense of personal control, more satisfaction with treatment, better compliance, and transfer into the daily routine of disease management and, consequently, better outcomes.
Patients with chronic pain are not a homogeneous group, and there is no magic bullet that fits all. Because each patient has a unique set of circumstances, psychosocial issues, and physical findings, treatment is individualized and based on the comprehensive assessment of the patient and the patient’s individual goals.
Chronic pain management should include:
collaboration between the rehabilitation professional and the patient
a personalized rehabilitation plan
tailored education of the patient on the nature of the problem
resolution of treatable barriers related to functional goal attainment
tailored instruction in independent management of pain
instruction in methods to prevent future problems
monitoring of outcome (achievement of patient goals)
monitoring of adherence to treatment
planned follow up
Implementing patient centered approaches in caring for individuals with chronic pain and using principles drawn from the chronic disease management model to improve care systems may improve patient and provider satisfaction with chronic pain care. For instance, significant positive associations were found between a positive therapeutic alliance and the patient’s global perceived effect of treatment, change in pain, physical function, patient satisfaction with treatment, depression, and general health status in patients with chronic musculoskeletal pain in physical rehabilitation. Contributing to a positive therapeutic alliance are (1) therapist-patient agreement on goals of treatment, (2) therapist-patient agreement on intervention, and (3) the affective bond between patient and therapist. Several studies indicate that a patient’s perception of a provider’s engagement and concern impacts their perceived satisfaction more than improved health.
Coming to a mutual agreement on goals and intervention can be a challenge. To decrease the negative impact of chronic pain on functioning and health-related quality of life, patients must adopt self-management skills. In order to do so, in case of persistent non-reducible pain, patients have to be ready to stop focusing on further medical diagnostics to find a definite medical solution for pain and change to an active orientation regarding self-management. Not all patients are ready for this. For a good collaboration between the physical therapist and the patient, the patient must at least be planning to take an active orientation toward self-management, and the therapist should support and encourage this goal. Exercise improves pain and function in people with persistent musculoskeletal pain (PMSK), but adherence is often poor. Evidence suggests that exercise behaviors are modifiable, and behavior initiation and maintenance may be enhanced with behavior change interventions. , In a systematic review on behavior change techniques (BCTs) associated with adherence to prescribed exercise in patients with persistent musculoskeletal pain, a moderate level of evidence to support adherence for five BCTs was found, including (1) Social support (unspecified), (2) Goal setting (behavior), (3) Instruction of behavior, (4) Demonstration of behavior, and (5) Behavior practice/rehearsal. Treatment groups including seven or fewer BCTs, which were unique to any BCTs used in the control group, were most effective at enhancing exercise.
Not only do patients bring expectations about treatment, but the provider does as well. Treatment decisions are often heavily influenced by the personal beliefs of the provider. Several studies have indicated that the personal attitudes and beliefs regarding pain of rehabilitation professionals and other healthcare providers are associated with their advice to patients regarding regaining activities and return to work. Practitioners with a more biomedical orientation are more likely to use a pain-contingent treatment approach and focus on “curing” impairments, whereas practitioners with a more biopsychosocial orientation will more likely use a time-contingent treatment approach and focus on increasing activities. Linton and associates investigated the level of fear avoidance beliefs in practicing general practitioners and physical therapists. Compared to providers with low fear avoidance, providers with high levels of fear avoidance belief had an increased risk for believing sick leave to be a good treatment, not providing good information about activities, and being uncertain about identifying patients at risk for developing persistent pain problems. The combination of a high fear avoidant provider with a high fear avoidant patient seems a recipe for disaster in chronic pain management and should at all costs be avoided.
Different assessment tools are currently available to measure practitioners’ beliefs toward pain, such as the Attitudes to Back Pain scale for musculoskeletal practitioners (ABS.mp), the Healthcare Providers’ Pain and Impairment Relationship Scale (HC-PAIRS), and the Pain Attitudes and Beliefs Scale for Physiotherapists (PABS.PT).
It can be concluded that for optimal interaction with his or her patient, a rehabilitation professional should have (1) a dynamic, multidimensional knowledge base that is patient centered, (2) a clinical reasoning process that is embedded in a collaborative, problem solving venture with the patient, (3) a central focus on movement assessment linked to patient function, and (4) consistent virtues seen in caring and commitment to patients.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here