Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Clinical signs to determine proper endotracheal tube (ETT) placement and positioning have limitations.
Secondary confirmatory methods must be used in routine and emergent settings to minimize the chances of ETT misplacement or improper ETT depth.
Exhaled CO 2 detection, especially by waveform capnography, is the most sensitive method to detect proper ETT placement in the respiratory tract.
Exhaled CO 2 determines tracheal placement of the ETT but does not eliminate the possibility of endobronchial intubation.
Exhaled CO 2 detection sensitivity decreases in cases with low or no pulmonary blood flow, such as during cardiac arrest.
After nonelective intubations outside the operating room, when the ETT will remain in place for an undetermined length of time, the use of chest x-ray (CXR) is recommended to confirm proper ETT depth.
The use of ultrasonography as a confirmatory method of proper tracheal tube placement and depth is gaining popularity and has many advantages over traditional radiologic methods.
Bilateral breath sounds do not always mean equal breath sounds and do not eliminate the possibility of an endobronchial intubation.
A normal end-tidal CO 2 (EtCO 2 ) and capnogram waveform cannot exclude the possibility of endobronchial intubation. An increased EtCO 2 , reduced EtCO 2 , or abnormal capnogram should encourage consideration of endobronchial intubation in the differential diagnosis of hypoxia or increased peak inspiratory pressures.
A fundamental tenet of elective and emergent airway management with tracheal intubation is the timely placement of the endotracheal tube (ETT) through the glottic opening, followed by confirmation of proper tube position. Inadvertent ETT misplacement, malposition, or dislodgment can have profound adverse clinical consequences. ETT misplacement occurs most commonly when inexperienced providers carry out intubation. However, it can even occur to seasoned veterans, especially in emergencies when airway management is performed in less-than-optimal conditions—for example, in the critically ill (including patients in cardiac arrest), in out-of-hospital intubations, and when difficulty visualizing the larynx is encountered.
Unrecognized esophageal intubation (EI) is the most severe complication of attempted tracheal intubation. All practitioners who perform advanced airway maneuvers experience EIs during their careers. Most EIs are immediately and easily recognized. When accidental EI is not promptly recognized, it can result in grave consequences: rapid, irreversible clinical deterioration, esophageal perforation (especially with traumatic intubation attempts), cerebral anoxia, and death. , If the ETT is inserted too deeply into a mainstem bronchus, complications range in severity from mild hypoventilation and atelectasis of the nonventilated lung, to hyperinflation and pneumothorax of the ventilated lung with subsequent development of hypoxemia and hemodynamic instability. The ETT may also not be placed deeply enough (i.e., pharyngeal placement), which predisposes to emesis, aspiration, and laryngospasm. In every instance where advanced airway maneuvers and tracheal intubation are performed, there should be a plan for assessment of tube placement and determination of tube depth, as well as proper documentation of both activities.
An ideal, “silver bullet” method or device to detect successful tracheal intubation does not exist. There is no method sufficiently reliable to confirm proper ETT placement and position in all patients and all circumstances. Properly placed ETTs may become displaced at any time; therefore, constant vigilance and reconfirmation of tube position may be needed. Of the available techniques to detect ETT placement, some are primarily intended to detect and confirm the ETT presence in the respiratory tract and rule out EI, whereas others are meant to establish correct ETT depth within the trachea. Some techniques have a dual role.
This chapter will review past and current knowledge of malpositioning of ETTs and the currently recommended techniques for primary and secondary determination of their adequate placement and positioning. Emphasis has been placed on more recent evidence because monitoring and detection methods have advanced considerably since the introduction in 1986 of the American Society of Anesthesiologists (ASA) Standards for Basic Monitoring, including oxygenation, ventilation, circulatory, and temperature monitors. Exhaled carbon dioxide (CO 2 ) as a monitor for proper ETT placement and ventilation has been widely adopted. It is espoused by both the American Heart Association (AHA) and the European Council on Resuscitation. , , Placement and positioning of double-lumen tubes are discussed elsewhere.
Tracheal intubation is considered the gold standard for advanced airway management. It can be performed in controlled settings, such as the operating room, or emergently, in and out of the hospital, in different circumstances, including trauma. Tracheal intubation is performed in all patient age groups by a diverse group of medical and paramedical providers with different skills, abilities, and procedural experience. Given the variety of circumstances, it is no surprise that the incidence of ETT malposition at the time of intubation or as a result of dislodgment after placement has been reported to be in the 4% to 26% range, with an incidence of accidental EI of 2.7% to 25%. , With significant advancements in airway management in the past three decades, and the introduction of mandatory ETT confirmation methods, the incidence of misplacement and malposition of ETT, including accidental EI, has decreased in all but the emergency setting and pediatrics. Airway management in the emergency setting is often performed in uncontrolled circumstances, in combative or intoxicated patients, or in tight spaces with decreased visibility. Transportation to or within a medical facility also predisposes to malposition or displacement of ETTs. , Pediatric and neonatal patients have proportionately shorter tracheas and therefore are particularly vulnerable to ETT misplacement and dislodgment, even with mild head flexion and extension.
In recent decades, there has been considerable interest in understanding and attempting to limit the impact of adverse events related to airway management. Several large-scale efforts have been conducted since advanced airway maneuvers became popular in the second half of the 20th century. These efforts have been extensively studied and reported, mainly by the ASA Closed Claims Project in the United States, the Australian Incidence Monitoring Study in Australia (AIMS), the Canadian Medical Protective Association (CMPA), the Denmark National Board of Patients’ Complaints (NBPC), and more recently the Fourth National Audit Project (NAP4) of the Royal College of Anaesthetists and the Difficult Airway Society. Major complications in airway management are rare but carry a high degree of mortality. They cover a broad spectrum of injuries ranging from mild, transitory, nonlife-threatening reversible issues to irreversible ones, such as brain damage and death. They are frequently associated with medicolegal issues and costly malpractice claims.
There are two primary sources of information for studies of airway-related complications: litigation-based retrospective reviews and critical incident analyses. These resources share the same goal of identifying problem areas related to different aspects of anesthetic care and analyzing patterns of injury so that strategies for prevention can be devised.
The nature of anesthesia malpractice claims has changed considerably since the 1970s. Modern respiratory monitoring (i.e., capnography for ventilation and pulse oximetry for oxygenation) was introduced in 1986 and adopted as part of the standard of care. In 1993, the ASA Task Force on Management of the Difficult Airway introduced Practice Guidelines for Management of the Difficult Airway. Since the introduction of the guidelines, significant complications, such as death and brain damage, have declined. Respiratory and airway-related events continue to be an important source of adverse events, according to the latest ASA closed claims analysis published in 2011, representing events from 1970 through 2007. Respiratory management issues, including airway management, accounted for 17% of claims in 2011, compared with 34% in Caplan’s original report in 1990. The most common respiratory events leading to anesthesia claims since 1990 were difficult intubation, inadequate oxygenation or ventilation, and pulmonary aspiration. In the original report, accidental EI (the most severe and lethal of all adverse events related to ETT misplacement) was reported in 18% of cases, and was considered the third most common event related to airway management. Since that time, EI has decreased to 5%, which is a significant improvement and a practice management success.
Almost any practitioner who has attempted tracheal intubation has experienced incidents of EI. This is for the most part harmless; what is of concern and a significant cause of litigation is placing an ETT in the esophagus and not recognizing it promptly before undue harm occurs. Unrecognized EI continues to be a problem because of its associated lethality and liability, especially in cases outside the operating room, in the emergency department, and in critical care and trauma settings. EI also has been reported consistently in all databases: The 2005 CMPA report showed that in 9 of the 16 cases where airway management was a central issue of litigation, EI occurred; the AIMS study revealed that there were 35 incidents of EI, which constituted 1.75% of all adverse events reported; NAP4 included 11 EIs resulting in 6 deaths. , Failure to detect adequate ETT placement and exclusion of EI constitute avoidable diagnostic errors that are usually caused by failure to adequately interpret clinical signs and confirm ETT placement with secondary methods.
No technique for confirmation of tracheal intubation is 100% reliable in all circumstances and age groups; therefore, the use of multiple available confirmatory methods is recommended when attempting to confirm the placement of ETTs. Even though the clinical determination of proper ETT placement should be performed in all instances, none of the primary clinical modalities (visualization of the ETT passing through the vocal cords, auscultation of bilateral breath sounds, humidification of the ETT, chest wall movement, and lack of abdominal distention) alone or in combination are sufficiently accurate to determine proper ETT placement and position, and, given their subjectivity, they must be accompanied and supplemented by rapid secondary point-of-care methods and techniques.
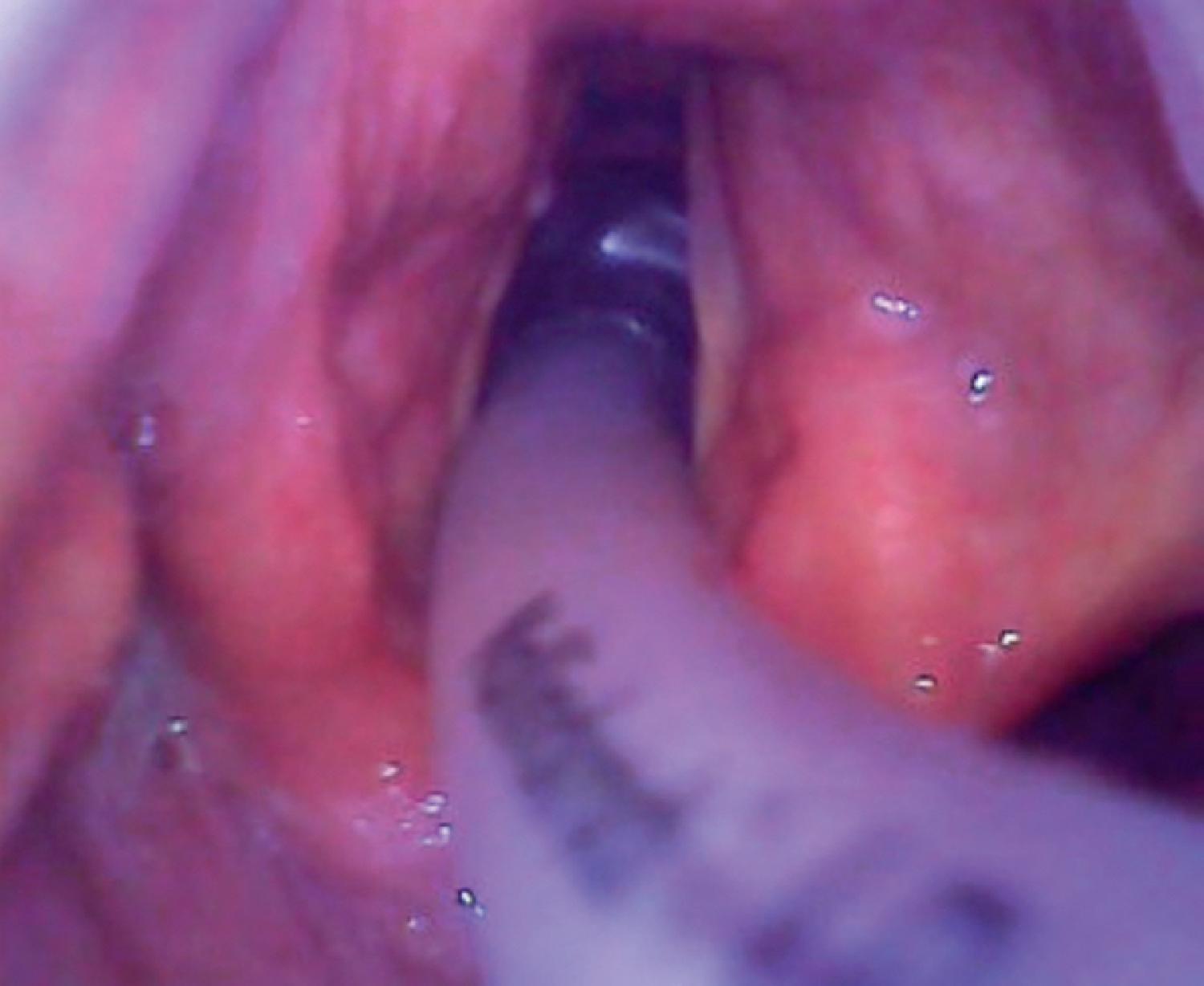
Visualization of the ETT passing through the vocal cords during any type of laryngoscopy is a primary technique to determine proper placement of the ETT but is fallible, does not determine proper positioning, and does not exclude dislodgement either before or after the ETT has been secured. Visualization of the ETT as it passes through the vocal cords is an operator-dependent method, and the success and effectiveness vary depending on the skill and experience of the provider performing the laryngoscopy. It is less accurate in cases of difficult laryngoscopy when there is a limited view of the glottic opening as a result of anatomic distortion or the presence of secretions, vomitus, or blood. It may be more accurate with the use of indirect laryngoscopy (e.g., video-assisted laryngoscopy [VAL]) given the improved glottic view compared with line-of-sight techniques such as direct laryngoscopy (DL). The benefits of VAL are more prominent when dealing with difficult intubations and in cases with limited glottic visualization (i.e., Cormack-Lehane grades III or IV). The improved view afforded by VAL can turn blind intubation into successful intubation under visual control ( Fig. 30.1 ). In a recent meta-analysis, De Jong and colleagues compared DL with VAL in the critical care setting. They reported a reduction of difficult intubation by 29%, a decrease in the incidence of Cormack-Lehane grade III or IV views by 26%, and a decrease the incidence of EI by 14%. Mosier and colleagues compared VAL use with DL and found that the first-attempt success rate for VAL was 78.6% versus 60.7% and that the use of VAL reduced the EI rate from 12.5% with DL to 1.3%. Kory and colleagues reported a 14% incidence of EI with the use of DL compared with 0% for VAL in a cohort of critical care patients.
Routine auscultation at one or two points on each side of the chest and over the epigastrium is recommended to establish proper ETT placement and position. Auscultation is widely used and is a cost-effective and straightforward method to confirm ETT placement; however, it also has its limitations. Anecdotal reports show that errors during auscultation constitute a significant source of litigation and a cause of undetected accidental EI. In the 1990 ASA closed claims analysis, Caplan noted that auscultation was reported as normal in 48% of cases involving EI. Normal breath sounds can be transmitted to the epigastric area, and gastric sounds can be transmitted to the chest wall, resulting in false-negative and false-positive readings, respectively. Esophageal sounds (sounds generated when the ETT enters the esophagus) can be transmitted to the chest wall of smaller patients because of the anatomic proximity of the esophagus and trachea in children and may be misinterpreted as pulmonary in origin. Normal breath sounds can also be easily transmitted to the epigastrium (mainly when uncuffed ETTs are used), potentially leading to an erroneous diagnosis of EI. In cases of hiatal hernia, gastric pull-through, diaphragmatic hernia, or gastric distention, the presence of gastric viscera in the thoracic cavity can predispose practitioners to a false determination of respiratory tract placement after EI.
Auscultation is also limited in detecting mainstem intubation; breath sounds from one lung can be transmitted to the opposite side of the chest in the case of mainstem intubation. Other limitations of auscultation include its operator dependency, and its greater accuracy when performed by experienced providers. In a study set in the intensive care unit (ICU), Knapp and colleagues demonstrated that experienced examiners were correct in all attempts at auscultation to determine the presence of the ETT in the trachea or in the esophagus, but inexperienced examiners were incorrect in 32% of cases. Auscultation is limited in noisy environments or when dealing with morbidly obese, cachectic, or pediatric patients. Air rescue missions, because of the high ambient noise and the requirement to wear helmets during flight, demand specialized equipment. In two reports by Grmec, auscultation was less sensitive and specific to detect proper ETT placement than end-tidal CO 2 (EtCO 2 ) during emergency intubations in the field. Although it is encouraged that all providers attempt to detect proper ETT placement with the help of auscultation, it is recommended that other secondary methods be performed routinely given the inherent limitations of this method.
Although the presence of water vapor condensation is a sign many intubation practitioners routinely rely upon, and it may indicate the presence of the ETT in the respiratory tract, it is not a reliable indicator to rule out EI or to confirm adequate ETT depth within the trachea. Cases of ETT humidification despite EI have been reported, and the presence of ETT fogging cannot establish correct midtracheal positioning of an ETT. In an animal study, Kelly and colleagues detected ETT humidification in 83% of tubes placed in the esophagus and concluded that the presence of condensation should not be used as the sole clinical indicator to determine correct ETT placement.
Abdominal distention versus symmetric chest movements with positive pressure ventilation can distinguish between esophageal and tracheal intubation in normal circumstances; however, in obese patients, obstetric patients, patients with large breasts, patients with chest wall pathology, or when there is an alteration of lung compliance, neither abdominal distention nor chest wall movement is a reliable clinical sign of adequate ETT placement and position. Likewise, as can occur with auscultation (see Auscultation), the presence of gastric viscera in the thoracic cavity can lead to thoracic movement despite EI, which can therefore be misinterpreted as proper ETT placement. Gastric distention could occur during mask ventilation and be subsequently mistaken for EI after intubation. Prior placement of a gastric drainage tube (i.e., an oral or nasogastric tube) can lead to decompression and, therefore, decrease the reliability of gastric distention as a clinical sign of accidental EI.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here