Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The human heart beats billions of times during the course of a normal life span, with each beat representing the amalgamation of electrical, biochemical, and mechanical events that occur over milliseconds. This chapter reviews the cellular and molecular processes that initiate and maintain blood pressure and blood flow to provide a framework for understanding concepts central to pharmacologic manipulation of the cardiovascular system.
Although many aspects of cardiovascular function have been known for thousands of years, it was not until the classic treatise by William Harvey in 1623 that the sequential relationship of the heart and vasculature was systematically characterized. Subsequent observation in both animals and man provided considerable insight into hemodynamics, particularly work by Stephen Hales, who in the 1730s measured blood pressure in horses and man, determined cardiac output, and had such a sophisticated appreciation of anatomy and fluid dynamics that he proposed regulation of vascular resistance by the microcirculation. At the subcellular level, technologic advances over the past 25 years have clearly had a profound effect on modern understanding of the molecular processes involved with cardiovascular function. Nonetheless, beginning in the mid-1800s, and using relatively crude methodologies, scientists developed a remarkably detailed understanding of the cardiac action potential, the central role of the calcium ion (Ca 2+ ) in excitation-contraction coupling and neurohormonal regulation of blood vessels.
The contraction of the heart follows from the spontaneous generation of an impulse (automaticity) that is routed through the anatomic conduction system, and ultimately to cardiomyocyte shortening. The path and speed of impulse conduction is dictated by the electrical characteristics of different cell types constituting the conduction system, which synchronizes contraction. The heart exhibits three main “electrical” characteristics that are regulated by the autonomic nervous system: chronotropy (rhythm of automaticity), bathmotropy (cellular excitability), and dromotropy (impulse conduction). Pathologic abnormalities (both congenital and acquired), as well as a wide variety of drugs, can alter cellular automaticity, excitability, and the velocity and path of impulse conduction.
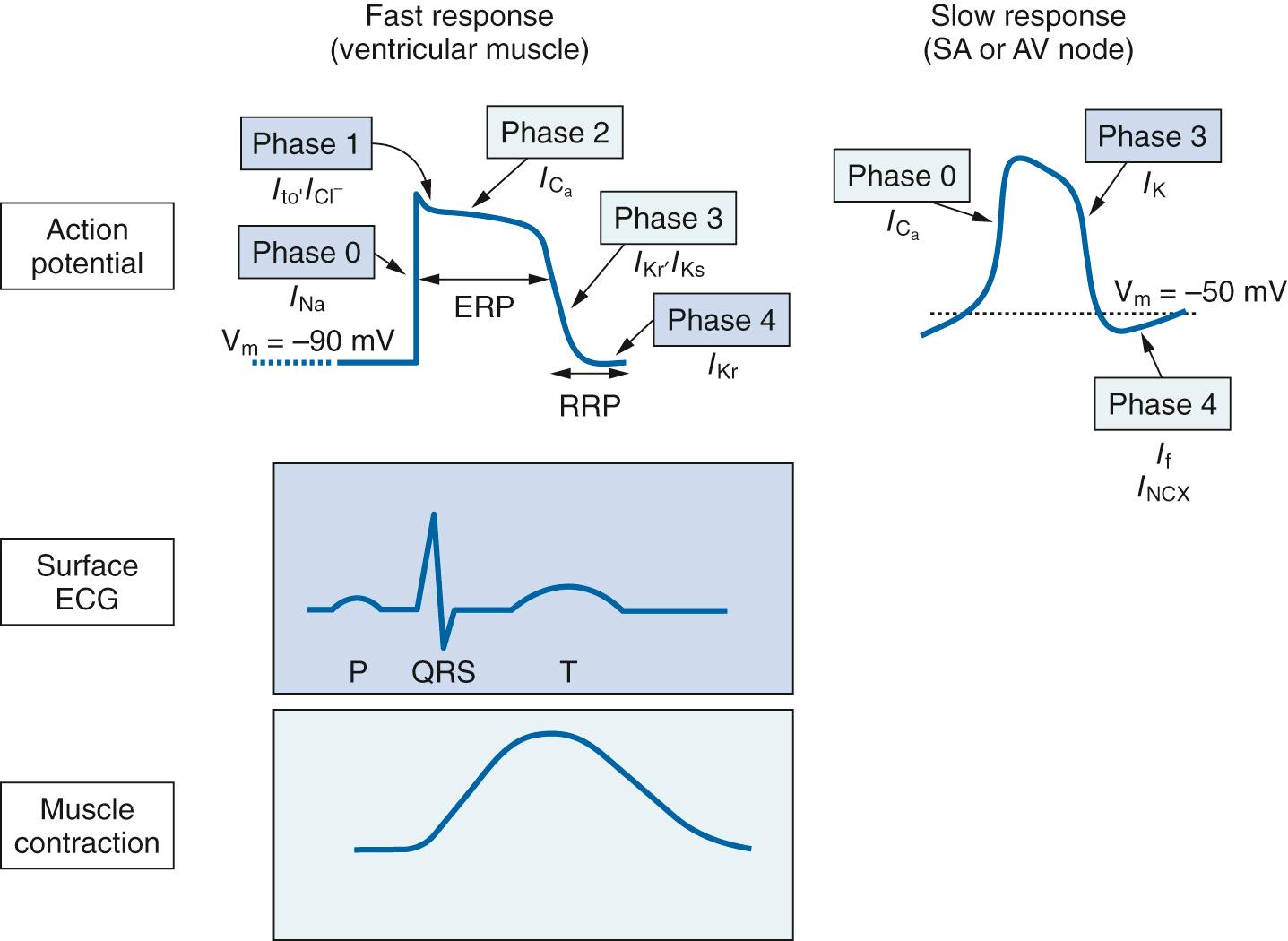
The fundamental process underlying all electrical activity in the heart is the action potential, which is an integrated movement of ions back and forth across the cell surface that results in rapid and reproducible changes in the electrical potential of the cell membrane ( Fig. 23.1 ). The characteristics and interactions among the various ion channels contributing to the action potential are complex and are reviewed more extensively in Chapters 8 and 27 . For the current discussion, a definition of basic terms and concepts is presented in the following text:
Membrane potential: Determined by the relative permeability of the cell membrane to specific ions, and forces both chemical (concentration gradient) and electrostatic (imparted by ion charge) that drive movement of ions across the membrane.
Conductance: An expression of how easily an ion flows across a membrane either through active pumps located in the membrane or ion channels; when specific ion channels open, conductance (g) for that ion increases.
Resting membrane potential: In cardiac cells, the conductance to the potassium ion (K + ) is high at rest, primarily because of diffusion out of the cells via selective K + channels along a concentration gradient; intracellular K + ([K + ] i ) is ~150 mEq/L, whereas extracellular K + ([K + ] o ) is ~5 mEq/L. The membrane is relatively impermeable to large anions such as proteins. Because these anions cannot follow K + out of the cell, the inside of the cell becomes negatively charged relative to the outside, and the resting membrane potential of myocytes is ~−90 mV. There is some movement of other ions across the cell membrane at rest, but conductance is very low relative to K + , so the resting membrane potential is close to the equilibrium potential for K + (E K ) of approximately −94 mV as calculated using the Nernst equation:
Unlike K + , myocyte conductance to the sodium ion (Na + ) is low at rest because voltage-gated Na + channels that allow Na + entry into the cell are closed. Nonetheless, because the concentration of extracellular Na + is much higher than intracellular (~145 mM vs. 10 mM) and the cell interior is negatively charged, both chemical and electrostatic forces drive some Na + ions across the membrane, which is the basis for secondary active transport of other molecules including Ca 2+ and hydrogen (H + ) ions. This movement is minimal and only slightly increases the membrane potential above the E K (i.e., from −94 to −90 mV). However, the slow Na + current could eventually depolarize the cell.
Maintenance of the Na + /K + gradient across the cell membrane is therefore critical and is actively achieved by expenditure of energy to move ions against an electrochemical gradient by the sodium-potassium adenosine triphosphatase (Na + /K + -ATPase), also known as the “sodium pump”. It is composed of α and β subunits and α 1 and α 2 isoforms. The α subunits contain both the Na + and K + binding sites and the adenosine triphosphate (ATP) catalytic site. The α 1 isoform is homogeneously distributed in the sarcolemma, while the α 2 isoform is localized in the T-tubules and may play a role in the excitation-contraction coupling. This protein extrudes 3 Na + ions for every 2 K + ions taken in, with ATP serving as the energy source; the pump is electrogenic in that charge movement across the membrane is unbalanced. Because of the central role of the Na + /K + -ATPase in maintaining membrane potential and its multiple downstream effects, the protein is the focus of extensive research. Myocytes also express Ca 2+ channels that permit Ca 2+ to enter the cells along its electrochemical gradient—that is, extracellular [Ca 2+ ] ≫ intracellular [Ca 2+ ]. The sarcolemmal Na + /Ca 2+ exchanger (NCX) catalyzes the countertransport of 3 Na + ions and 1 Ca 2+ ion using the inward gradient for Na + to drive the extrusion of Ca 2+ . Under physiologic conditions, this mechanism contributes to removal of Ca 2+ from the cardiac cell after each beat, thus facilitating relaxation and the maintenance of Ca 2+ balance. However, in common pathologic conditions, Ca 2+ influx via NCX can be enhanced, resulting in intracellular Ca 2+ accumulation, which can exacerbate cardiac injury and contractile dysfunction and lead to arrhythmias. For example, during reperfusion following ischemia, acidosis provokes Na + overload via the Na + /H + exchanger, which can slow or even reverse NCX activity. As with the Na + /K + -ATPase, the sarcolemmal NCX remains widely studied in regard to its role in cardiac pathology and as a target for pharmacologic manipulation.
Threshold potential: The membrane potential at which inward currents exceed outward currents as the result of voltage-gating of Na + and Ca 2+ channels, and depolarization becomes self-sustained. At this point, the action potential is initiated.
Fast versus slow response tissues (see Fig. 23.1 ): Fast response tissues depend on the opening of voltage-gated Na + channels to initiate depolarization. These tissues include the atria and ventricles, along with the specialized infranodal conducting system (bundle of His, fascicles and bundle branches, terminal Purkinje fibers). In contrast, depolarization in slow response tissues, such as the sinoatrial (SA) and atrioventricular (AV) nodes, is initiated by movement of Ca 2+ through long-lasting (L-type) voltage-gated Ca 2+ channels. Fast and slow response tissues also differ with regard to the magnitude and stability of their resting membrane potential (the basis for automaticity) and the amplitude of the action potential.
In addition to differences in how depolarization is initiated between fast and slow tissues, there are fundamental differences in the subsequent action potential, underscoring how each tissue can exhibit different sensitivities to disease or drugs. The following comparison starts with the action potential phase during which depolarization begins for each tissue ( Table 23.1 .)
| Fast Response | Slow Response | |
|---|---|---|
| Tissues | Atria, ventricles, bundle of His, fascicles, bundle branches, and terminal Purkinje fibers | Sinoatrial and atrioventricular nodes |
| Phase 0—Rapid depolarization | Opening of the voltage-gated Na + channels | Increased Ca 2+ conductance through L-type Ca 2+ channels |
| Phase 1— Early repolarization | K + efflux and chloride influx | None |
| Phase 2— Plateau | Slow calcium 2+ entry Na + channels in the closed inactivated state |
None |
| Phase 3—Final repolarization | K + efflux exceeds Ca 2+ influx | Increased K + efflux Closure of L-type Ca 2+ channels |
| Phase 4—Resting membrane potential | Activation of the NA + /K + -ATPase Na + channels in the resting state |
−60 mV: Slow inward Na + influx −50 mV: Opening of T-type Ca 2+ channels −40 mV: Opening of voltage gated L-type Ca 2+ channels Slow K + efflux |
When the membrane potential reaches threshold, voltage-gated Na + channels open, leading to a rapid Na + entry along both a marked concentration gradient (chemical force) and the electrostatic force provided by charge difference across the membrane. The voltage-gated Na + channels have a short open time, meaning that most of the channels close within a few milliseconds after the initiation of the action potential. However, a small subgroup of these channels reopens during the latter phases of the action potential, leading to a sustained Na + influx called the late current. The Na + channels remain in this so-called fast-inactivated state until the membrane potential becomes more negative, at which time they return to their resting (ready-to-go) state. Before this can occur, however, the membrane potential becomes positive for a period of time (overshoot); although there is no longer an electrostatic drive for Na + to enter the cell, a concentration gradient still exists to push Na + across the membrane. During depolarization, voltage-gated Ca 2+ channels (VGCC) also open but the inward flux is much slower than for Na + .
With termination of the inward Na + current (I Na ) resulting from Na + channel fast-inactivation and the positive membrane potential, both chemical and electrostatic forces promote K + efflux from the cell, described as a transient outward current ( I to ), and a modest inward chloride current ( I Cl ) to elicit a decline in membrane potential.
A continued slow Ca 2+ entry current (I Ca ) offsets the electrical effect of K + loss secondary to opening of voltage-gated K + channels. The plateau voltage is sufficient to maintain Na + channels in the closed, fast-inactivated state.
This phase begins when the efflux of K + exceeds the influx of Ca 2+ and the I Ca current ends. The delayed rectifier K + current (I K ) in phase 3 has both rapid ( I Kr ) and slow ( I Ks ) components that lead to repolarization and return to the resting potential.
The Na + /K + -ATPase extrudes Na + that entered during depolarization and restores the K + lost during repolarization. Once the resting potential is stabilized, Na + channels return to their resting state and are ready for the next depolarization.
During a single cardiac cycle (i.e., one action potential), the voltage-gated Na + channel exists in three different states: (1) resting, (2) active (open) during phase 0 depolarization, and (3) inactive at positive potentials (end of phase 0) and with marked depolarization (phase 2 plateau). Even though Na + cannot pass through the channel when in the resting or inactivated conformations, these two states are physiologically distinct. In the resting state, achieving the threshold potential opens the channel. In contrast, once the Na + channel is inactivated, it cannot be activated again until it cycles back to the resting membrane potential, which brings it into the resting state. Most drugs, including various antiarrhythmic compounds, preferentially bind to the inactivated state of the Na + channel. These distinctions can be clinically important.
When the membrane potential reaches its maximum negative point after repolarization (about −60 mV), slow, inward (depolarizing) Na + currents are activated. Referred to as funny currents ( I f ), because unlike most currents they are activated by hyperpolarization not depolarization, the I f cause the membrane potential to begin a slow spontaneous depolarization . When the membrane potential reaches about −50 mV, transient or T-type Ca 2+ channels open, allowing Ca 2+ to enter the cell along its electrochemical gradient and further depolarize the membrane. When the potential reaches about −40 mV, VGCC open to further depolarize the cell until an action potential threshold is reached (between −40 and −30 mV). A slow decline in the outward movement of K + also occurs during phase 4 as the K + channels responsible for repolarization during phase 3 continue to close.
While I f have come to be known as the “membrane voltage clock” that dictates spontaneous membrane depolarization, recent studies have suggested that automaticity is more complex. Spontaneous, rhythmic release of Ca 2+ into the cytoplasm from storage sites within the sarcoplasmic reticulum (SR) occurs during phase 4 and leads to activation of another depolarizing ionic current through the NCX (I NCX ), known as the “subsarcolemmal calcium clock.”
The I f and T-type Ca 2+ currents decline as their respective channels close, and depolarization is primarily caused by increased Ca 2+ conductance through the L-type Ca 2+ channels that begins toward the end of phase 4. Movement of Ca 2+ through these channels is not rapid, so the slope of phase 0 (the rate of depolarization) is much slower than found in fast response tissues. However, it is possible for fast response tissues to be converted to slow response tissues by tissue damage and electrolyte imbalance. Under these circumstances, Na + channels can become inactivated, with depolarization then dependent on the slow Ca 2+ channels:
Phase 1—plateau: None for slow response tissue.
Phase 2: None for slow response tissue.
Phase 3: K + channels open, thereby increasing outwardly directed, hyperpolarizing K + currents. At the same time, there is inactivation and closure of L-type Ca 2+ channels, decreasing Ca 2+ conductance and inward depolarizing Ca 2+ currents.
The cardiac muscle fibers are made of many individual cardiac cells connected in series to one another with gap junctions forming a syncytium. When a slow action potential develops in a membrane, current flows from this membrane to adjacent areas. Ions can then flow from one cell to another via low-resistance gap junctions, and if the current flow is sufficient, it causes sequential depolarization from cell to cell. The gap junctions are dynamic structures, opening and closing in response to changes in pH, Ca 2+ , and under some circumstances, voltage. Impulse propagation can also be affected by the orientation of myofibers and of the collagen matrix in which the fibers reside.
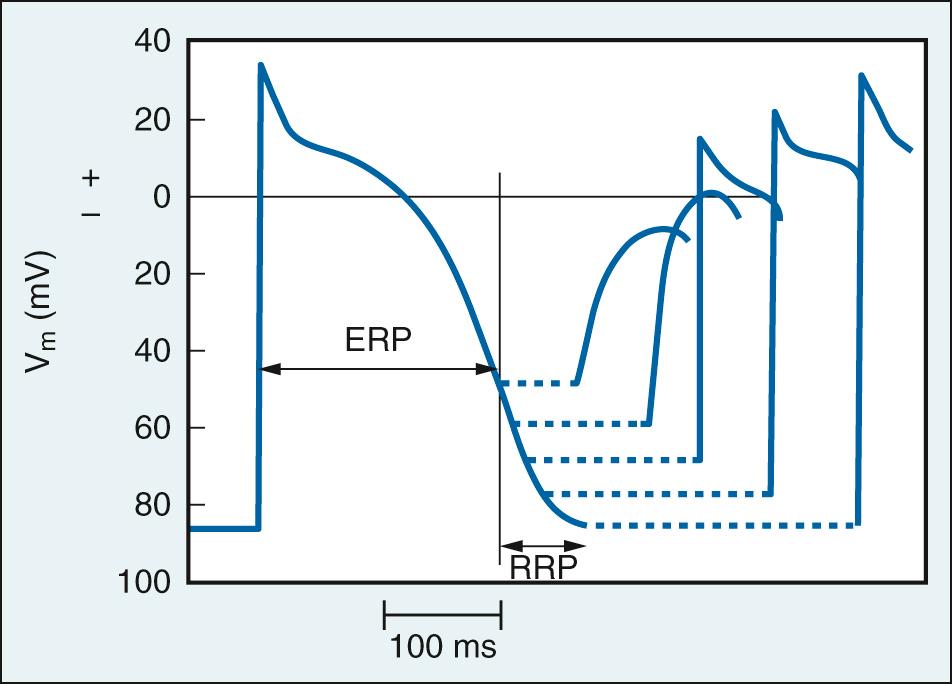
For an impulse to be conducted from cell to cell, or more globally to be spread throughout the heart, cells in the path must be excitable (bathmotropy). The characteristics of excitability for a cell depend on whether it exhibits fast or slow action potentials. Within fast response tissues, the membrane potential is not affected by an electrical impulse from the beginning of phase 0 to a midpoint in the repolarization process in phase 3 (the effective refractory period; see Fig. 23.1 ). When the membrane potential recovers below −50 mV, enough of the fast Na + channels have transitioned from the inactivated to resting state to allow for the membrane to again depolarize. However, because not all fast channels have recovered, the slope and amplitude of any resulting action potentials will not be normal until the membrane potential has been allowed to stabilize at its more negative values at the end of phase 3 when the Na + channels have entirely recovered from fast inactivation ( Fig. 23.2 ). This represents the relative refractory period. In contrast, within slow response tissues the relative refractory period persists even after the membrane has fully repolarized, a characteristic known as postrepolarization refractoriness . Importantly, under most circumstances the heart rate—either spontaneous or paced within a physiologic range—provides a cycle length (beat-to-beat duration in milliseconds) that is longer than the refractory period, thus allowing for full recovery of the action potential. However, duration of the action potential is affected by cycle length. For example, measurements obtained from canine Purkinje fibers show that at a cycle length of 630 msec (heart rate of 95 beats/min) the action potential duration was 180 msec, whereas at 400 msec (heart rate of 150) action potential duration was shortened to 140 msec, although the amplitude was maintained—that is, the membrane was not in a relative refractory period. This phenomenon appears to primarily reflect changes in K + conductance through delayed rectifier K + channels.
The velocity at which an impulse is conducted (dromotropy) is largely determined by the resting membrane potential, the amplitude of the action potential, and the rate of change in membrane potential during phase 0 (dV m /dt). These characteristics are affected by autonomic nervous system regulation, pathologic or pharmacologic inactivation of Na + channels by hyperkalemia or ischemia-induced acidosis, direct damage to cardiomyocytes, or the effect of chemicals, particularly antiarrhythmic drugs. Accordingly, regional variations in conduction velocity can be dynamic and profound. Slow conduction in the AV and SA nodes ranges from 0.02 to 0.1 m/sec, fast conduction in cardiomyocytes range from ~0.3 to 1 m/sec, and those in specialized conducting fibers are even more rapid (~1 to 4 m/sec).
The only normal path for impulse conduction from the atria to the ventricles is through the AV node. Consequently, this region of the heart represents a site for physiologic, pathologic, and pharmacologic alteration of rhythm. Although much of the basic information regarding structure-based electrophysiology of the AV node has come from animal studies, it appears that the AV node and the surrounding “perinodal area” are composed of multiple cell types that are electrophysiologically distinct. Three main types have been described and are localized to regions within or adjacent to the AV node: the atrionodal (AN), nodal (N), and nodal-His (NH) cells. The small, ovoid N cells are the primary sites where impulse conduction is slowed and therefore modulated, representing a distinctly slow response tissue with few gap junctions and reduced excitability compared with surrounding cells. The Ca 2+ current-dependent upstroke of phase 0, a major determinant of conduction velocity, is relatively prolonged in slow response tissue. In contrast, surrounding “transitional cells” have a greater density of Na + channels, with an action potential and conduction velocity more like fast response tissue; variations in AV node conduction (i.e., fast and slow pathway conduction) have been described in which impulses are diverted through regions with different conduction velocities.
In keeping with a critical regulatory role, the AV node is densely innervated by autonomic nerve fibers and can also be affected by autocoids (adenosine) and local metabolic influences (hypoxia, acidosis). Direct or pharmacologic stimulation of sympathetic or parasympathetic nerves has profound, often counterbalancing, effects on the action potentials, and therefore conduction velocity, of both N and transitional cells. Sympathetic stimulation activates G-protein–coupled β-adrenergic receptors (predominantly β 1 ) to activate adenylyl cyclase, and via multiple mechanisms increases the L-type calcium current, I f , and the inward rectifying K + current. Ultimately, β 1 agonism enhances automaticity and excitability, along with increasing action potential amplitude and conduction velocity (positive chronotropy, bathmotropy, and dromotropy). Parasympathetic stimulation activates G-protein–coupled M 2 muscarinic receptors to decrease adenylyl cyclase activity, and reduces automaticity and excitability, increases refractoriness, and slows AV node conduction (negative chronotropy, bathmotropy, and dromotropy). In addition, AV nodal cells express surface receptors for adenosine (A 1 ); agonist binding stimulates inhibitory G proteins that inhibit adenylyl cyclase. In addition, pathways downstream to both M 2 and A 1 receptors affect I f and various K + currents. Rate-related hyperpolarization of the N cell membrane also contributes to reduced excitability, increased refractoriness, and AV conduction slowing to the point of even complete block.
While the generation and propagation of electrical impulses in the heart provide a stimulus, it is the mechanical response to this stimulus—cardiomyocyte contraction—that generates the pressure actually driving cardiovascular function. Literally hundreds of years of research, using both intact hearts and isolated muscle, have yielded several essential principles for cardiac contraction:
Cardiac muscle contraction, unlike that of skeletal muscle, is an all-or-none response.
The magnitude and rate of cardiac contractile responses reflect cytoplasmic Ca 2+ concentration or Ca 2+ sensitivity of contractile proteins.
When stimulated with greater frequency, the heart normally contracts with greater force and relaxes more rapidly.
Cardiac muscle contractile force is length-dependent.
Modern experimental techniques involving molecular biology have provided considerable insight into phenomena at the subcellular level and have challenged some traditional fundamental assumptions. Furthermore, increased understanding of cardiac pathophysiology has underscored the importance of molecular regulation of lusitropy (relaxation), in addition to that of inotropy (contractility).
The T-tubules are invaginations of the myocytes surface cell membrane present at each Z-line that form a complex network within the cells. They constitute specialized regions of the cell membrane that play an integral role in excitation-contraction coupling and in ensuring synchronous Ca 2+ release and rapid Ca 2+ extrusion from the myocyte ( Fig. 23.3 ). During phase 2 of the fast tissue action potential, the influx (extracellular to intracellular) of Ca 2+ via VGCCs and, to a much lesser extent the NCX, functions as “activator Ca 2+ ,” which stimulates the SR to release a larger amount of Ca 2+ , a process known as Ca 2+ -induced Ca 2+ release (CICR) ( Fig. 23.4 ).
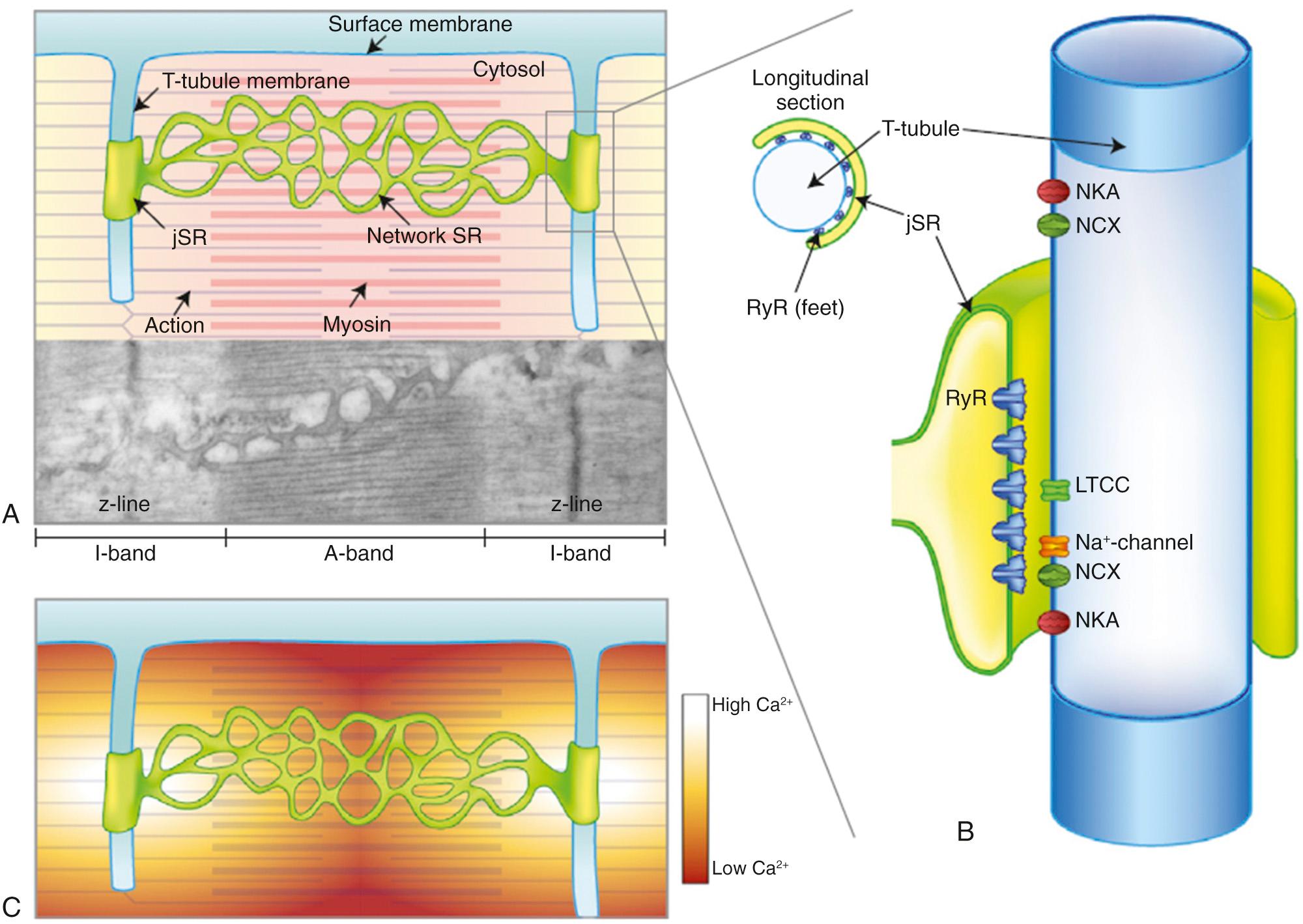
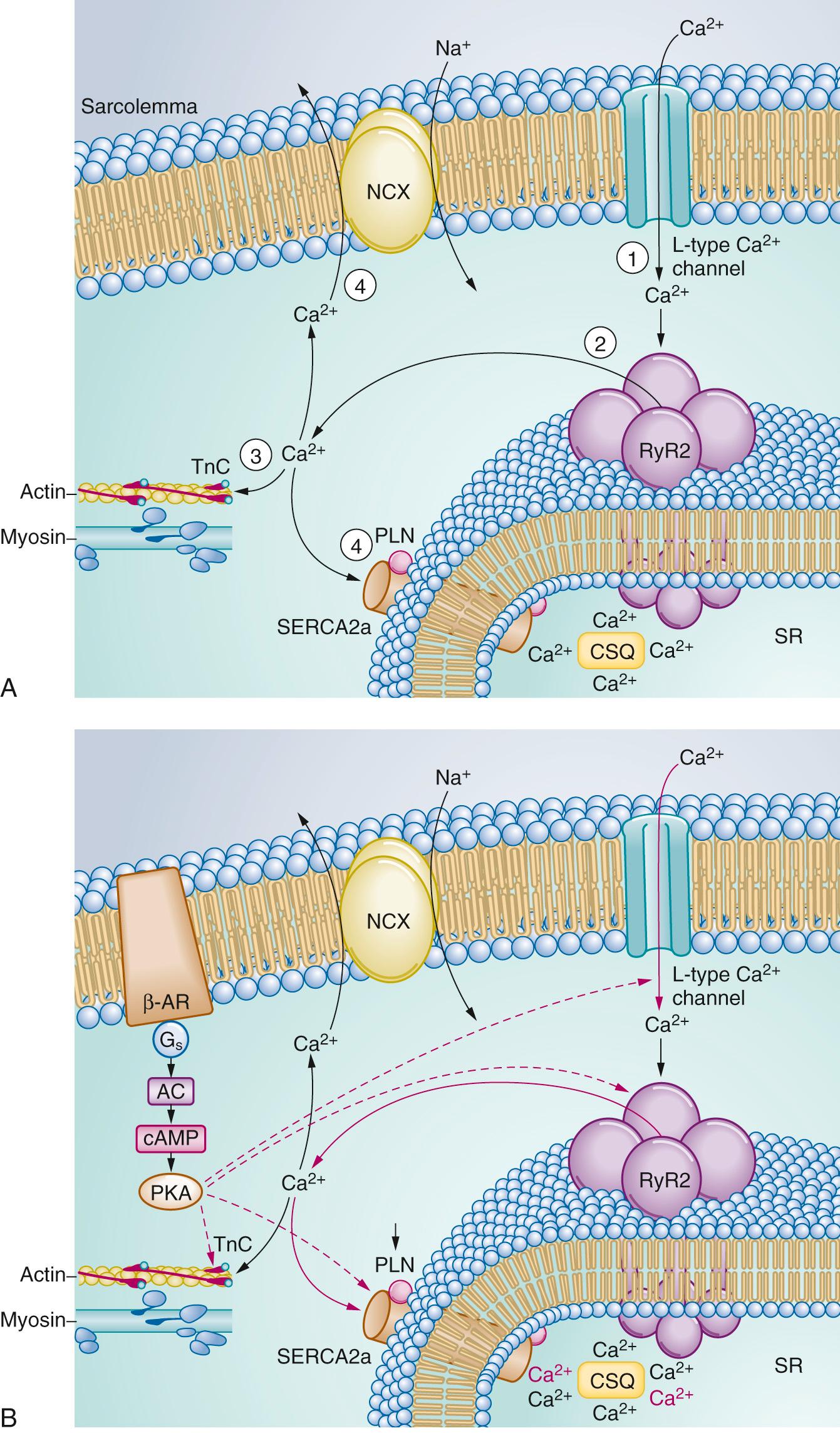
Storage and release of Ca 2+ by the SR are relatively complex processes modulated by high-capacity Ca 2+ -binding proteins such as calsequestrin and the ryanodine-sensitive Ca 2+ release channel, respectively. Calsequestrin is able to bind and store large amounts of Ca 2+ with low affinity, thus reducing the amount of free Ca 2+ in the SR and maintaining a low concentration gradient relative to the cytoplasm. Known as the ryanodine receptor (RyR), the SR Ca 2+ release channel exists in multiple isoforms, with type 2 (RyR2) predominantly found in the heart. When activated, RyR2 has a very high conductance for Ca 2+ ; as Ca 2+ exits the SR, dissociation of Ca 2+ from calsequestrin provides for continued high conductance, and cytosolic Ca 2+ concentrations rise rapidly from ~10 −7 M to 10 −5 M. Recent evidence indicates that SR Ca 2+ release is not initially a global event but occurs as bursts or “sparks” in zones where L-type VGCC in T-tubules are in close proximity to the SR and RyR2 proteins. Less well appreciated, and of less physiologic importance, is the fact that SR Ca 2+ release can also be stimulated by the second messenger inositol triphosphate ( IP 3 ) binding to the IP 3 receptor (IP 3 R) on the SR membrane. This is a relatively slow-onset process that has been linked to stimulation of α-adrenergic receptors on cardiomyocytes and to muscle remodeling.
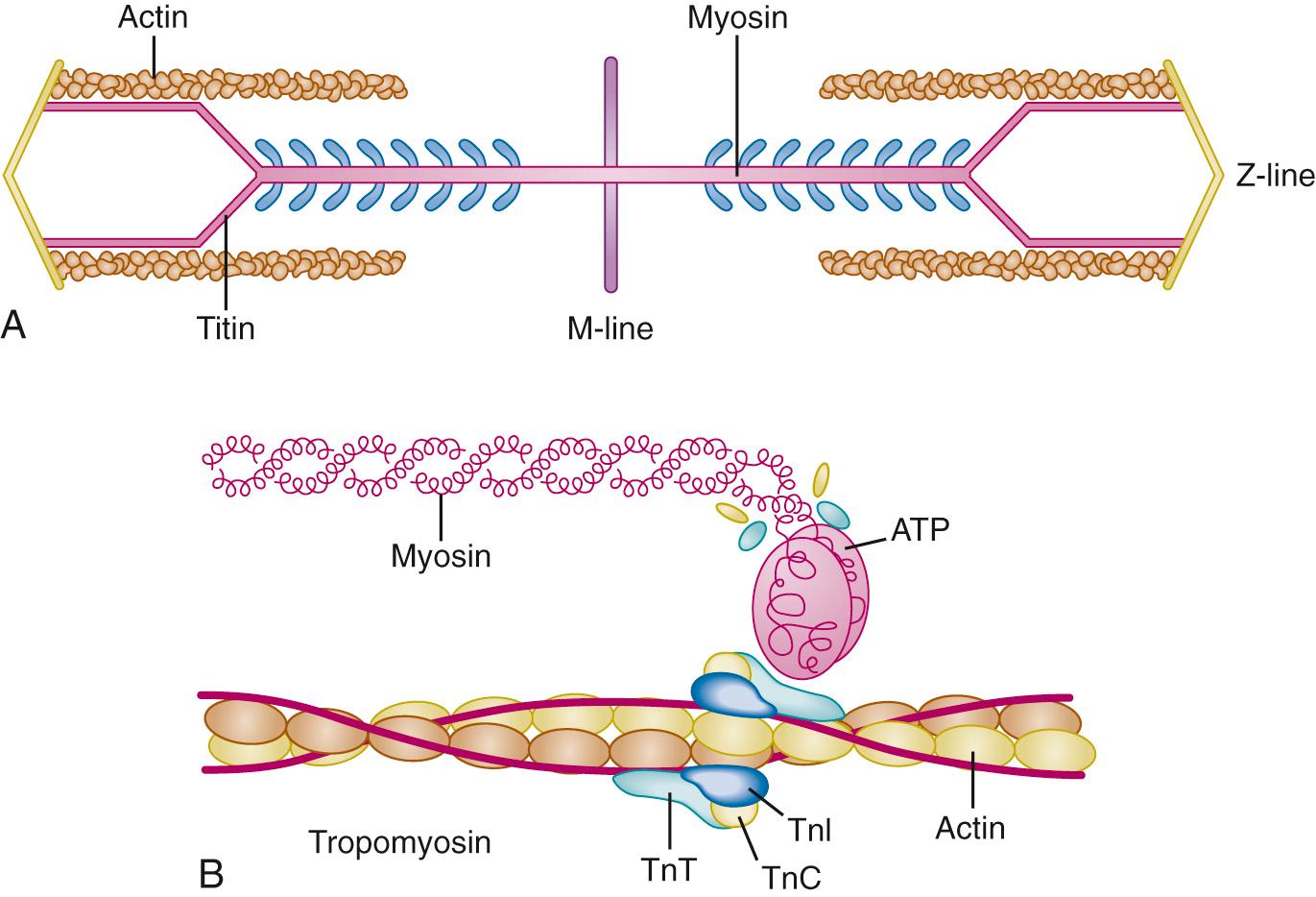
As with all muscles, the molecular stimulus for contraction of the cardiomyocyte is Ca 2+ binding with contractile proteins ( Fig. 23.5 ). Within the sarcomere, the troponin complex containing the subunits TnI (binds to actin), TnC (the Ca 2+ binding component), and TnT (binds troponin to tropomyosin) dictates the interaction between actin and myosin. In the relaxed state, tropomyosin blocks formation of myosin cross-bridges. When cytoplasmic Ca 2+ reaches ~10 −6 M, binding to TnC results in a conformational change in troponin, leading to changes in tropomyosin that facilitate formation of actin-myosin cross-bridges. The number of cross-bridges formed, the rate at which this process occurs, and the duration of cross-bridge attachment determine the resulting force. Each cross-bridge cycle consumes one molecule of adenosine triphosphate (ATP). A simplified two-stage model involving “on-time” and “off-time” for actin-myosin cross-bridges has been proposed as a means to help characterize inotropic regulation. Within this model, during each cross-bridge cycle (and there are many during each cardiac contraction), the myosin head attaches to actin and rotates to produce a unitary force for that interaction that is maintained during the on-time. Dissociation of myosin results in a non–force-producing state during the off-time. It is then the combination of on-time and the unitary force that determines the force-time integral for each cross-bridge, and ultimately the number of cross bridges attached per unit time, that determines overall contractile force.
As soon as the stimulus to release Ca 2+ is terminated, active reuptake into the SR, and, to a lesser extent, extrusion from the cell via the NCX, leads to a rapid decline in intracellular Ca 2+ , thus facilitating dissociation of Ca 2+ from TnC and to relaxation. The reuptake of Ca 2+ into the SR is a fast (time constant of ~100 msec), energy-dependent process involving the sarcoplasmic endoreticular calcium ATPase (SERCA) and its regulatory protein phospholamban (PLN). As with RyR, SERCA is found throughout the body in different isoforms; the type 2a isoform (SERCA2a) predominates in the heart. Under resting conditions, SERCA2a does not function at maximal capacity owing to an inhibitory influence of PLN. However, the inhibitory effect of PLN is lost when the protein is phosphorylated at one of two sites, each sensitive to different kinases (protein kinase A [PKA] and calmodulin-dependent kinase II [CaMKII]).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here