Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Developmental abnormalities of the skin are a diverse group of anomalies representing errors in morphogenesis. By definition, they are present at birth, although some are not evident in the neonatal period, but most present during infancy. They vary in severity from the inconsequential to the serious and, in some instances, represent a marker for significant extracutaneous anomalies.
Accessory mammary tissue (supernumerary nipples, accessory nipple, polythelia, polymastia) may consist of true glandular tissue (accessory breasts), areola, nipples, or a combination thereof. It is often bilateral and found along the course of the embryologic breast lines, which run from the axilla to the inner thigh. Accessory nipples are the most common variant, occurring in as many as 2% of females, manifesting clinically as soft, brown, pedunculated papules ( Fig. 9.1 ). In the newborn, the lesions are often very subtle, appearing as a light brown or pearly 1–3 mm macule. Familial occurrence has been reported.

It has been suggested that renal and urogenital malformations occur with increased frequency in infants with polythelia, although the results of published studies are conflicting, with incidence figures ranging from zero to approximately 10%.
The diagnosis is usually made clinically but may be confirmed by histologic demonstration of mammary tissue. An accessory nipple will show epidermal thickening, pilosebaceous structures, and smooth muscle, with or without true mammary glands. The differential diagnosis includes melanocytic nevus, neurofibroma, verruca, or skin tag.
Complete surgical excision is usually recommended if there is glandular tissue because enlargement at puberty may cause pain and embarrassment. Small accessory nipples need not be excised. Breast carcinoma has also been reported in ectopic mammary tissue in an adult.
The auricle is formed by fusion of six tubercles derived from the first and second branchial arches. Incomplete fusion may lead to entrapment of epithelium, forming cysts that communicate to the skin surface through sinuses. If the cyst and sinus are obliterated, a pit is left behind. Preauricular pits are common and may be inherited in an autosomal dominant fashion. They manifest as small depressions at the anterior margin of the ascending limb of the helix ( Fig. 9.2 ).
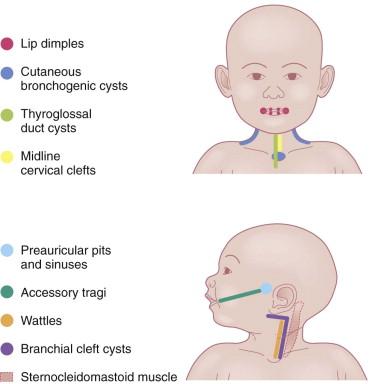
Preauricular cysts present as tender swellings in the preauricular region; occasionally they are bilateral. If there is a sinus tract, fluid or pus may drain from a small opening just anterior to the ascending portion of the helix ( Fig. 9.3 ). Most patients with preauricular cysts will have a history of recurrent infections.

The purported association of preauricular pits, accessory tragi, and sinuses with renal abnormalities is controversial. The most recent recommendations reserve renal ultrasound screening for patients with additional dysmorphic features, a family history of deafness, auricular and/or renal malformations, or a maternal history of gestational diabetes. Patients with preauricular pits or tags may have a higher incidence of hearing impairment, although studies regarding this are conflicting. Most studies do suggest screening for hearing deficits if the universal newborn hearing screen is not routinely performed.
The diagnosis is usually clinically apparent. The sinuses and cysts are lined by stratified squamous epithelium. Surgical excision of preauricular cysts and sinuses is indicated to prevent secondary infection. An experienced surgeon should perform the excision because the procedure may be complicated by multiple cysts along a tract that ends at the periosteum of the auditory canal.
The tragus is derived from the dorsal portion of the first branchial arch. Accessory tragi (erroneously referred to as preauricular ‘tags’) are always congenital and manifest as pedunculated, flesh-colored, soft, round papules usually arising on or near the tragus. They may occur anywhere from the preauricular region to the corner of the mouth, following the line of fusion of the mandibular and maxillary branches of the first branchial arch ( Fig. 9.4 ). They may be bilateral and/or multiple. The same hearing and renal screening recommendations discussed above regarding preauricular pits should be followed. Accessory tragi are usually isolated defects, but may be associated with other developmental abnormalities of the first branchial arch. Goldenhar syndrome (oculoauriculovertebral syndrome) manifests as epibulbar dermoids, vertebral anomalies, and accessory tragi ( Box 9.1 ).

The diagnosis is usually clinically apparent. Histologically, there are numerous tiny hair follicles with prominent connective tissue. A central core of cartilage is usually present. Accessory tragi should be removed by careful surgical dissection because most contain cartilage that may extend deeply, contiguous with the external ear canal. They are not skin tags and should not be tied off with suture material.
Cervical tabs are soft, pedunculated, irregular nodules occurring on the neck along the anterior border of the sternocleidomastoid muscle. They are thought to be remnants of branchial arches and tend to occur along branchial arch fusion lines ( Fig. 9.5 ). Histologically, they show lobules of mature cartilage embedded in collagen. The lesions do not extend deeply, but complete surgical excision is the treatment of choice because ligation may result in complications.

Supernumerary digits arise from the lateral surface of a normal digit. They are most common on the ulnar surface of the fifth digit, but may occur on any finger. They are congenital and may be bilateral or multiple. Some are small pedunculated papules, whereas others are normal-sized digits containing both cartilage and nail ( Fig. 9.6 ). These lesions should be surgically excised and the associated nerve dissected if present. Ligating the supernumerary digit with suture material without completely removing the nerve may result in skin necrosis, infection, and painful neuromas in adult life.

Branchial cysts are congenital malformations; however, they are not often apparent clinically until the first or second decade of life. They are painless, mobile, cystic swellings in the neck that may swell during respiratory tract infections. Most measure 1–2 cm, although they may be as large as 10 cm. Branchial cysts derived from the second branchial arch are the most common and are found on the lateral aspect of the upper neck, along the sternocleidomastoid muscle ( Fig. 9.7 ).
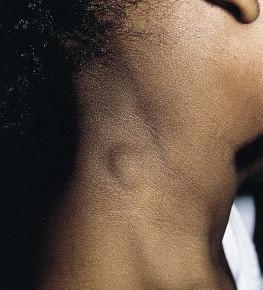
Branchial cleft cysts derived from the first branchial arch are very rare and are located in the periauricular area or on the upper neck anterior to the sternocleidomastoid muscle. Definitive diagnosis is made by histologic examination of the lesions. Branchial cysts are lined by stratified squamous epithelium or, rarely, by ciliated columnar epithelium. Additionally, there is often abundant lymphoid tissue. Squamous cell carcinomas arising in these cystic lesions have been described in adults.
Branchial sinuses and branchial clefts are thought to be remnants of the branchial cleft depressions. They are usually present at birth or noted during the first few years of life. The most common location is along the lateral lower third of the neck. Often a skin tag with a small amount of cartilage is associated with the pit. Branchial cleft anomalies should be surgically excised to prevent infection, with careful attention to the possibility of a true fistula connecting to the tonsillar oropharynx. Preoperative imaging may be necessary to exclude the possibility of true fistulae.
Thyroglossal duct cysts are the most common cause of a congenital neck mass. They result from the persistence of a tract formed during the migration of the rudimentary thyroid gland from the base of the tongue to the anterior cervical regions. The most common location is on, or just lateral to, the midline neck in the area of the hyoid bone, but they may be found anywhere from the posterior tongue to the suprasternal notch. Most thyroglossal duct cysts present in childhood as an asymptomatic neck mass that moves upward with tongue protrusion or swallowing. Occasionally, ectopic thyroid tissue can be found in these cysts, and an association with thyroid cancer has been reported. The treatment is complete surgical excision in order to prevent growth and infection. Preoperative imaging with high-resolution ultrasound is important to confirm the diagnosis and identify the presence of a normal thyroid gland.
Bronchogenic cysts are usually found within the chest or mediastinum but may also occasionally be found in the skin. The most common cutaneous location is in the subcutaneous tissue at the suprasternal notch, but other locations include the lateral neck, scapula, and presternal area. Thus, these cysts should be included in the differential diagnosis of both lateral and midline neck masses. The cysts are congenital and usually apparent at birth. They are asymptomatic, small cystic swellings that will gradually enlarge over time and may discharge a mucoid material. These lesions are not usually associated with other malformations and do not connect to underlying structures. The diagnosis is made by histologic examination of the nodule or sinus. Bronchogenic cysts are lined by lamina propria and a pseudostratified columnar ciliated epithelium with goblet cells. The cyst wall may contain smooth muscle, mucus glands, and cartilage and lymphatic tissue may or may not be present.
The differential diagnosis includes branchial arch cysts, thyroglossal duct cysts, teratomas, and heterotopic salivary gland tissue. The treatment is complete surgical excision to prevent infection.
Median raphe cysts (congenital sinus and cysts of the genitoperineal raphe, mucous cysts of the penile skin, parameatal cysts) are the consequence of incomplete fusion of the ventral aspect of the urethral or genital folds. The cysts can occur at any site on the ventral surface of the male genital region, including the parameatus, glans penis, penile shaft, scrotum, or perineum. In most cases they remain asymptomatic and do not interfere with urinary or sexual function. Rarely they can enlarge or become superinfected. In infancy they manifest as small, soft, flesh-colored papules along the ventral aspect of the penis in the line of the median raphe, however, they may enlarge during adolescence ( Fig. 9.8 ). The cysts are lined with pseudostratified columnar epithelium, except at the distal penis, where they have stratified epithelium.

Disruption of abdominal wall fusion causes midline defects of variable degree, often involving the heart and sternum, as well as the abdominal wall. Supraumbilical raphes are linear, midline clefts that occur superior to the umbilicus ( Fig. 9.9 ). A well-described association of supraumbilical raphe and/or sternal clefting has been described in association with hemangiomas and PHACE syndrome (see Chapter 21 ).

This rare abnormality of the midline ventral neck presents as a small skin tag superiorly with a linear, vertically oriented atrophic patch. At the inferior aspect of the patch there is often a small sinus containing ectopic salivary tissue. Midline cervical clefts can be associated with cleft lip, palate, mandible, chin, tongue, or midline neck hypoplasia. Excision with serial Z-plasties is the treatment of choice.
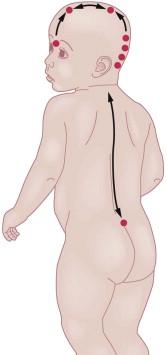
The skin and the nervous system share a common ectodermal origin. Separation of the neural and cutaneous ectoderm occurs early in gestation, at the same time the neural tube is fusing. This shared embryologic origin explains the simultaneous occurrence of congenital malformations of the skin and neural tube dysraphism, which is an incomplete closure or defective fusion. Open neural tube defects are often large and diagnosed in utero or at birth; however, closed or occult neural tube defects often present solely with congenital abnormalities of the skin overlying the defect. It is important to recognize these cutaneous markers and screen with the appropriate radiologic imaging techniques. A general knowledge of embryology and formation and closure of the neural tube is useful in identifying which cutaneous markers are highly indicative of underlying defects. The neural tube is no longer believed to fuse in a zipper-like fashion, but rather in a segmental, noncontiguous pattern. This theory is supported by the clinical observation of cutaneous ‘hotspots’ for dysraphic conditions. Each hotspot corresponds to a fusion point of the various segments of the neural tube ( Fig. 9.10 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here