Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Good evidence-based practice dictates that clinicians always quantitate the extent of neuromuscular block by objective monitoring.
The neuromuscular block should be adjusted to ensure optimal surgical conditions. In most procedures, one or two responses to train-of-four (TOF) stimulation will suffice. To avoid involuntary diaphragmatic movements, a deeper level of neuromuscular block is required (i.e., one to five responses to post-tetanic count [PTC]).
Adequate recovery of postoperative neuromuscular function cannot be guaranteed without objective neuromuscular monitoring.
Objective neuromuscular monitoring is essential for management of neuromuscular blockade intraoperatively and its reversal for postoperative care. Muscle relaxants should not be given in the intensive care unit without proper monitoring.
It is impossible to exclude with certainty clinically significant residual neuromuscular block by clinical evaluation of recovery of neuromuscular function.
Residual postoperative neuromuscular block causes decreased chemoreceptor sensitivity to hypoxia, functional impairment of the pharyngeal and upper esophageal muscles, impaired ability to maintain an open upper airway, and an increased risk of hypoxemic events, as well as the development of postoperative pulmonary complications.
Absence of tactile fade in the response to TOF stimulation, tetanic stimulation, and double-burst stimulation does not exclude significant residual block.
To exclude clinically significant residual neuromuscular block, the TOF ratio must exceed 0.9 when measured mechanically or electromyographically and 1.0 when measured acceleromyographically.
Antagonism of the neuromuscular block with a cholinesterase inhibitor should not be initiated before at least two to four responses to TOF stimulation are observed.
Antagonism of the neuromuscular block achieved by rocuronium and vecuronium can be initiated at all levels of block with the selective relaxant binding agent sugammadex.
If adequate recovery (TOF ≥0.9-1.0) has not been documented objectively at the end of the surgical procedure, the neuromuscular block should be antagonized.
The editors, publisher, and Dr. Casper Claudius would like to thank Dr. Jorgen Viby-Mogensen for his contribution to this chapter in the prior edition of this work. It has served as the foundation of the current chapter.
Our understanding of the pathophysiologic consequences of residual paralysis has improved over the last decades, and it is now generally accepted that even small degrees of residual paralysis (i.e., a train-of-four [TOF] ratio 0.7-0.9) may be clinically harmful. As a consequence, the benchmark of adequate neuromuscular recovery has been revised several times; an adductor pollicis TOF ratio of 0.9 or greater is now required to exclude relevant residual neuromuscular block (i.e., paralysis). Clinically significant residual paralysis cannot be excluded using clinical criteria and it can persist postoperatively. Objective monitoring of the degree of neuromuscular block associated with pharmacologic reversal reduces the incidence of residual paralysis and should be part of standard perioperative monitoring when neuromuscular blocking agents (NMBAs) are used.
In awake patients, muscle power can be evaluated by tests of voluntary muscle strength, but this is impossible during anesthesia and recovery from anesthesia. Historically, anesthesiologists have used clinical tests to assess muscle power directly and to estimate neuromuscular function indirectly (muscle tone; feel of the anesthesia bag as an indirect measure of pulmonary compliance, tidal volume, and inspiratory force). All these tests are influenced by factors other than the degree of neuromuscular block and, therefore, should not be used to evaluate recovery from neuromuscular blockade. Whenever precise information regarding the status of neuromuscular functioning is desired, the response of muscle to nerve stimulation should be assessed. This procedure also takes into account the considerable variation in individual response and sensitivity to muscle relaxants.
This chapter reviews the basic principles of neuromuscular monitoring and the requirements for effective use of nerve stimulators for peripheral nerve stimulation. It also describes the response to nerve stimulation during depolarizing (phase I and phase II) and nondepolarizing neuromuscular block, provides information about the level of neuromuscular blockade, and discusses the consequences of residual paralysis. Moreover, methods of evaluating evoked neuromuscular responses with and without the availability of recording equipment are discussed.
Neuromuscular monitoring is used to evaluate the effect of a NMBA. The muscle response after stimulation of its corresponding motor nerve is assessed. The most frequently assessed nerve-muscle unit is the ulnar nerve and the adductor pollicis muscle. The muscle response can be evaluated either qualitatively with a peripheral nerve stimulator or quantified with objective monitors. With the peripheral nerve stimulator, the observer evaluates the muscle response either tactically or visually, whereas with the monitor the response is objectively measured and displayed on a screen. Whatever method is used for neuromuscular monitoring, the clinician should be familiar with the following terms: supramaximal stimulation, calibration, impedance, and safety margin.
The reaction of a single muscle fiber to a stimulus follows an all-or-none pattern. In contrast, the response (the force of contraction) of the whole muscle depends on the number of muscle fibers activated. If a nerve is stimulated with sufficient intensity, all fibers supplied by the nerve will react, and the maximum response will be triggered. After administration of a neuromuscular blocking drug, the response of the muscle decreases in parallel with the number of fibers blocked. The reduction in response during constant stimulation reflects the degree of neuromuscular block.
For the preceding principles to work, the stimulus must be truly maximal throughout the whole period of monitoring; therefore, the electrical stimulus applied is usually at least 15% to 20% greater than that necessary for a maximal response. For this reason, the stimulus is said to be supramaximal. This compensates for potential changes in skin resistance intraoperatively and assures constant maximal stimulation throughout the procedure.
However, supramaximal electrical stimulation can be painful, which is not a concern during anesthesia, but during recovery the patient may be awake enough to experience the discomfort of nerve stimulation. Therefore, some researchers advocate stimulation with submaximal current during recovery. Although several investigations indicate that testing of neuromuscular function can be reliably performed postoperatively with submaximal stimulation, the accuracy of such monitoring is unacceptable with that low current.
A device used for objective monitoring of the neuromuscular function should be calibrated before the NMBA is administered. Calibration adjusts the gain of the device to ensure that the observed response to supramaximal stimulation is within the measurement window of the device and as close as possible to the “100% control response.” The calibration procedure varies with the type of device used, but most often it is done with 1.0 Hz single-twitch stimulation. It is especially important to calibrate when the onset and recovery of the neuromuscular block are established with single-twitch stimulation.
In the TOF mode of nerve stimulation, calibration is considered less important because all four responses are amplified equally. Consequently, the TOF ratio is rarely influenced by calibration; however, in patients with very weak or strong responses to nerve stimulation, one or more responses to TOF stimulation might be out of the recording window, and the displayed TOF response might be incorrect. In some devices, supramaximal stimulation is established concurrently with the calibration procedure.
An alternative and novel option to ensure a constant maximum stimulus throughout the whole procedure is to control the impedance (resistance) of the skin. Indeed, as long as the resistance of the skin is below a threshold value, the neuromuscular monitoring device will stimulate with the same user-selected electrical current (i.e., 60 mA). For a maximum current of 60 mA, the maximal resistance of the skin should be equal to or lower than 5 kΩ. If the resistance of the skin is above this value, the monitor will not be able to stimulate the patient with the selected current. More recently, nerve stimulators have been introduced that indicate the level of skin impedance on the screen (e.g., TofScan by iDMed, Marseille, France). Using this approach, establishment of supramaximal stimulation is not needed to assure that nerve stimulation is effective and constantly maximal through the whole procedure.
Neuromuscular transmission has a substantial margin of safety. Neuromuscular block only becomes evident when 70% to 80% of acetylcholine receptors at the neuromuscular endplate are occupied by nondepolarizing NMBDs and to produce complete block, 90% to 95% of receptors must be occupied. Thus, the currently available equipment and the currently applied stimulation patterns allow only insight to this 70% to 95% range of receptor occupancy. This should be kept in mind, especially during recovery of neuromuscular block, where 70% of the acetylcholine receptors at the neuromuscular endplate may still be occupied but no longer detectable with neuromuscular monitoring.
Neuromuscular function is monitored by evaluating the muscular response to supramaximal stimulation of a peripheral motor nerve. Theoretically, two types of stimulation can be used: electrical and magnetic. Electrical nerve stimulation is by far the most commonly used method in clinical practice, and it is described in detail in this chapter. In theory, magnetic nerve stimulation has several advantages over electrical nerve stimulation. It is less painful and does not require physical contact with the body; however, the equipment required is bulky and heavy, it cannot be used for TOF stimulation, and it is difficult to achieve supramaximal stimulation with this method. As a result, magnetic nerve stimulation is not used in clinical anesthesia.
Electrical impulses are transmitted from stimulator to nerve by means of surface or needle electrodes. Normally, disposable pre-gelled silver or silver chloride surface electrodes are used. The conducting area should be small, approximately 7 to 11 mm in diameter ( Fig.43.1 ). Otherwise, the current produced in the underlying nerve may not be adequate. Ideally, the skin should be cleansed properly and preferably rubbed with an abrasive before application of the electrodes. When the selected current cannot be obtained with surface electrodes, needle electrodes can be used in a few exceptional cases. Although specially coated needle electrodes are commercially available, ordinary steel injection needles often suffice. A sterile technique should be used, and the needles should be placed subcutaneously to avoid direct injury to the underlying nerve.
In principle, any superficially located peripheral motor nerve can be stimulated and the response to corresponding muscle measured. Choosing the site of neuromuscular monitoring depends on several factors: the site should be easily accessible during surgery, it should allow quantitative monitoring and finally, direct muscle stimulation should be avoided. Direct muscle stimulation is characterized by weak contractions without fade persisting even at a deep level of neuromuscular blockade. The risk is increased when the stimulation electrodes are directly attached over the muscle to be assessed. To prevent direct muscle stimulation, the nerve-muscle unit should be chosen so that the site of nerve stimulation and the site of the subsequent evaluation of the twitch response are topographically (anatomically) distinct.
In clinical anesthesia, the ulnar nerve is the gold standard as a stimulation site, but the median, posterior tibial, common peroneal, and facial nerves are also sometimes used. For stimulation of the ulnar nerve, the electrodes are best applied to the volar side of the wrist (see Fig. 43.1 ). The distal electrode should be placed approximately 1 cm proximal to the point at which the proximal flexion crease of the wrist crosses the radial side of the tendon to the flexor carpi ulnaris muscle. The proximal electrode should preferably be placed so that the distance between the centers of the two electrodes is 3 to 6 cm (see Fig. 43.1 ). With this placement of the electrodes, electrical stimulation normally elicits only finger flexion and thumb adduction. If one electrode is placed over the ulnar groove at the elbow, thumb adduction is often pronounced because of stimulation of the flexor carpi ulnaris muscle. When this latter placement of electrodes (sometimes preferred in small children) is used, the active negative electrode should be at the wrist to ensure maximal response. Polarity of the electrodes is less crucial when both electrodes are close to each other at the volar side of the wrist; however, placement of the negative electrode distally normally elicits the greatest neuromuscular response. When the temporal branch of the facial nerve is stimulated, the negative electrode should be placed over the nerve, and the positive electrode should be placed somewhere else over the forehead. When the posterior tibial nerve is stimulated, the electrodes should be placed close to the medial malleolus, with the same distance as described above and the negative electrode being placed distally.

Several nerve-muscle units may be chosen in clinical practice. Most often the ulnar nerve-adductor pollicis muscle is used.
Ulnar nerve-adductor pollicis muscle: This nerve-muscle unit is easily accessible intraoperatively if the arm is in the outstretched position and the hand in the supine position. The stimulatory response can be evaluated tactilely, visually, or by objective means. It has the lowest risk of direct muscle stimulation, because it ensures topographic separation of the stimulated nerve and the evaluated muscle by stimulating the ulnar nerve running along the median side of the arm and assessing the muscle response at the adductor pollicis muscle, which is indeed located on the lateral side of the hand.
Posterior tibial nerve-flexor hallucis brevis muscle: This nerve-muscle unit can be used for monitoring when the hands are inaccessible. The flexor hallucis brevis muscle produces flexion of the big toe following posterior tibial nerve stimulation. The characteristics (onset and recovery) of the neuromuscular block at the flexor hallucis brevis muscle is almost consistent with that of the adductor pollicis muscle.
Facial nerve-orbicularis oculi and facial nerve-corrugator supercilii muscle: When the arms are tucked under surgical drapes, quite often the only accessible site for monitoring is the head. Two facial muscles can be used as monitoring sites: the orbicularis oculi muscle and the corrugator supercilii muscle. The former encircles the orbital opening; its stimulation through the zygomatic branches of the facial nerve causes the eyelids to close. Stimulation by the temporal branch of the facial nerve of the latter one draws the medial end of the eyebrow downward, producing wrinkling of the brow. However, because the facial nerve is in direct proximity to the intrinsic mimic muscles, the risk of direct muscle stimulation is significant. Therefore, care must be taken that the correct stimulatory response is assessed, and any other twitching muscle in the direct proximity of the stimulation electrodes is not falsely interpreted. Stimulation of the facial nerve can be accomplished with significantly lower currents: most often 25 to 30 mA are sufficient. Stimulation of these two muscles is technically difficult and the result often unsatisfactory in clinical practice.
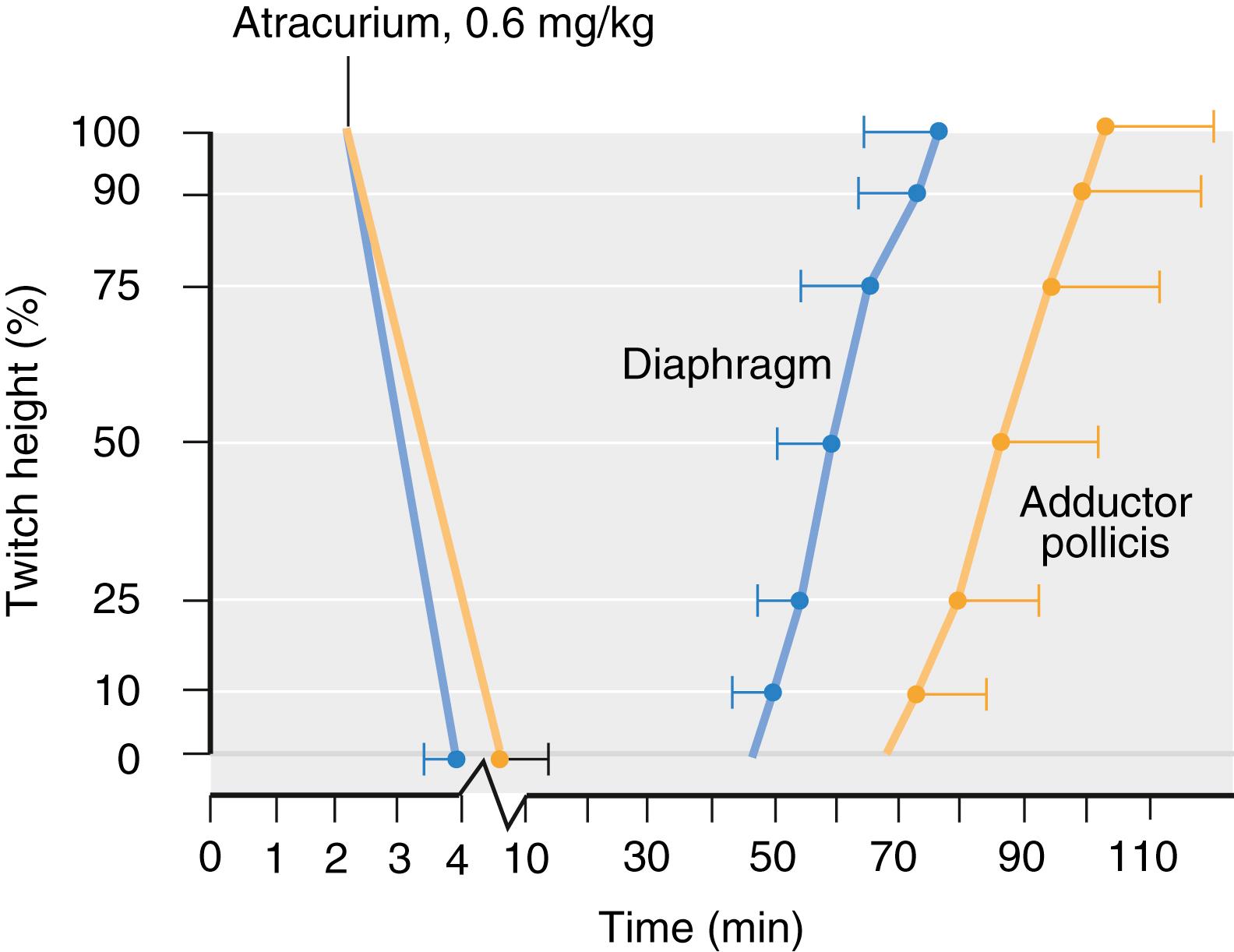
Because different muscle groups have different sensitivities to neuromuscular blocking drugs, results obtained for one muscle cannot be automatically extrapolated to other muscles. However, most of the studies that are the base for dosing recommendations of NMBAs arise from measurement of the stimulation of the ulnar nerve. The diaphragm is among the most resistant of all muscles to both depolarizing and nondepolarizing neuromuscular blocking drugs. In general, the diaphragm requires 1.4- to 2.0-fold as much muscle relaxant as the adductor pollicis muscle for an identical degree of block ( Fig. 43.2 ). Also of clinical significance is that onset time is normally shorter for the diaphragm than for the adductor pollicis muscle, and the diaphragm recovers from paralysis more quickly than the peripheral muscles ( Fig. 43.3 ). The other respiratory muscles are less resistant than the diaphragm, as are the larynx and the corrugator supercilii muscles. Most sensitive are the abdominal muscles, the orbicularis oculi muscle, the peripheral muscles of the limbs, and the geniohyoid, masseter, and upper airway muscles. From a clinical point of view, the response of the corrugator supercilii to facial nerve stimulation reflects the extent of neuromuscular block of the laryngeal adductor muscles and abdominal muscles better than the response of the adductor pollicis to ulnar nerve stimulation. Furthermore, the upper airway muscles seem to be more sensitive than the peripheral muscles. Although some investigations using acceleromyography (AMG) have indicated small differences in the response to TOF nerve stimulation in the hand (adductor pollicis muscle) compared to the leg (flexor hallucis brevis muscle), these differences are probably of little clinical significance. When comparing different sites of stimulation, there might be large differences between contralateral limbs (e.g., arm-to-arm variation of ± 20%).

Although the precise source of these differences is unknown, possible explanations may be variations in acetylcholine receptor density, acetylcholine release, acetylcholinesterase activity, fiber composition, innervation ratio (number of neuromuscular junctions), blood flow, and muscle temperature.
For the evaluation of the neuromuscular function, the most commonly used patterns are TOF stimulation, double-burst stimulation (DBS), and posttetanic count (PTC) stimulation. Single-twitch stimulation and tetanic stimulation are mainly used as a component in composite stimulation patterns (i.e., TOF, DBS, or PTC).
Background : Single-twitch stimulation is the earliest and simplest pattern. The first device specifically developed to monitor the neuromuscular block, the “St. Thomas’s Hospital nerve stimulator,” could only deliver a single twitch. For decades it remained the only established stimulation pattern to assess neuromuscular blockade intraoperatively.
Stimulation pattern : In the single-twitch mode of stimulation, single electrical stimuli are applied to a peripheral motor nerve at frequencies ranging from 1.0 Hz (once every second) to 0.1 Hz (once every 10 seconds; Fig. 43.4 ) and the subsequent muscle response is evaluated. The response to single-twitch stimulation depends on the frequency at which the individual stimuli are applied. If the rate of delivery is increased to greater than 0.15 Hz, the evoked response will gradually decrease and stabilize at a lower level. Therefore, results obtained with 1-Hz single-twitch stimulation cannot be compared with results obtained using, for example, 0.1-Hz single-twitch stimulation. As a result, a frequency of 0.1 Hz is generally recommended.

Clinical application : To assess the degree of neuromuscular blockade after single-twitch stimulations, a comparison with a reference value recorded before administration of the NMBA is mandatory. Thus, without appropriate monitoring equipment, this stimulation pattern does not provide sufficient information of the level of block. In clinical practice, the single twitch stimulation has only limited value as a stand-alone stimulation pattern; it is mainly used as a component of the PTC stimulation and as 0.1 Hz single-twitch stimulation, it is sometimes used in scientific trials specifically to evaluate the time to onset of neuromuscular blockade. Moreover, it is the only stimulation pattern that allows, in conjunction with a monitoring device, assessing a depolarizing neuromuscular block after succinylcholine.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here