Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Cardiac arrest is a leading cause of mortality.
Current AHA Guidelines recommend chest compressions before initial airway management.
Ventilation and oxygenation during CPR can be performed via bag mask ventilation or an advanced airway device (either an endotracheal tube or a supraglottic airway).
Interruptions in chest compressions should be minimized during airway management.
Hyperventilation should be avoided during CPR.
Ventilation plays a larger role in pediatric and neonatal resuscitation and high levels of supplemental oxygen should be avoided in neonates.
Introduction
Basic Life Support and Cardiopulmonary Resuscitation Guidelines
Changes to AHA Guidelines 2010–2015
AHA Updated Guidelines 2015-2020
Initial Airway Management During Cardiopulmonary Resuscitation
Rescue Breathing
Airway Adjuncts
Advanced Airway Management During Cardiopulmonary Resuscitation
Confirmation of Endotracheal Tube Placement During Cardiopulmonary Resuscitation
Supraglottic Airway Devices
Role of Advanced Airway Devices
Use of Cricoid Pressure During Cardiopulmonary Resuscitation
Alternative Methods of Oxygen Delivery During Cardiopulmonary Resuscitation
Oxylator
ResQPODPassive Oxygen Insufflation
Airway Management Postintubation and after Return of Spontaneous Circulation
Challenges of Airway Management During Cardiopulmonary Resuscitation
Access to the Airway
Infection Risk During CPR and Airway ManagementCervical Spine InjuryEquipment Challenges
Controversies
Role of Hyperventilation
When to Secure the Airway
Supraglottic Airway Device Versus Endotracheal Intubation as an Advanced Airway Technique
Pediatric Basic and Advanced Life Support and Resuscitation
Neonatal Basic and Advanced Life Support and Resuscitation Clinical Pearls
Conclusion
Cardiac arrest is one of the leading causes of mortality in the United States. Most cardiac arrests occur outside the hospital, usually in the home, and 50% of arrests are unwitnessed. In-hospital cardiac arrests (IHCA) have a more favorable outcome than out-of-hospital cardiac arrests (OHCA). The average survival to discharge for adult OHCA patients who receive cardiopulmonary resuscitation (CPR) ranges from 3.4% to 22%, with a 10.4% survival rate after initial hospitalization and 8.2% survival rate with good functional outcome. Among adults admitted to hospitals, 1.2% suffer from IHCA, and of those, 25.8% were discharged from the hospital, and 82% of those survivors had good functional status. Early CPR and defibrillation are recognized as the most important treatment steps for cardiac arrest, but adequate oxygenation and ventilation are also important for providing oxygen to vital organ systems. Although earlier American Heart Association (AHA) CPR guidelines focused on the airway and ventilation as first steps in resuscitation, more recent versions have placed a stronger emphasis on rapid return of circulation.
The most common etiology of cardiac arrest in adult patients outside the hospital setting is cardiac in nature, most often ventricular fibrillation. In the hospital, however, cardiac arrest may be because of cardiac or pulmonary causes. Most first responders outside the hospital are not trained in advanced airway management; therefore, the AHA CPR guidelines related to airway management are different for lay rescuers than for in-hospital providers.
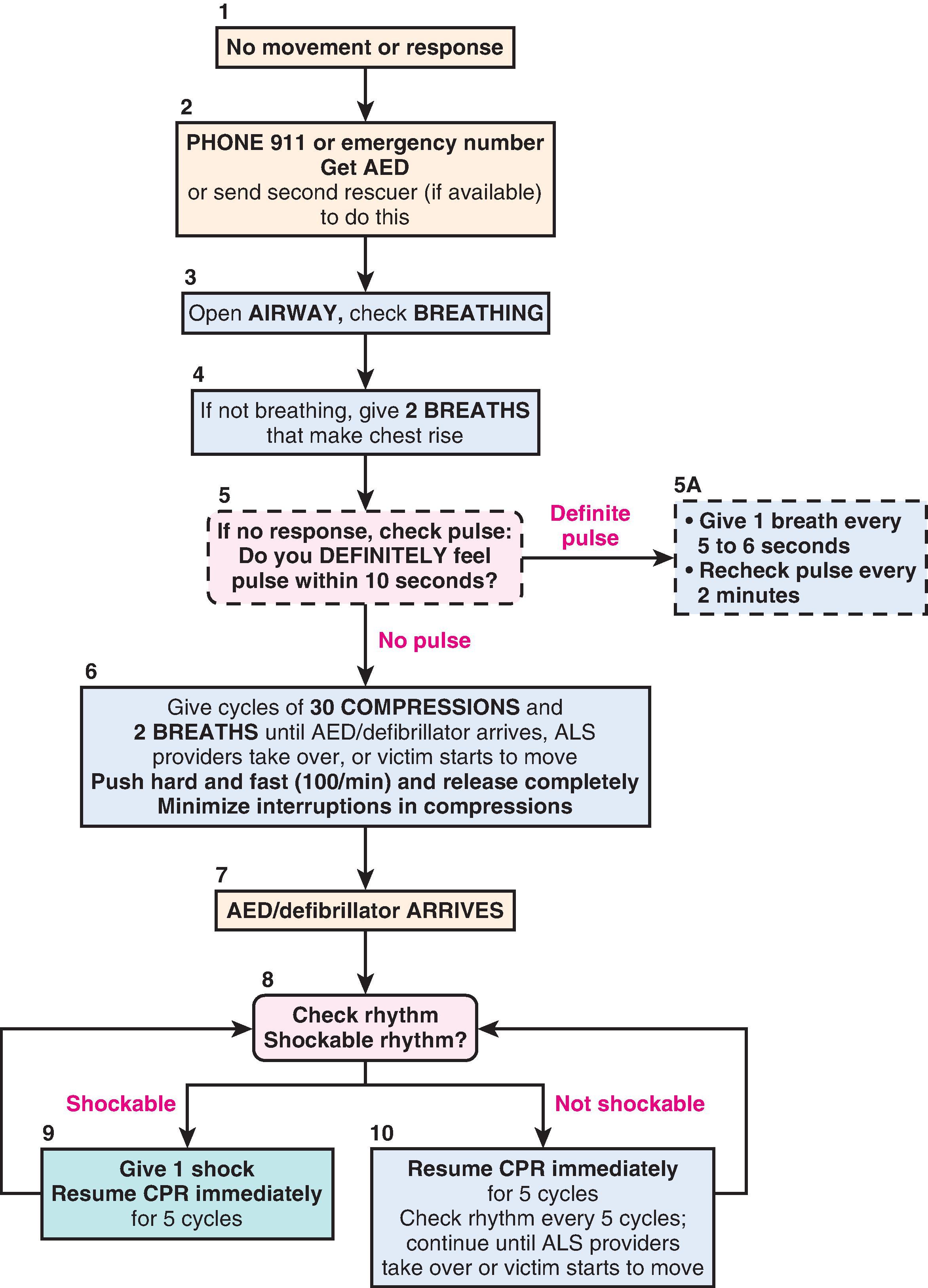
The initial 2005 AHA guidelines for basic life support (BLS) and CPR recommended the sequence of airway, breathing, and circulation (A-B-C). Thus, the first steps in the 2005 BLS guidelines were opening the airway, checking for breathing, and providing 2 rescue breaths if adequate breathing was not detected. The third step was to initiate chest compressions ( Fig. 32.1 ). To check for breathing, lay rescuers and healthcare providers were advised to “look, listen, and feel.” Healthcare providers were then advised to check for a pulse after delivering the initial rescue breaths to a nonresponsive, nonbreathing individual.
The 2005 AHA CPR guidelines recommended 2 rescue breaths, each given over 1 second, with sufficient tidal volume to produce visual chest rise. If an advanced airway was in place, the guidelines recommended 8 to 10 breaths per minute without synchronizing breaths between chest compressions.
Updated BLS and CPR guidelines were released by the AHA in 2010 and in 2015 with significant changes. Table 32.1 summarizes these guidelines. The recommended sequence was changed to circulation, airway, and breathing (C-A-B). In conditions of low blood flow (e.g., cardiac arrest), oxygen delivery to the brain and heart is limited primarily by blood flow rather than arterial oxygen content. Using cardiac-only resuscitation and minimizing delays or interruptions in chest compressions can improve survival. Evidence does not show any difference in survival rates between chest compressions delivered alone and chest compressions combined with positive-pressure ventilation (PPV). The 2010 AHA guidelines recommended that chest compressions be initiated before rescue breaths or advanced airway placement, with rescue breaths provided after the first cycle of chest compressions. “Look, listen, and feel” was removed from the 2010 algorithm. The AHA released updated guidelines in 2015, but the C-A-B sequence remained unchanged, with a continued focus on early initiation of quality chest compressions before airway management. The BLS components listed in Table 32.1 from the 2010 AHA guidelines were not changed in the 2015 update.
| Component | RECOMMENDATION | ||
|---|---|---|---|
| Adults | Children | Infants | |
| Initial response | Unresponsive | Unresponsive | Unresponsive |
| No breathing or no normal breathing (i.e., only gasping) No pulse palpated within 10 sec for all ages (HCP only) |
No breathing or only gasping | No breathing or only gasping | |
| CPR sequence | C-A-B | C-A-B | C-A-B |
| Compression rate | At least 100/min | At least 100/min | At least 100/min |
| Compression depth | At least 2 inches (5 cm) | At least one-half AP diameter | At least one-half AP diameter |
| About 2 inches (5 cm) | About 1.5 inches (4 cm) | ||
| Chest wall recoil | Allow complete recoil between compressions | Allow complete recoil between compressions | Allow complete recoil between compressions |
| HCPs rotate compressors every 2 min | HCPs rotate compressors every 2 min | HCPs rotate compressors every 2 min | |
| Compression interruptions | Minimize interruptions in chest compressions | Minimize interruptions in chest compressions | Minimize interruptions in chest compressions |
| Try to limit interruptions to <10 sec | Try to limit interruptions to <10 sec | Try to limit interruptions to <10 sec | |
| Airway | Head tilt and chin lift (HCP suspects trauma: jaw thrust) | Head tilt and chin lift (HCP suspects trauma: jaw thrust) | Head tilt and chin lift (HCP suspects trauma: jaw thrust) |
| Compression-to-ventilation ratio (until advanced airway placed) | 30:2—one or two rescuers | 30:2—one rescuer 15:2—two HCP rescuers |
30:2—one rescuer 15:2—two HCP rescuers |
| Ventilations when rescuer untrained or trained and not proficient | Compressions only | Compressions only | Compressions only |
| Ventilations with advanced airway (HCP) | 1 breath every 6 sec (10 breaths/min) | 1 breath every 6 sec (10 breaths/min) | 1 breath every 6 sec (10 breaths/min) |
| Asynchronous with chest compressions | Asynchronous with chest compressions | Asynchronous with chest compressions | |
| About 1 sec per breath | About 1 sec per breath | About 1 sec per breath | |
| Visible chest rise | Visible chest rise | Visible chest rise | |
| Defibrillation | Attach and use AED as soon as available | Attach and use AED as soon as available | Attach and use AED as soon as available |
| Minimize interruptions in chest compressions before and after shock | Minimize interruptions in chest compressions before and after shock | Minimize interruptions in chest compressions before and after shock | |
| Resume CPR beginning with compressions immediately after each shock | Resume CPR beginning with compressions immediately after each shock | Resume CPR beginning with compressions immediately after each shock | |
The recommended compression-to-ventilation ratio and ventilation rate with an advanced airway in place, as outlined in Table 32.1 , remained unchanged in the 2015 guidelines. The 2015 AHA guidelines also recommended that in a patient with a witnessed OHCA and a shockable rhythm, PPV may be delayed for up to three cycles of chest compressions. This recommendation was based on recent evidence that neurologic survival and survival to hospital discharge are improved with this delayed ventilation strategy. ,
The 2015 guidelines recommended that lay rescuers check for absence of breathing or gasping only after checking for patient response and activating emergency response, whereas the recommendation to healthcare providers is to check for lack of breathing and absence of pulse simultaneously ( Table 32.2 ). The 2015 guidelines also recommended that emergency dispatchers become trained to recognize that abnormal or agonal breathing patterns are associated with a high likelihood of cardiac arrest. The misinterpretation of agonal gasps or abnormal breathing as normal may delay the onset of chest compressions. ,
| Step | Untrained Lay Rescuer | Trained Lay Rescuer | Healthcare Provider |
|---|---|---|---|
| 1 | Confirm scene safety. | Confirm scene safety. | Confirm scene safety. |
| 2 | Check for patient response. | Check for patient response. | Check for patient response. |
| 3 | Shout for help, phone 911, or ask bystander to phone 911. Keep phone at side of patient, with the phone in speaker mode. | Shout for help, activate emergency response system. Keep phone at side of the patient if possible. | Shout for help, activate resuscitation team (resuscitation team can also be activated immediately after pulse/breathing check). |
| 4 | Follow the instructions provided by telecommunicator. | Check for absence of breathing or presence of gasping only. If none, begin chest compressions. | Check for absence of breathing or presence of gasping only while simultaneously checking for pulse. AED and emergency equipment should be retrieved immediately after breathing and pulse check. |
| 5 | Follow telecommunicator instructions to look for absence of breathing, identify gasping only. | Answer questions and follow instructions from telecommunicator. | Begin CPR immediately, use AED/defibrillator when available. |
| 6 | Follow instructions of telecommunicator. | Send a second person, if available, to retrieve an AED. | When a second rescuer arrives, provide two-person CPR and use AED/defibrillator. |
Although the optimal oxygen concentration to be delivered during CPR has not been defined, current AHA guidelines recommend initial delivery of 100% oxygen during resuscitation. After return of spontaneous circulation (ROSC), the 2010 guidelines recommended titration of oxygen administration to maintain oxygen saturation level of 94% or greater to avoid hyperoxia when appropriate monitoring is available. The 2015 guidelines added to this recommendation that the highest available oxygen concentration should be administered after ROSC to avoid hypoxia until arterial oxygen saturation or partial pressure of arterial oxygen can be measured. Box 32.1 summarizes the changes pertaining to airway management during CPR that were introduced in the 2010 AHA guidelines, and Box 32.2 summarizes the additional changes introduced in the recent 2015 AHA guidelines.
Management
The basic life support sequence changed from A-B-C to C-A-B for adults, children, and infants. Initiate chest compressions before ventilations.
Use of cricoid pressure during ventilations is not recommended.
Instruction to “look, listen, and feel for breathing” was removed from the algorithm.
Excessive ventilation should be avoided.
Continuous quantitative capnography is recommended to confirm endotracheal tube placement.
Oxygen concentration is weaned after return of spontaneous circulation to maintain oxygen saturation at 94% or greater.
Positive-pressure ventilation can be delayed for up to three cycles of CPR in OHCA patients with a shockable rhythm.
Passive ventilation techniques are not routinely recommended during conventional CPR but may be considered by EMS systems when performing continuous chest compressions.
Manual in-line stabilization, rather than an immobilization device, is recommended when cervical spine injury is suspected.
The use of ultrasound was added as method for confirming endotracheal tube placement.
Since 2015, the AHA has released yearly focused updates based on updated evidence, as well as updated guidelines in 2020 that incorporated updated recommendations from the previous focused updates. , The 2020 guidelines stress that if a patient demonstrates agonal breathing or gasping respiration, lay rescuers should assume the patient is in cardiac arrest and begin CPR. The steps and recommendations provided in Tables 32.1 and 32.2 remain unchanged in the updated 2020 guidelines.
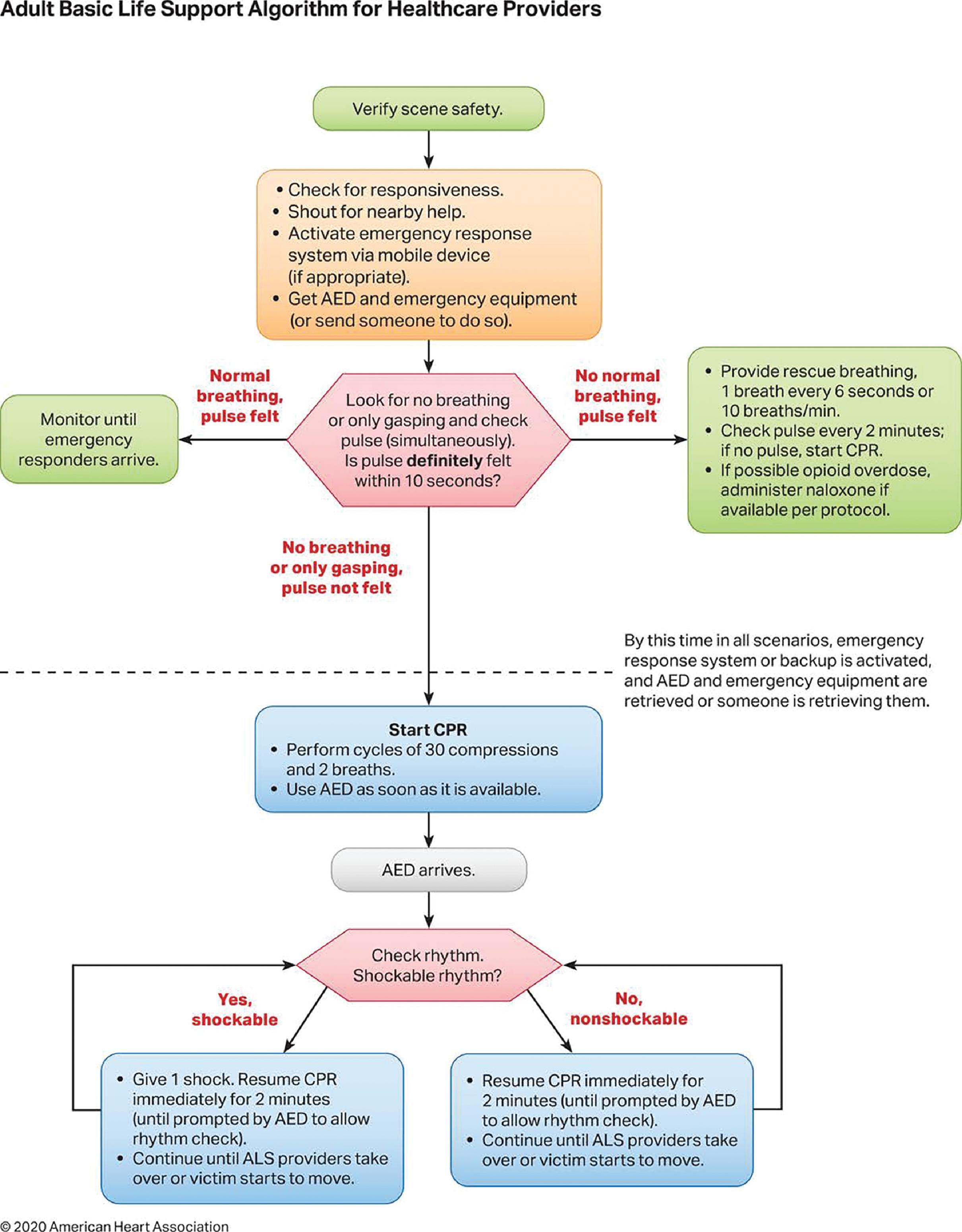
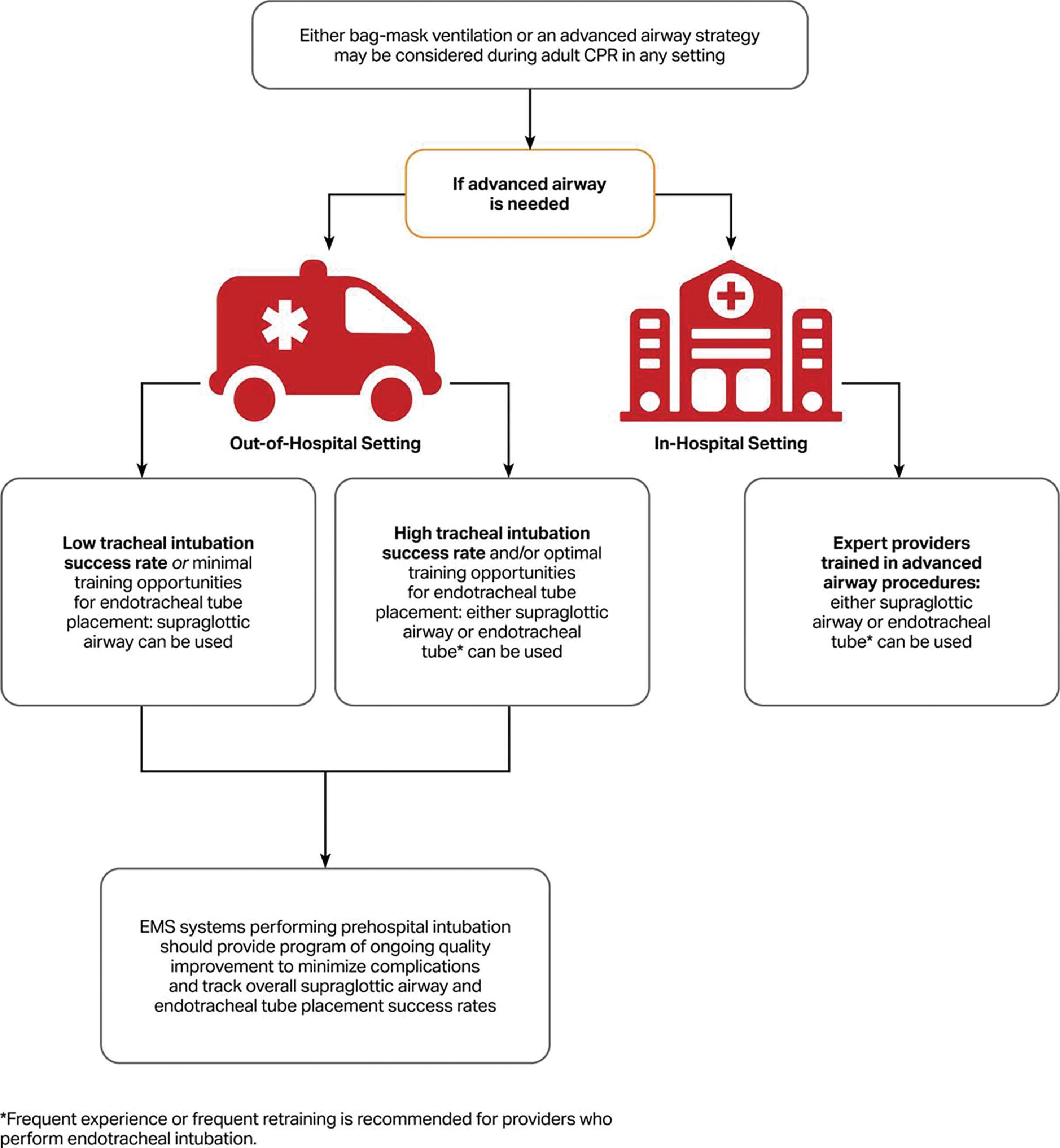
The 2019 focused update provided updated recommendations for the use of advanced airway devices and stressed the need for training and use of capnography, and these recommendations are incorporated into the 2020 updated guidelines as well , ( Box 32.3 ). Both the 2019 and 2020 guidelines also support previous versions to avoid interruptions in chest compressions for airway management, suggesting that advanced airway management can be delayed until after two rounds of chest compressions or even until after ROSC if bag-mask ventilation is adequate. The 2020 updated adult BLS algorithm for healthcare providers is shown in Fig. 32.2 . The only change in this algorithm from the 2010 and 2015 versions is the simplification to provide rescue breathing every 6 seconds or 10 breaths per minute. The 2020 updated AHA guidelines also recommend that either a supraglottic airway (SGA) or an endotracheal tube (ETT) can be considered as an advanced airway technique and that an SGA may be preferred over an ETT in settings with minimal training opportunities or low intubation success rates ( Fig. 32.3 ).
If a patient demonstrates agonal breathing or gasping respiration, lay rescuers should assume the patient is in cardiac arrest and begin CPR.
Rescue breathing was simplified to 10 breaths/minute.
Either bag-mask ventilation or an advanced airway may be considered during CPR in any setting.
Either a supraglottic airway (SGA) or an endotracheal tube (ETT) can be considered as an advanced airway technique,
In settings with minimal training opportunities or low intubation success rates, an SGA may be preferred.
Waveform capnography should be used to confirm and monitor ETT placement, including during transport.
Initial rescue breathing during CPR should be provided through a mouth-to-mouth method, mouth-to-barrier device, or bag-mask ventilation (if available). If the mouth is not accessible or the patient has a tracheal stoma, mouth-to-nose or mouth-to-stoma ventilation may be necessary. Each rescue breath should be given over 1 second with a sufficient tidalvolume to produce a visible chest rise. If a pulse is present, 1 rescue breath should be given every 6 seconds (or 10 breaths per minute) to maintain oxygen levels, and the pulse rechecked every 2 minutes. Once CPR is initiated, 2 ventilations should be provided after completing 30 compressions (30:2 compression-to-ventilation ratio). Trained lay rescuers or healthcare providers should initiate rescue breathing. An untrained lay rescuer should provide chest compressions only and not initiate rescue breathing.
The airway should be opened by a head-tilt–chin-lift maneuver, unless a cervical spine injury is suspected. If a cervical spine injury is suspected, a jaw thrust should be performed with the head maintained in a midline position.
Oropharyngeal airways can assist bag-mask ventilation by displacing the tongue, which can occlude the airway. Oropharyngeal airways are recommended for unconscious patients and should be placed by rescuers trained in their use.
Nasopharyngeal airways are better tolerated in conscious patients than are oral airway adjuncts, and they can assist ventilation by relieving nasopharyngeal obstruction. Nasal airway adjuncts should be placed by a rescuer trained in their use, and they should be avoided if a basilar skull fracture or coagulopathy is suspected. Case reports have described intracranial placement of the nasopharyngeal airway in the presence of a basilar skull fracture, so an oral airway is preferred in these patients. , Incorrect placement of an oropharyngeal or nasopharyngeal airway may worsen airway obstruction.
The primary goal of airway management during CPR should be to provide adequate oxygenation and ventilation. If bag-mask ventilation is adequate and an advanced airway strategy will interrupt chest compressions, current AHA guidelines suggest that insertion of an advanced airway can be deferred until either ROSC occurs or the patient fails to respond to chest compressions and defibrillation. If bag-mask ventilation is not adequate, however, an advanced airway should be placed.
Trained healthcare providers should perform tracheal intubation during CPR while minimizing interruptions in chest compressions. Tracheal intubation performed by direct laryngoscopy may be more difficult if performed during chest compressions. Prolonged attempts at tracheal intubation should be avoided, especially if chest compressions are halted during attempts. Placement of an endotracheal tube (ETT) or another advanced airway device has not been associated with any improvement in ROSC. Tracheal intubation attempts by inexperienced providers may result in complications, such as failed intubation or esophageal intubation.
After ETT placement, ventilations are delivered without interruption of chest compressions at a rate of 1 breath every 6 seconds. Certain resuscitation medications can be delivered through the ETT ( Box 32.4 ). Secretions can be removed from the airway through the ETT, and the ETT cuff may provide a barrier against aspiration. Per the 2020 updated AHA advanced cardiovascular life support (ACLS) guidelines, in order to use advanced airway devices effectively, healthcare providers should maintain their knowledge and skills through frequent practice. In addition to mastering bag-mask ventilation, providers should master an advanced airway strategy and a second (backup) strategy for use.
Administer two to three times the intravenous dosage, followed by 10 mL of normal saline:
Lidocaine
Epinephrine
Atropine
Vasopressin
Naloxone
More recent studies comparing the use of an SGA versus an ETT demonstrate no difference in survival or neurological outcome between the two techniques. Therefore, the most recent guidelines recommend that providers can use either advanced airway technique during CPR in any setting (OHCA or IHCA). Since the success of advanced airway placement is highly dependent on provider skill set, either bag-mask ventilation or an advanced airway is considered acceptable during CPR. If an advanced airway is used, an SGA can be used in settings with low intubation success rate or minimal training for ETT placement, whereas in settings where ETT placement success is high with optimal training, either an SGA or ETT can be used. See Fig. 32.3 for the current recommendations related to advanced airway management in patients with cardiac arrest.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here