Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The concept of fibrohistiocytic neoplasms has been challenged largely because the malignant forms (i.e., malignant fibrous histiocytoma) consistently lack histiocytic features, and because some, when carefully studied, show a subtle degree of differentiation. Nonetheless, many benign fibrohistiocytic lesions are truly derived from histiocytes (e.g., solitary xanthogranuloma, xanthoma), so there remains some merit in retaining this category. This has been endorsed by the World Health Organization (WHO), recognizing that use of the term “fibrohistiocytic” is descriptive and merely denotes a lesion composed of cells that resemble normal histiocytes and fibroblasts.
Benign fibrohistiocytic tumors, however, are a pathogenetically diverse group of lesions. Xanthoma is a “pseudotumor” that usually arises in response to a disturbance in serum lipids. The preponderance of evidence suggests fibrous histiocytoma is a true neoplasm with a definite growth potential but a limited capacity for aggressive behavior. Between these extremes are lesions of an indeterminate nature, exemplified by solitary xanthogranuloma. Although solitary xanthogranuloma resembles a tumor morphologically, it usually regresses with time, questioning its proper position in the spectrum between hyperplasia and neoplasia. The present classification represents a practical, rather than a conceptual, approach to defining differences among several histologically similar lesions ( Box 10.1 ).
Forms of histiocytosis X
Eosinophilic granuloma
Hand-Schüller-Christian disease
Others
Hemophagocytic lymphohistiocytosis
Infection-associated hemophagocytic syndrome
Sinus histiocytosis with massive lymphadenopathy
Solitary xanthogranuloma
Reticulohistiocytoma
Acute monocytic leukemia
Malignant histiocytosis
True histiocytic lymphomas
Fibrous histiocytoma is a neoplastic lesion composed of a mixture of fibroblastic and histiocytic cells arranged in sheets or short fascicles and accompanied by varying numbers of inflammatory cells, foam cells, and siderophages. This tumor usually occurs in the dermis and superficial subcutis and rarely in deep soft tissues. When located in the skin, fibrous histiocytoma is also referred to as dermatofibroma . In this chapter we use the all-inclusive term fibrous histiocytoma to refer to lesions of the dermis and soft tissue. The terms histiocytoma cutis, nodular subepidermal fibrosis, and sclerosing hemangiomas, once used as synonyms for fibrous histiocytomas, are now archaic.
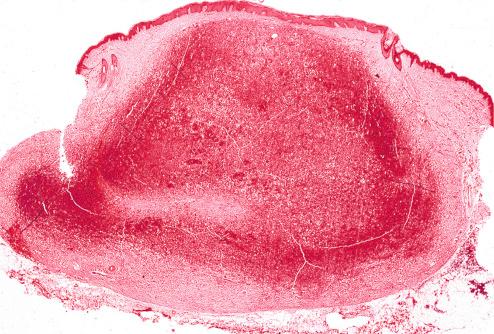
Cutaneous fibrous histiocytoma is a solitary, slowly growing nodule that usually makes its appearance during early or middle adult life. A subset has been reported to occur following minor trauma or insect bites. Although any part of the skin surface may be affected, it is most common on the extremities. Approximately one-third of these tumors are multiple and present metachronously. Synchronous development can occur in the setting of immunosuppression, particularly systemic lupus erythematosus. Cutaneous fibrous histiocytomas are elevated or pedunculated lesions measuring from a few millimeters to a few centimeters in diameter ( Figs. 10.1 to 10.3 ). Rarely, they result in a depressed area in the skin (“atrophic dermatofibroma”). They impart a red to red-brown to blue-black color to the overlying skin. Although usually ascribed to the presence of hemosiderin, epidermal hyperpigmentation has recently been attributed to lesional expression of stem cell factor and an increase in tyrosinase-positive melanocytes. Such lesions may be confused clinically with malignant melanoma. The presence of a central dimple on lateral compression is regarded as a useful clinical sign for distinguishing it from melanoma. Deeply situated fibrous histiocytomas are less common than cutaneous ones. The relative incidence is difficult to determine because cutaneous lesions are less likely to be subjected to biopsy or excised than deep ones. In a study by Fletcher, only three cases of fibrous histiocytoma involving skeletal muscle were culled from more than 1000 fibrohistiocytic tumors. As with their cutaneous counterparts, they present as painless masses, usually on an extremity. Rarely, deep fibrous histiocytomas may occur in retroperitoneal, mediastinal, and pelvic soft tissue. Although they develop at any age, most occur between 20 and 40 years. They tend to be larger than the cutaneous tumors. Fibrous histiocytomas involving skeletal muscle and visceral soft tissue locations are often large, 5 cm or more, in contrast to their cutaneous and subcutaneous counterparts, which are usually 3 cm or less. Grossly, they are circumscribed, yellow or white masses that may have focal areas of hemorrhage.



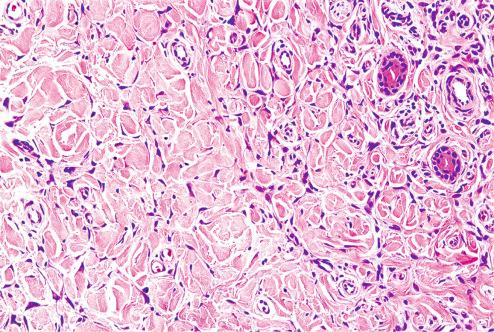
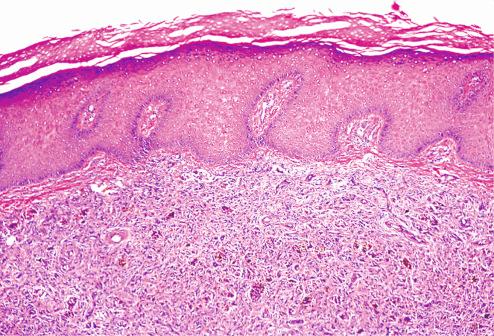
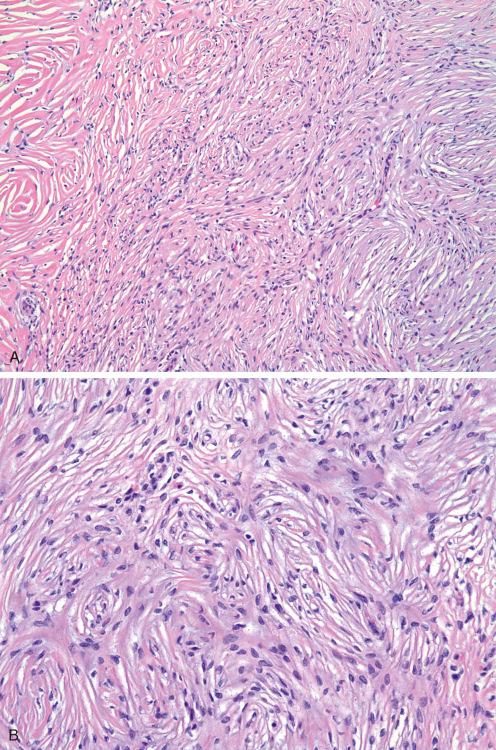
The cutaneous fibrous histiocytoma consists of a nodular cellular proliferation involving dermis and occasionally subcutis ( Fig. 10.4 ). The tumor is not sharply defined laterally and typically interdigitates with dermal collagen (“collagen trapping”) ( Fig. 10.5 ). The overlying epidermis frequently shows some degree of hyperplasia, including acanthosis or elongation and widening of the rete pegs ( Fig. 10.6 ). Hyperplasia of other adnexal structures may also be seen, sometimes forming intralesional epithelial cysts. The presence of a rim of normal dermis between epidermis and tumor is variable. At the deep margin, the tumor extends small tentacles for a short distance into the subcutis ( Fig. 10.7 ) or, less often, has a smoothly contoured margin ( Fig. 10.8 ). Both patterns contrast with the diffusely infiltrating border of dermatofibrosarcoma protuberans. Most cutaneous fibrous histiocytomas consist of short, intersecting fascicles of lightly eosinophilic fibroblastic cells ( Figs 10.9 to 10.15 ). The fascicles usually form a loose crisscross pattern or a vague storiform pattern ( Fig. 10.9 ). Occasional rounded “histiocytic” cells accompany the spindle cells, but they rarely predominate. Multinucleated giant cells of the foreign body or Touton type are a typical feature of this form of fibrous histiocytoma and often contain phagocytosed lipid and hemosiderin ( Figs. 10.12 and 10.14 ). Inflammatory cells, particularly lymphocytes and xanthoma cells, are scattered randomly throughout the tumors but vary greatly in number. Small aggregates of lymphocytes are often seen adjacent to foci of subcutaneous fat involvement. The stroma consists of a delicate collagen network surrounding individual cells. In a few cases, the vessels and stroma exhibit striking hyalinization ( Fig. 10.13 ). Cystic areas of hemorrhage are common and, when prominent, result in large accumulations of hemosiderin in the tumor cells. When this feature is striking, some have employed the terms “siderotic” or “aneurysmal” fibrous histiocytoma (see later). Other unusual features seen in these lesions include clear cell change, granular cell change, nuclear palisading, extensive hyalinization, lipidization, and smooth muscle hyperplasia.
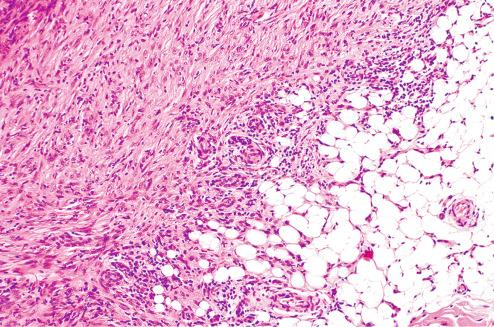
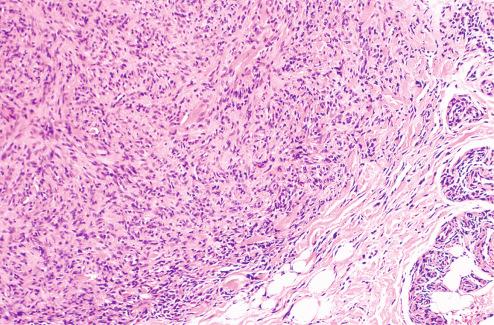
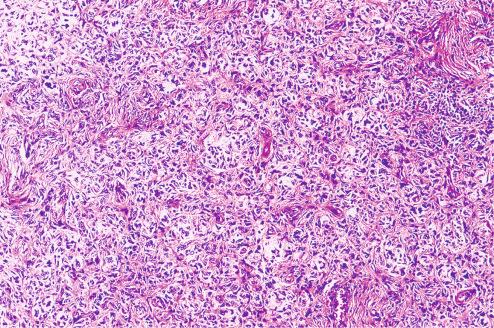
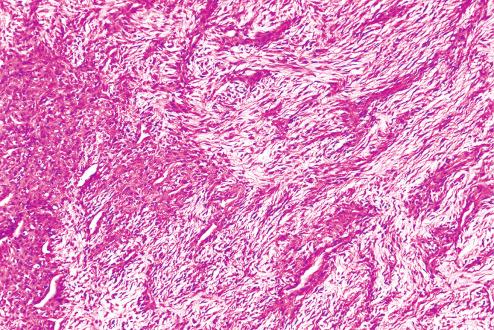
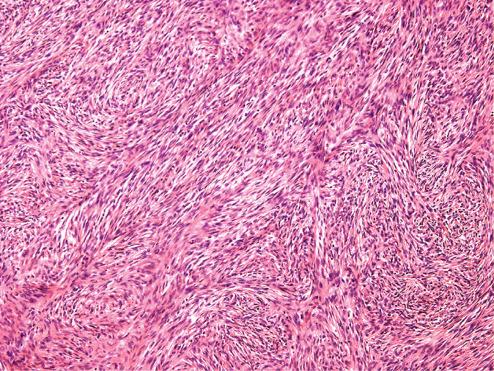
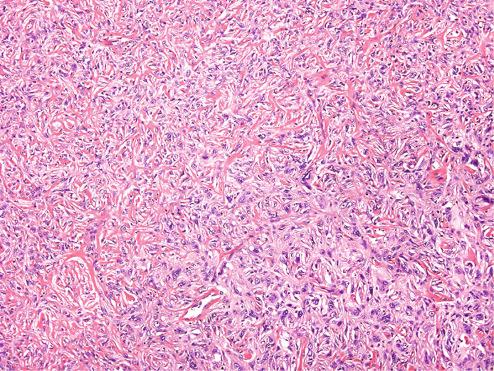
Deep fibrous histiocytomas are similar to their cutaneous counterparts but usually have a more prominent storiform pattern and fewer secondary elements such as xanthoma cells ( Figs. 10.16 to 10.18 ). The stroma often undergoes myxoid change ( Fig. 10.17 ) or hyalinization. In unusual cases, dense bundles of collagen ( amianthoid fibers ) and even metaplastic osteoid are detected. Not infrequently, deep fibrous histiocytomas blend with areas indistinguishable from a benign solitary fibrous tumor ( Fig. 10.18 ). This combination of pericytic and fibrohistiocytic areas is particularly characteristic of fibrous histiocytomas of the orbit.
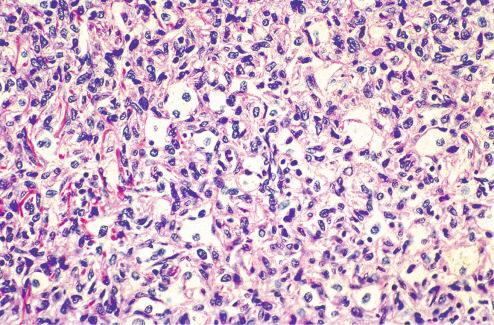
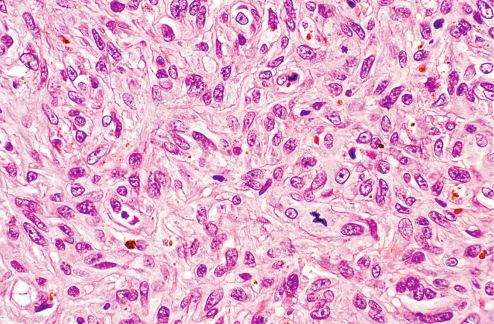
The benign nature of fibrous histiocytoma is usually apparent histologically. The cells are well differentiated and exhibit little pleomorphism and usually little or no mitotic activity ( Fig. 10.19 ). The occasional pleomorphic cells with hyperchromatic nuclei and clear to eosinophilic cytoplasm ( Fig. 10.20 ), sometimes called “monster cells,” within an otherwise typical fibrous histiocytoma seem to be a degenerative phenomenon and do not affect the prognosis adversely. However, the presence of both pleomorphism and mitotic activity suggests a more aggressive lesion, either atypical fibrous histiocytoma or superficial undifferentiated pleomorphic sarcoma. Cellular fibrous histiocytomas are characterized by somewhat longer, cellular fascicles of spindle cells bereft of other cellular elements (e.g., siderophages, giant cells). Although benign, these lesions are thought to have a higher local recurrence rate than other forms of fibrous histiocytoma, as discussed later.
It is well recognized that clinically benign fibrous histiocytomas may occasionally show morphologic features associated with malignancy in other tumor types, such as increased cellularity, necrosis, vascular invasion, mitotic activity, and cytologic atypia. Therefore, it is important to recognize the underlying nature of the lesion to know what significance to place on these features. A useful guideline is that benign fibrous histiocytomas may show enhanced cellularity and some level of mitotic activity (e.g., cellular fibrous histiocytoma) and may still be considered benign. Likewise, benign fibrous histiocytomas may display nuclear atypia on a degenerative basis in the form of large “monster” cells set amidst the typical backdrop of banal neoplastic cells. Such lesions also are clinically benign. The presence of both mitotic activity and atypia (especially atypical mitotic figures) in a lesion clearly showing areas of conventional fibrous histiocytoma characterizes “atypical fibrous histiocytomas.” The diagnosis of atypical fibrous histiocytoma should not be used for lesions without clear areas of conventional fibrous histiocytoma; such lesions are likely to represent either atypical fibroxanthoma or superficial undifferentiated pleomorphic sarcoma.
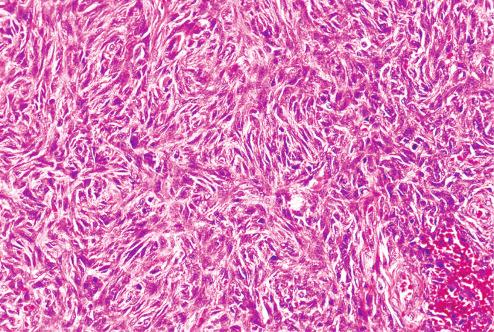
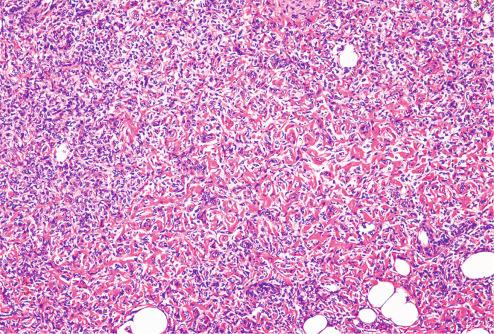
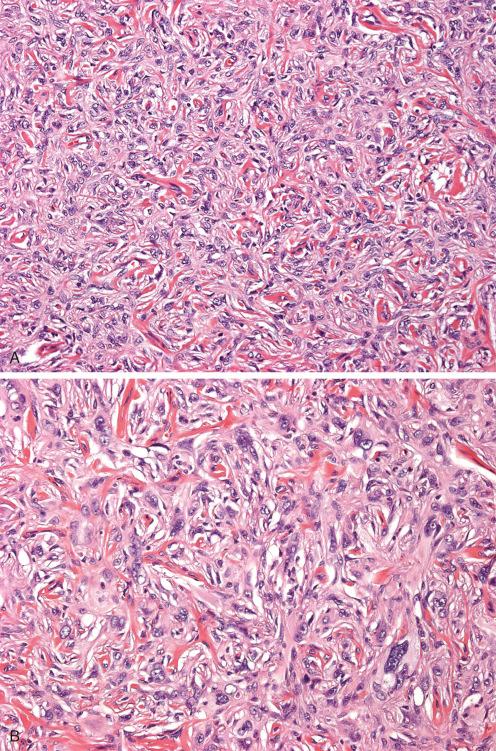
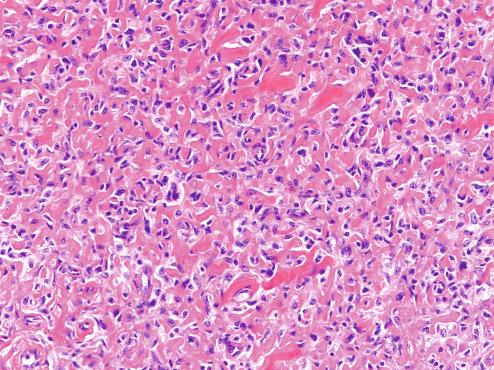
Cellular fibrous histiocytomas occur in a similar age range and in similar locations as ordinary fibrous histiocytomas. They are characterized by increased cellularity, a predominantly fascicular growth pattern, and a relative paucity of giant cells, siderophages, and foamy macrophages ( Figs. 10.21 and 10.22 ). Some cellular fibrous histiocytomas have been reported as “dermatofibroma with subcutaneous extension” and “dermatofibroma with potential for local recurrence.” Mitotic activity is usually somewhat higher (mean: 3 mitoses per 10 high-power fields [hpf]) and subcutaneous extension more common (30%) than in the usual fibrous histiocytoma. About 10% undergo spontaneous central necrosis, a phenomenon that in our experience seems to be particularly common in tumors in younger patients and in the hands and feet. Cellular fibrous histiocytomas have been reported to recur in up to 25% of cases; it is unclear whether this is a reflection of these lesions’ relatively high cellularity or their more frequent involvement of the subcutaneous adipose tissue. We generally recommend complete excision showing negative margins for cellular fibrous histiocytomas to reduce the risk of local recurrence.
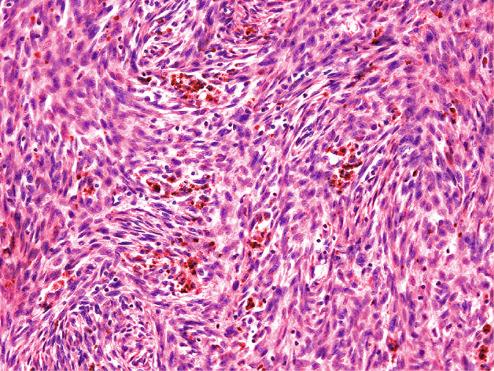
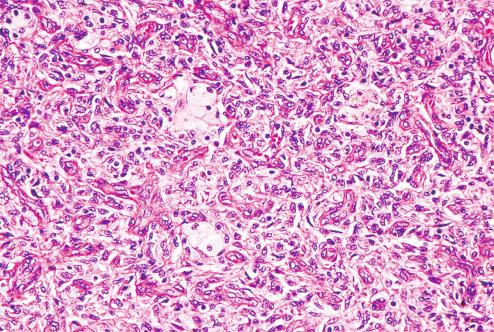
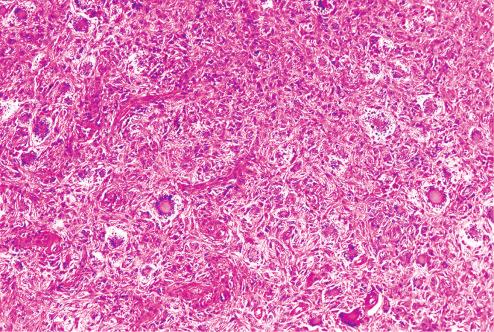
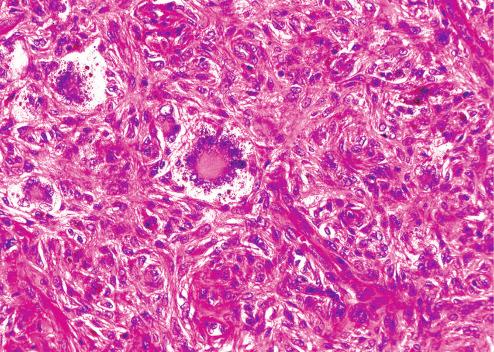
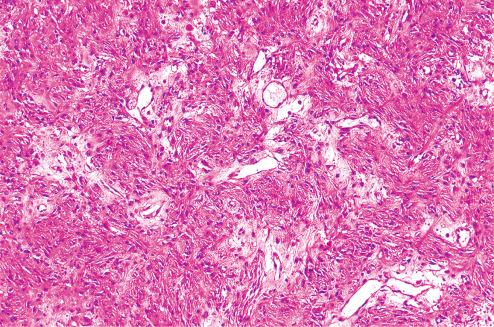
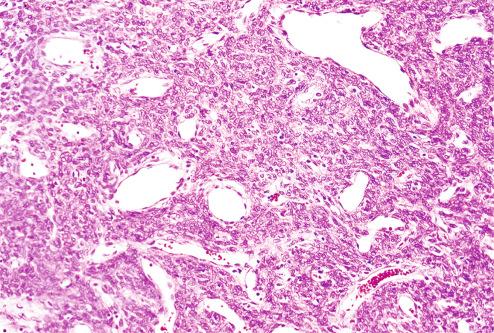
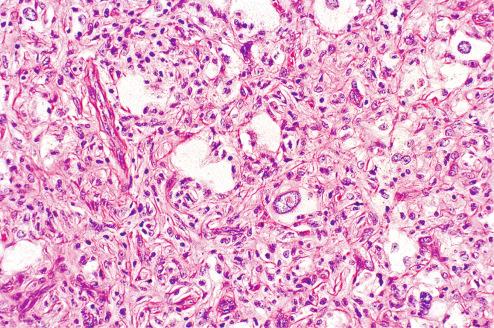
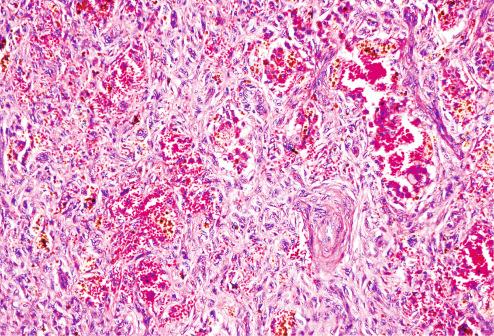
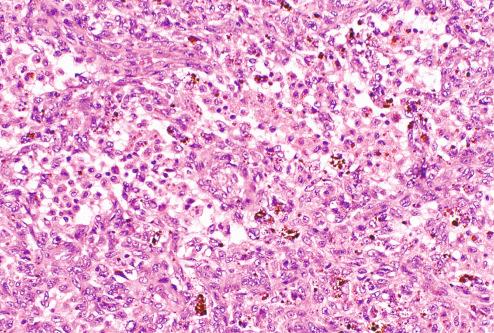
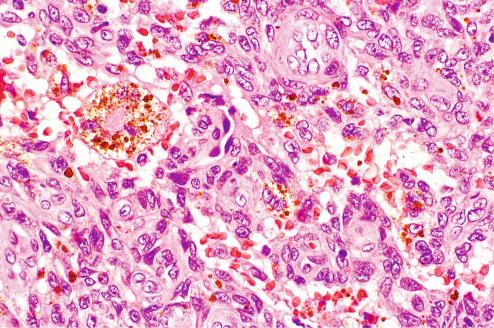
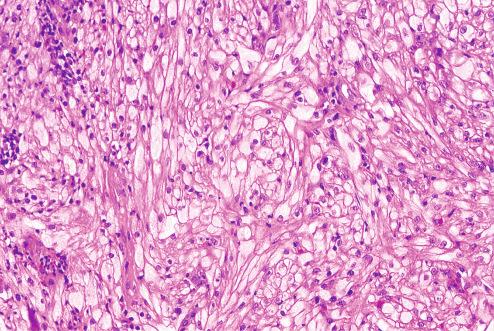
Approximately 1% to 2% of benign fibrous histiocytomas undergo extensive cystic hemorrhage. These aneurysmal fibrous histiocytomas are significant because they can evolve rapidly as a result of spontaneous intralesional hemorrhage. Their blue to black color suggests the clinical diagnosis of a vascular or melanocytic tumor. Aneurysmal fibrous histiocytomas may also achieve very large size at diagnosis. At low power, these lesions contain large, blood-filled spaces lined by discohesive fragments of tumor rather than endothelium ( Figs. 10.23 to 10.26 ). Hemosiderin may be abundant, and mitotic activity is often noted in the immediate vicinity of the hemorrhage. The cells of aneurysmal fibrous histiocytomas are typically plump and grow in “tight” storiform arrays. A 20% recurrence rate has been reported for these tumors, which in our experience likely overstates their locally recurring potential. Despite the similarity of names, the aneurysmal fibrous histiocytoma should be clearly distinguished from the angiomatoid (malignant) fibrous histiocytoma of childhood , a subcutaneous lesion often associated with systemic symptoms (see Chapter 11 ).

A very small number of fibrous histiocytomas have borderline histologic features that include significantly more atypia and mitotic activity than encountered in the usual type. Kaddu et al. coined the term “atypical fibrous histiocytomas” for these lesions. They differ from atypical fibroxanthoma/superficial undifferentiated pleomorphic sarcomas in their predilection for younger individuals (mean: 38 years) and in a distribution that favors the extremities rather than the sun-exposed surfaces of the face and neck. The average size is less than 2 cm. The majority are restricted to the dermis, with superficial subcutaneous involvement in one-third of cases. The diagnosis of atypical fibrous histiocytoma should be applied only to cases that have a clear-cut background of classic fibrous histiocytoma but display areas of more generalized atypia than the occasional monster cell and show increased mitotic activity, including atypical forms ( Figs. 10.27 and 10.28 ). Information in 21 patients followed for approximately 4 years disclosed local recurrences in three patients and distant metastases in two, one of whom died (see later, Metastasizing Fibrous Histiocytomas).
The rare and minor variants of benign fibrous histiocytoma are principally important in that they evoke a somewhat different list of diagnostic considerations. Zelger et al. described a “clear cell dermatofibroma” in which most of the cells underwent a translucent clear-cell change ( Fig. 10.29 ). This lesion must be distinguished from clear cell carcinomas, melanocytic tumors, and perivascular epithelioid cell neoplasms involving the skin. The cells may be positive for factor XIIIa but not for melanocytic antigens. Lipidized (ankle-type) fibrous histiocytoma, typically a lesion of the lower leg, particularly ankle, is usually larger than the usual fibrous histiocytomas and is characterized by foamy histiocytes situated within a hyalinized collagenous or osteoid-like stromal backdrop ( Fig. 10.30 ). Fortuitous palisading of nuclei (“palisaded fibrous histiocytoma” ), extensive myxoid change (“myxoid dermatofibroma” ), and granular cell change have also been noted in fibrous histiocytomas.
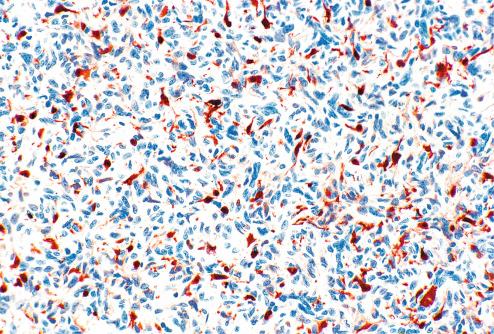
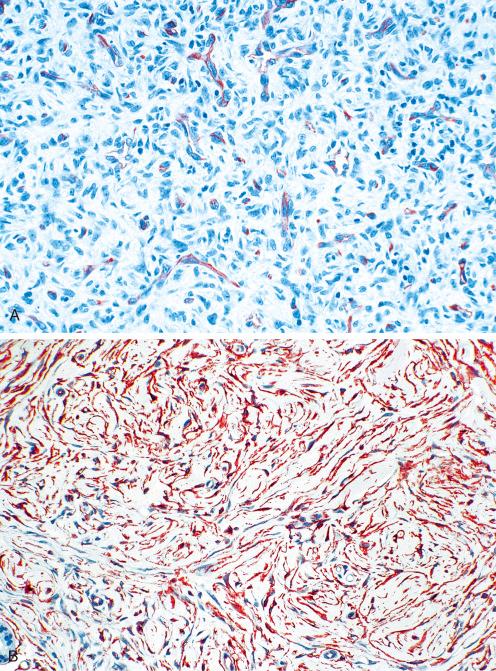
The majority of fibrous histiocytomas displays immunostaining for factor XIIIa in a significant population of cells, leading some to conclude that these tumors arise from dermal dendrocytes ( Fig. 10.31 ). Whether factor XIIIa stains tumor elements or reactive dermal dendrocytes that populate benign fibrous histiocytomas is a matter of debate. In our experience, factor XIIIa immunolabeling is frequently absent in the neoplastic cells in fibrous histiocytomas, in particular cellular fibrous histiocytomas, and the practical utility of this marker is questionable. Furthermore, factor XIIIa is present in many other mesenchymal lesions, and its presence is not diagnostic of fibrous histiocytomas. The combination of factor XIIIa and CD34, however, is typically used to distinguish benign fibrous histiocytoma from dermatofibrosarcoma protuberans (see Differential Diagnosis). Myoid markers (e.g., desmin, smooth muscle myosin ) are occasionally present in fibrous histiocytomas, in particular cellular fibrous histiocytomas, and are indicative of limited myofibroblastic differentiation, a finding of no clinical significance. These findings should not be construed as evidence of a smooth muscle neoplasm. Fibrous histiocytomas also tend to contain other cell types, including dermal interstitial cells (CD34 positive), Langerhans cells (S-100 protein positive), and macrophages (CD68 and CD163 positive), and the presence of multiple cell types is perhaps the most characteristic immunohistochemical aspect of these tumors.
Although the reactive versus neoplastic nature of fibrous histiocytomas was the subject of considerable debate for years, the great preponderance of evidence now indicates neoplastic origin for these tumors. The clonality of fibrous histiocytomas has been demonstrated by a variety of different methods in 30% to 100% of cases examined. In 2014, Plaszczyca et al., using a variety of different molecular genetic techniques, including next-generation sequencing, demonstrated recurrent gene fusions in six of eight fibrous histiocytomas involving membrane-associated proteins including podoplanin (PDPN), CD63, and LAMTOR1 with protein kinase C isoforms (PRKCB and PRKCD). Two other cases in this series had karyotypic abnormalities (translocations) but could not be analyzed by molecular methods. Subsequently, LAMTOR-PRKCD , NUMA1-SFMBT1, and KIRREL-PRKCA fusions as well as PRKCB or PRKCD rearrangements have been identified in fibrous histiocytomas of various types and in both superficial and deep locations.
Array-based comparative genomic hybridization techniques show a high frequency of chromosomal aberrations in metastasizing and atypical fibrous histiocytomas, including gains of chromosomes 7 and 8q and loss of Xq in metastasizing fibrous histiocytomas and losses of 9 and 22 in atypical fibrous histiocytomas. In contrast, typical cellular fibrous histiocytomas show only rare gains in chromosome 20. Metastasizing fibrous histiocytomas frequently contain comparative genomic hybridization (CGH) aberrations.
Some generalizations can be made concerning the clinical behavior of fibrous histiocytomas. Fewer than 5% of cutaneous fibrous histiocytomas recur following local excision. In our experience, the overall recurrence rate of cutaneous and soft tissue fibrous histiocytomas is approximately 10% after conservative therapy. Those located in deep soft tissue have a somewhat higher recurrence rate that reflects larger size and incomplete surgical excision. Franquemont et al. reported a recurrence rate of almost 50% for fibrous histiocytomas (eight cases) that extended into the subcutis or grew in a multinodular fashion (or both). Font and Hidayat noted that 57% of orbital fibrous histiocytomas with infiltrative margins or hypercellular zones (or both) recurred, compared with 31% of those without these features. Mentzel et al. likewise stated that facial fibrous histiocytomas, which frequently invade subcutis and muscle, have a high rate of recurrence. Most recently, Gleason et al. documented a 22% local recurrence rate in deep fibrous histiocytomas. As previously noted, cellular and aneurysmal fibrous histiocytomas have been reported historically to recur locally in approximately 20% to 25% of cases. We suspect that the local recurrence rate is now considerably lower, since most cellular and aneurysmal fibrous histiocytomas are reexcised following initial diagnosis, in our experience.
Exceptionally rare cases of histologically benign fibrous histiocytomas have produced metastases, a phenomenon first reported in two cases by Colome-Grimmer and Evans. Both were small (2 cm) cutaneous lesions that recurred, produced regional lymph node metastasis, and ultimately metastasized to the lung. The metastases appeared similar to the primary lesions, and both patients were alive 4 and 8 years after resection of the pulmonary deposits. Guillou et al. described three patients with fibrous histiocytomas of the aneurysmal, cellular, or atypical types who developed regional lymph node metastases but who had a protracted course and favorable outcome. Rare metastases have also been reported in association with otherwise typical deep fibrous histiocytomas. Two larger series of metastasizing fibrous histiocytomas have recently been reported. Doyle and Fletcher reported 16 cases with metastases, including 11 cellular, 2 aneurysmal, 1 atypical, and 1 epithelioid fibrous histiocytoma. Of these, 10 cases had recurred locally, including four patients with multiple recurrences. Metastases occurred a median of 17 months after initial diagnosis and involved lungs, lymph nodes, soft tissue and liver; six patients died of disease. Although the primary tumors in this series tended to be large and cellular, they did not have histologic features that would have predicted metastasis, and the histologic features were similar in primary and metastatic sites. Similar findings were reported in another series of seven metastasizing fibrous histiocytomas.
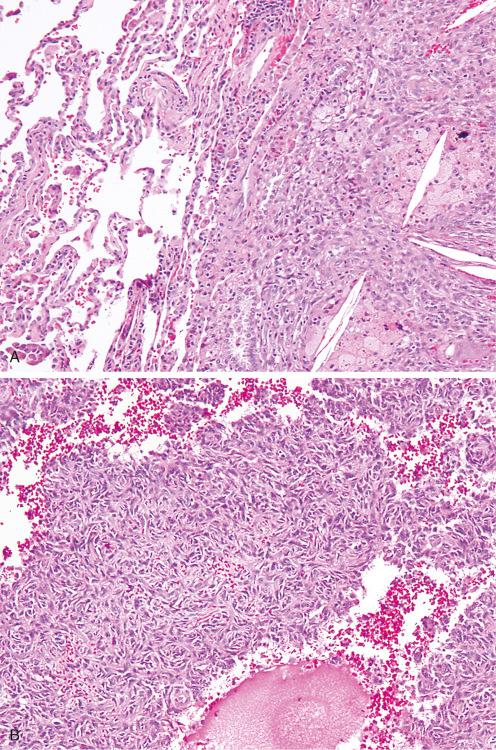
As noted earlier, CGH copy number aberrations are relatively common in fibrous histiocytomas that have subsequently metastasized, although study of a much larger number of cases is necessary before this technique can be recommended for the routine evaluation of fibrous histiocytomas. Cases described in the pulmonary pathology literature as “cystic fibrohistiocytic lesions” of the lung also appear to represent examples of metastasizing fibrous histiocytoma. We too have seen instances of pulmonary metastasis from benign cutaneous fibrous histiocytomas in which the metastases also appeared histologically identical to the primary ( Fig. 10.32 ). From a practical perspective, we do not mention the risk of metastasis in benign fibrous histiocytomas in our diagnostic reports, since this would create unnecessary concern for the vast majority of patients with this disease. These are best regarded as benign neoplasms with a vanishingly small risk of metastasis rather than mesenchymal tumors of borderline (intermediate) malignancy.
Fibrous histiocytomas are most frequently confused with other benign lesions, notably nodular fasciitis, neurofibroma, leiomyoma, and storiform collagenoma. Although nodular fasciitis may display a storiform pattern, it is distinguished from fibrous histiocytoma by its loosely arranged bundles of myofibroblasts. Cellular areas containing proliferating myofibroblasts alternate with loose myxoid zones containing extravasated red blood cells and inflammatory cells. The vasculature in fasciitis is seldom as orderly or as uniform as that of fibrous histiocytoma. Finally, because most cases of fasciitis are excised during the period of active growth, they usually manifest much more mitotic activity than a fibrous histiocytoma of comparable cellularity. In our experience, it is difficult, if not impossible, to distinguish the early (cellular) phase of nodular fasciitis from a benign fibrous histiocytoma. Fortunately, from a practical point of view, this diagnostic imprecision has little adverse effect on patient care. The distinction between a fibrous histiocytoma and a neurofibroma is usually not difficult. Neurofibromas contain a population of Schwann cells expressing S-100 protein and/or SOX10 and having serpentine nuclei. Additional features of neural differentiation may include organoid structures reminiscent of sensory receptors or vague nuclear palisading. The usual lack of any storiform pattern or significant inflammation in neurofibromas further underscores the difference between the two tumors. Sclerotic forms of leiomyoma may resemble a fibrous histiocytoma. However, smooth muscle tumors have a more distinct fascicular growth pattern. Their blunt-ended nuclei are plumper, and the cytoplasm typically has longitudinal striations corresponding to the presence of myofilamentous material, which can be accentuated with Masson trichrome stain. They strongly express smooth muscle actin (SMA) and muscle-specific actin in a diffuse pattern, unlike the focal immunoreactivity noted in benign fibrous histiocytomas reflective of myofibroblastic differentiation. Caldesmon and desmin expression are also characteristic of leiomyoma, but not fibrous histiocytoma. Lastly, the rare storiform collagenoma (sclerotic fibroma) resembles a fibrous histiocytoma or dermatofibrosarcoma protuberans by virtue of its striking storiform pattern. However, these small, dermal nodules, which are composed principally of plates of collagen separated by cleftlike spaces, lack the cellularity of either of the previous tumors. In their multifocal form, storiform collagenomas may be associated with Cowden syndrome ( Fig. 10.33 ).
Most importantly, fibrous histiocytoma must be distinguished from dermatofibrosarcoma protuberans (DFSP). As with fibrous histiocytoma, DFSP occurs in the dermis and subcutis but typically displays extensive subcutaneous involvement in the form of long, penetrating tentacles of tumor. It is also characterized by a more uniform cellular population and lacks overlying epidermal hyperplasia, giant cells, inflammatory cells, and xanthomatous elements. Its fascicles, composed of slender attenuated cells, are longer and arranged in a distinct storiform pattern, unlike the short curlicue fascicles of fibrous histiocytoma. Its margins are highly infiltrative, in contrast to the better-defined margins of fibrous histiocytoma. Although fibrous histiocytomas may occasionally show limited extension into the subcutis, this is in the form of bulbous protrusions, rather than the diffuse, honeycomb pattern seen in DFSP. Immunostaining reveals distinct differences in the cellular composition of these tumors as well. In contrast to fibrous histiocytomas, which typically consist of an admixture of factor XIIIa, CD34, S-100 protein, SMA, and CD68-positive cells, DFSP is composed essentially entirely of CD34-positive spindled cells ( Fig. 10.34 ). Many fibrous histiocytomas, in particular cellular forms, also show a reactive component of CD34-positive cells, frequently present at the deep and lateral borders of the lesion, and care should be taken not to misinterpret this as evidence of DFSP. Those lesions previously described as “indeterminate fibrohistiocytic lesions” of the skin likely represent such cases, rather than a distinct entity. Careful histologic evaluation and CD34 immunostaining (sometimes with the addition of factor XIIIa) should be sufficient for the distinction of fibrous histiocytoma and DFSP in the great majority of cases. Other markers reported of value in this differential diagnosis include podoplanin (D2-40), HMGA1, and HMGA2 (positive in fibrous histiocytoma but not DFSP), and ApoD1 (positive in DFSP but not fibrous histiocytoma).
The difference between benign fibrous histiocytomas and superficially located undifferentiated pleomorphic sarcomas is usually obvious because the latter is a pleomorphic, predominantly subcutaneous tumor with numerous typical and atypical mitotic figures and prominent areas of hemorrhage and necrosis. Less obvious is the difference between aneurysmal and angiomatoid (malignant) forms of fibrous histiocytoma. The latter is a distinctive, pediatric, translocation-associated mesenchymal tumor of uncertain lineage, characterized by sheets of histiocytic cells interrupted by cystic areas of hemorrhage. They are surrounded by a dense cuff of lymphocytes and plasma cells but almost never have giant cells or xanthoma cells, as does the aneurysmal variant of fibrous histiocytoma.
Dermatomyofibroma, originally described as “haemorrhagic dermatomyofibroma” (plaquelike dermal fibromatosis), is an uncommon benign cutaneous tumor showing fibroblastic and myofibroblastic differentiation. Fewer than 100 cases have been reported.
Dermatomyofibroma occurs much more often in women than men, with a mean patient age of 30 years. Cases occurring in pediatric patients have been reported as well. The tumors most often involve the shoulder, neck, and trunk but may occur in a variety of locations. Clinically, dermatomyofibromas present as linear, plaquelike, and sometimes hemorrhagic lesions, mimicking a wide variety of neoplastic and nonneoplastic diseases of the skin. Microscopically, the lesions consist of poorly defined, plaquelike proliferation of well-differentiated, cytologically bland (myo)fibroblastic spindled cells, typically oriented parallel to the overlying epidermis ( Fig. 10.35 ). Most tumors are confined to the dermis, although limited subcutaneous involvement can be seen as well. Nuclear atypia and mitotic activity are absent. Despite their name, dermatomyofibromas show myofibroblastic differentiation in the form of SMA expression in a minority of cases, with only 11 of 48 cases expressing this marker in the largest reported series to date. Dermatomyofibromas are entirely benign, with only rare local recurrences.
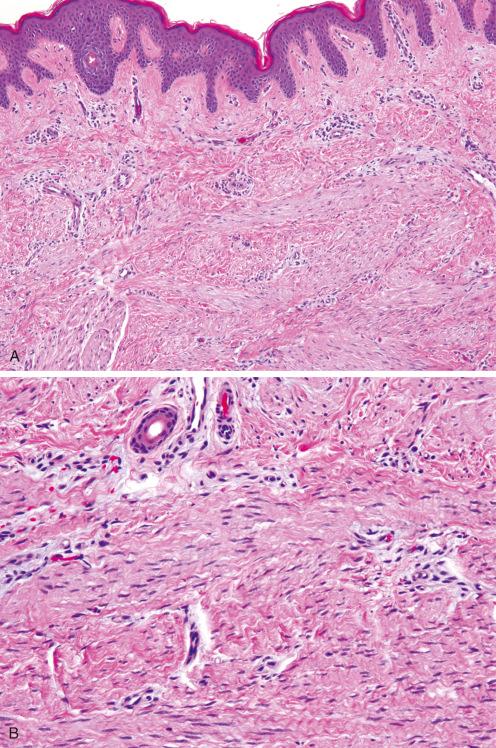
Dermatomyofibromas differ from typical fibrous histiocytomas ( dermatofibromas ) in that they lack epidermal hyperplasia, peripheral collagen trapping, and siderophages/giant cells; consist of a more uniform proliferation of spindled cells oriented parallel to the epidermis; and contain increased amounts of dermal elastic fibers. Although dermatomyofibromas may show limited CD34 expression, they lack the storiform growth pattern and infiltrative growth pattern seen in DFSP. Cutaneous involvement is very rare in desmoid-type fibromatoses , which typically present as larger, deeply situated lesions, showing longer fascicles of myofibroblastic cells.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here